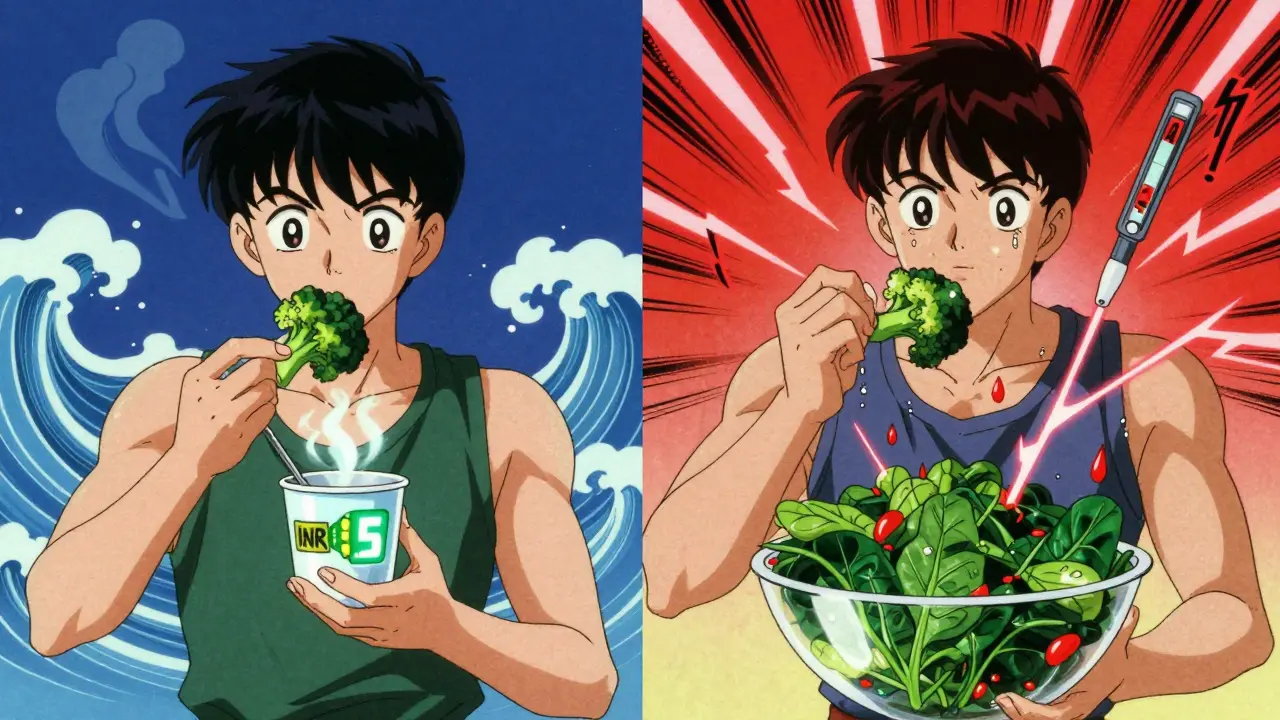
If you're on warfarin, your INR isn't just a number on a lab report-it's a daily balancing act between what’s in your medicine cabinet and what’s on your plate. One serving of kale can drop your INR from 2.8 to 1.9. A week of switching from spinach to iceberg lettuce can spike it to 4.1. That’s not a myth. That’s real, measurable, and dangerous if you don’t understand how vitamin K works with warfarin.
How Warfarin and Vitamin K Fight Over Your Blood
Warfarin doesn’t make your blood thinner by diluting it. It blocks a key enzyme called VKORC1, which your liver needs to recycle vitamin K. Without enough recycled vitamin K, your body can’t activate clotting factors II, VII, IX, and X. That’s how it prevents dangerous clots. But vitamin K-especially from food-fights back. It’s the fuel your body uses to make those same clotting factors. So when you eat more vitamin K, you’re giving your body more ammo to overcome warfarin’s effect. Less vitamin K? Warfarin works too well. Too much? It doesn’t work enough.The goal? Keep your INR between 2.0 and 3.0 for most people, or 2.5 to 3.5 if you have a mechanical heart valve. That’s the sweet spot where you’re protected from clots but not bleeding out. And the biggest thing you can control? Your daily vitamin K intake.
