It’s 2 a.m. again. Your mind won’t shut off. You’ve tried counting sheep, deep breathing, even that lavender spray - nothing works. So you reach for the bottle in the bathroom cabinet: a little white pill labeled "Sleep Aid." It’s easy. It’s over-the-counter. It’s been there for years. But is it really helping - or just making things worse?
What’s Actually in Those Sleep Pills?
Most OTC sleep aids fall into two camps: antihistamines and supplements. The antihistamines - like diphenhydramine (Benadryl, Sominex, Nytol) and doxylamine (Unisom SleepTabs) - were never meant to help you sleep. They were made for allergies. The drowsiness? That’s just a side effect. These drugs block histamine, a chemical in your brain that keeps you awake. When it’s blocked, you feel sleepy. Simple. But your body doesn’t care why you’re taking it. It just reacts. The other group is supplements: melatonin, valerian root, chamomile. Melatonin is the most popular. It’s a hormone your body naturally makes when it gets dark. Taking it as a pill tries to mimic that signal. But here’s the catch: supplements aren’t regulated like real medicine. A 2017 study found that melatonin pills contained anywhere from 83% less to 478% more than what’s on the label. That’s not a typo. One pill might have 0.2mg. Another, same brand, same box, could have 5mg. You’re guessing every time.How Much Do They Actually Help?
Let’s be honest: the benefit is tiny. Clinical trials show these pills help you fall asleep 3 to 13 minutes faster. They add 20 to 60 minutes of sleep total. For most people, that’s not life-changing. It’s barely noticeable. If you’re lying there for 90 minutes before nodding off, a 10-minute improvement doesn’t fix the real problem. And here’s the thing - they don’t improve sleep quality. You might fall asleep faster, but your deep sleep? Your REM cycles? Those stay broken. You wake up feeling like you didn’t rest at all. That’s why so many people say they feel groggy the next day. It’s not just "I’m tired." It’s a foggy, slow, off-balance feeling that lasts hours.The Hidden Risks - Especially for Older Adults
Antihistamine-based sleep aids are in a dangerous class called anticholinergics. These drugs interfere with acetylcholine, a brain chemical critical for memory and focus. Long-term use? That’s linked to higher dementia risk. A 2015 study tracked over 3,400 people for seven years. Those who took these pills regularly had a 54% higher chance of developing dementia. For people over 65, the risks are even worse. These drugs cause dizziness, blurred vision, and confusion. And that’s not just uncomfortable - it’s dangerous. One study found that older adults using diphenhydramine had a 50% higher risk of falling. Falls are the leading cause of injury-related death in seniors. That’s not a side effect. That’s a threat. The American Geriatrics Society says first-gen antihistamines like diphenhydramine are "potentially inappropriate" for anyone over 65. Yet millions still take them. Why? Because they’re cheap. Because they’re easy. Because no one told them the truth.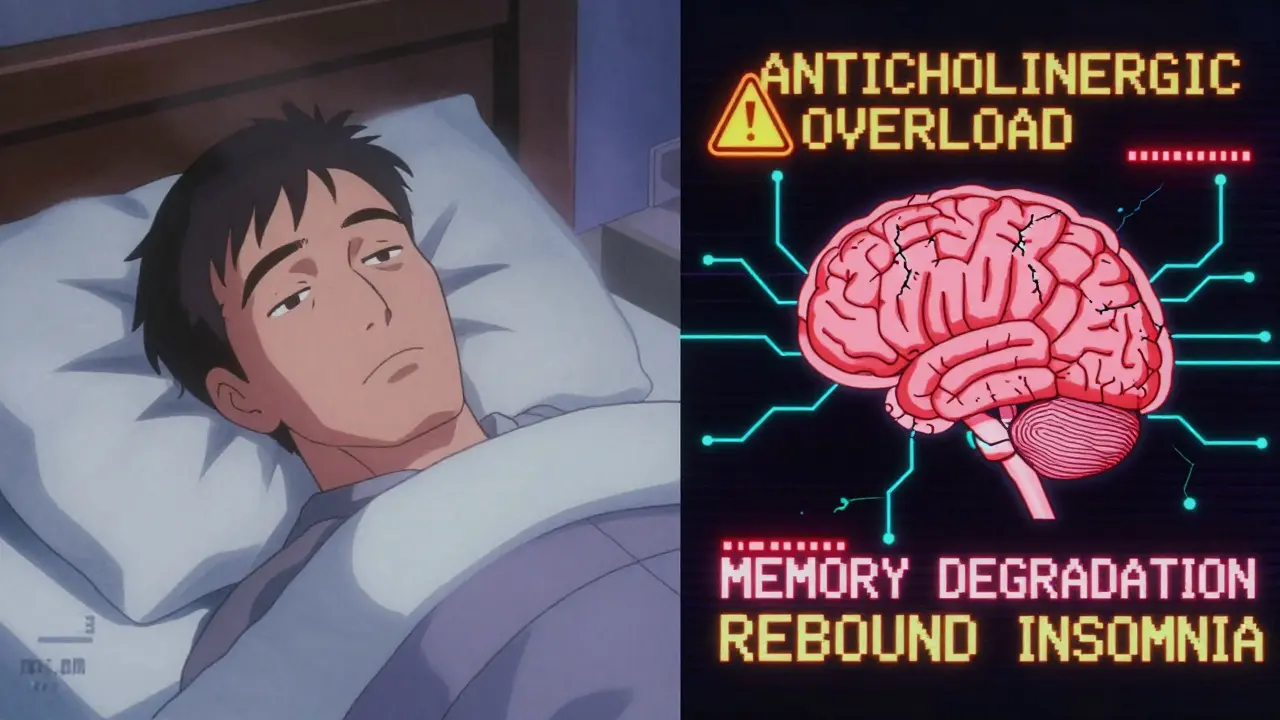
Melatonin Isn’t Harmless Either
People think melatonin is "natural," so it’s safe. But natural doesn’t mean harmless. High doses - 5mg or more - are common. But the European Food Safety Authority says 1mg is enough for most adults. Higher doses don’t help more. They just cause more side effects. Common issues? Daytime drowsiness (45% of users), vivid dreams or nightmares (68%), headaches (31%), dizziness (28%), nausea (19%), and even bedwetting in kids (8%). The NHS warns that melatonin can cause "pains in your arms or legs" - and if it doesn’t go away in a few days, you should stop. And here’s something few admit: melatonin can make insomnia worse over time. If you take it every night for more than 10 days, your body starts to rely on it. About 25% of daily users develop tolerance. Then, when they stop, their sleep crashes harder than before. That’s rebound insomnia. It hits 30% of people who use OTC sleep aids for over two weeks straight.Who Should Never Take These?