Which Foods Have the Most Vitamin K?
Not all greens are created equal. The American Heart Association says any food with more than 60 micrograms (mcg) of vitamin K per serving can affect your INR. Here’s what’s on the high end:- Cooked kale: 547 mcg per cup
- Cooked spinach: 889 mcg per cup
- Cooked collard greens: 773 mcg per cup
- Cooked broccoli: 220 mcg per cup
- Cooked Brussels sprouts: 219 mcg per cup
- Raw lettuce (iceberg): 17 mcg per cup
- Raw carrots: 16 mcg per cup
- Apples: 4 mcg per medium fruit
It’s not just about eating these foods. It’s about eating the same amount every day. One day you eat two cups of cooked spinach. The next day, you eat a salad with iceberg lettuce. That’s a 50-fold difference. Your INR will swing. And your doctor will have to adjust your warfarin dose. That’s not safe. That’s a rollercoaster.
Consistency Beats Restriction
For years, doctors told patients on warfarin to avoid vitamin K. That advice is outdated. The 2023 American College of Chest Physicians Guidelines now say: don’t cut vitamin K. Keep it steady.Why? Because if you suddenly eat a lot of vitamin K after weeks of eating almost none, your INR will crash. You’re at risk for a stroke or clot. If you suddenly eat almost no vitamin K, your INR will climb. You’re at risk for bleeding. Either way, you’re in the ER.
Studies show that people who keep their daily vitamin K intake within 10% of their normal amount have a 70% or higher Time in Therapeutic Range (TTR). People with inconsistent intake? Only 34% stay in range. That’s a 36-point gap. That’s the difference between staying out of the hospital and spending weeks in it.
It’s not about eating only low-vitamin K foods. It’s about eating the same high-vitamin K foods, the same amount, every day. If you love kale, eat one cup every day. If you hate it, eat none. But don’t flip-flop.
What About Cooking and Portion Size?
Cooking changes vitamin K levels. Boiling spinach for 10 minutes can knock out 30-50% of its vitamin K. Steaming? It keeps most of it. So if you usually eat steamed broccoli and suddenly switch to boiled, you’re changing your vitamin K intake without even realizing it.Portion size matters too. A “cup” of cooked greens isn’t just a handful. Use a measuring cup. A tablespoon of olive oil in your salad? That’s fine. A big bowl of raw spinach? That’s 145 mcg-enough to shift your INR if you’re not used to it.
Even sauces and dressings can sneak in vitamin K. Soy sauce, some salad dressings, and even certain types of margarine contain it. Read labels. Keep a food log. For the first two weeks, write down everything you eat and drink. Then look at your vitamin K totals. Adjust your meals to match your usual intake.
What About Supplements and Other Foods?
Vitamin K supplements? Don’t take them unless your doctor tells you to. Some people with unstable INR are prescribed 100-200 mcg of oral vitamin K daily to stabilize levels. But that’s a medical decision, not a DIY fix.What about vitamin K2? Found in fermented foods like natto, cheese, and egg yolks. It’s less studied than K1, but it still affects warfarin. If you eat natto daily, your doctor needs to know. If you never eat it, don’t start.
Green tea? It can interfere with warfarin metabolism. Alcohol? It can increase bleeding risk. Cranberry juice? It can raise INR. Avocados? High in vitamin K-about 21 mcg per half. Not a problem if you eat it regularly. A problem if you eat it once a week.