If you have sleep apnea, avoid them. These drugs relax your throat muscles. That makes breathing pauses during sleep worse. If you’re pregnant, skip them too. Diphenhydramine has limited safety data. Melatonin? Almost none. The NIH says it’s not recommended. If you’re on other meds - especially antidepressants, sedatives, or blood pressure drugs - talk to your doctor first. These pills can interact badly. And if you have an enlarged prostate, urinary problems, glaucoma, or asthma? Antihistamines can make those worse. Dry mouth? That’s common. But urinary retention? That’s serious. You might not be able to pee at all.
How Long Is "Safe" to Use Them?
The official advice? Two weeks. Max. That’s what the FDA says. That’s what the Cleveland Clinic says. That’s what the Sleep Foundation says. But here’s what actually happens: 38% of users go past two weeks. 19% use them for more than a month. Why? Because they think it’s harmless. Because they don’t know the risks. Because they’re desperate. If you’ve been taking it for more than 10 days and your sleep hasn’t improved? Stop. Don’t just quit cold turkey - but don’t keep going either. Talk to your doctor. Your insomnia isn’t a pill problem. It’s a pattern problem.What Should You Do Instead?
There’s a better way. Cognitive Behavioral Therapy for Insomnia, or CBT-I, is the gold standard. It’s not magic. It’s not a pill. It’s a set of tools: fixing your sleep schedule, learning to quiet your mind, changing habits that sabotage sleep. Studies show it works for 70-80% of people. And the results last. Unlike pills, it doesn’t wear off. It rewires your brain. You don’t need a therapist to start. Try these simple steps:- Go to bed and wake up at the same time every day - even on weekends.
- Get bright light in the morning. Walk outside for 15 minutes.
- Stop screens at least an hour before bed. Blue light kills melatonin production.
- Keep your bedroom cool, dark, and quiet. No TV. No phone.
- If you can’t sleep after 20 minutes, get up. Read a book under dim light. Don’t lie there stressing.
The Bottom Line
OTC sleep aids aren’t evil. Sometimes, they help - briefly. A night of jet lag? A stressful week? A single dose might get you through. But they’re not a solution. They’re a Band-Aid on a broken bone. The real problem isn’t that you can’t fall asleep. It’s that your body doesn’t trust nighttime anymore. Your brain is wired for stress, not rest. Pills don’t fix that. Behavior does. If you’ve been using OTC sleep aids for more than two weeks, you’re not alone. But you’re also not safe. The risks add up. The benefits fade. And the longer you wait to change, the harder it gets to break the cycle. You don’t need a miracle. You need a plan. And that plan doesn’t come in a bottle.Can I take OTC sleep aids every night?
No. Most OTC sleep aids are meant for short-term use only - no more than 7 to 10 days in a row, and never longer than two weeks. Using them nightly increases your risk of side effects like next-day drowsiness, confusion, and even long-term cognitive decline. It can also lead to rebound insomnia, where your sleep gets worse once you stop.
Is melatonin safer than antihistamine sleep aids?
Melatonin has fewer immediate side effects than antihistamines like diphenhydramine, but it’s not risk-free. High doses (above 1mg) can cause vivid dreams, dizziness, nausea, and daytime grogginess. It also lacks long-term safety data, especially for people over 65, pregnant women, or those with chronic conditions. Plus, because it’s not regulated, the actual dose in your pill may be wildly different from what’s on the label.
Why do OTC sleep aids make me feel groggy the next day?
Antihistamine-based sleep aids don’t just help you fall asleep - they linger in your system. Your body takes hours to break them down, so they’re still active when you wake up. This causes that heavy, foggy feeling. Melatonin can cause similar grogginess if taken too late or in too high a dose. Neither product improves sleep quality - they just push you into sleep faster, often without the restorative stages your brain needs.
Are OTC sleep aids addictive?
They’re not physically addictive like opioids or benzodiazepines. But your body can develop tolerance - meaning you need more to get the same effect. More importantly, you can become psychologically dependent. You start believing you can’t sleep without them. That’s why 30% of people who use them for more than two weeks experience rebound insomnia when they stop.
What’s the best alternative to OTC sleep aids?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective long-term solution. It helps you change the thoughts and habits keeping you awake. Studies show it works for 70-80% of people and the results last years. Simple habits like keeping a consistent sleep schedule, avoiding screens before bed, and getting morning sunlight also make a huge difference - and they’re free.