Real People, Real Stories
On Reddit’s r/bloodthinners, one user wrote: “I ate a big bowl of kale after a week of salads. My INR dropped from 2.8 to 1.9 in three days. My doctor increased my warfarin by 2 mg. I was scared I’d clot.”Another said: “I switched from spinach to romaine because I thought it was ‘healthier.’ My INR went from 2.3 to 4.1. I had a nosebleed that wouldn’t stop. They gave me vitamin K in the ER.”
But then there’s the success story: a woman in Ohio ate exactly one cup of cooked broccoli every single day for six months. Her TTR hit 92%. She didn’t change her warfarin dose. She didn’t go to the ER. She just kept it consistent.
Tools to Help You Stay on Track
You don’t have to guess. There are tools:- CoumaDiet (iOS/Android): Tracks vitamin K in over 1,000 foods. Rated 4.6/5 by over 1,200 users.
- Food logs: Write down meals. Use a measuring cup. Take a photo. Do this for two weeks. Then find your average daily vitamin K.
- Registered dietitians: 72% of U.S. anticoagulation clinics have one on staff. Ask your clinic for a referral.
- Weekly INR checks: Don’t skip them. Even if you feel fine. Your INR can change without symptoms.
Some clinics now use AI tools that predict your INR based on your food log. Mayo Clinic’s system is 89% accurate in early tests. It’s not perfect. But it’s better than guessing.
When You Eat Out or Travel
Restaurant meals are the #1 cause of INR spikes and crashes. You don’t know what’s in the salad. You don’t know if the broccoli was boiled or steamed. You don’t know if the chef added spinach to your soup.Plan ahead. Call the restaurant. Ask: “What greens are in the salad?” “Is the broccoli steamed or boiled?” “Do you use spinach in the omelets?”
Travel? Pack your own snacks: apples, carrots, rice cakes. Bring your measuring cup. Stick to your routine. Don’t try new foods. Don’t drink unfamiliar juices. Stick to water.
One survey found 63% of warfarin users had an emergency visit after eating inconsistently while traveling. That’s avoidable.
What If You Can’t Stick to It?
If you’re struggling, talk to your doctor. You’re not failing. The system is hard. But there’s help.Some patients do better with daily low-dose vitamin K (150 mcg). A 2022 study in Blood Advances showed it cut INR swings by 28%. It’s not a cure. But it’s a buffer. It smooths out the bumps when your diet slips.
There’s also a new clinical trial (NCT05123489) testing vitamin K-fortified foods-like bread or yogurt-with standardized amounts. It’s still in testing. But it could be a game-changer.
For now, your best tool is consistency. Not perfection. Not restriction. Just the same amount, every day.
What About DOACs? Are They Better?
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban don’t interact with vitamin K. That’s why they’re popular. But they’re not for everyone.Warfarin is still the first choice for:
- People with mechanical heart valves (98% use warfarin)
- People with antiphospholipid syndrome (87% use warfarin)
- People with severe kidney disease
DOACs aren’t approved for these groups. So if you’re on warfarin, you’re not stuck with outdated care. You’re in a group that still needs this tool-and vitamin K management is the key to using it safely.
The American Heart Association says warfarin will remain essential for at least the next 15 years. That means learning how to manage vitamin K isn’t optional. It’s part of your treatment.
Can I eat leafy greens while on warfarin?
Yes, but only if you eat the same amount every day. A cup of cooked spinach or kale is fine if you have it daily. Switching between high and low vitamin K foods causes dangerous INR swings. Consistency is more important than avoidance.
Does cooking reduce vitamin K in vegetables?
Yes, boiling can reduce vitamin K by 30-50%, especially in spinach and kale. Steaming preserves most of it. If you usually eat steamed broccoli, don’t switch to boiled without telling your doctor. Even small changes can affect your INR.
Should I take vitamin K supplements to stabilize my INR?
Only if your doctor prescribes it. Taking supplements without medical guidance can make your INR unstable. Some patients with erratic diets are given 150 mcg daily to smooth out fluctuations-but this is a controlled treatment, not a DIY fix.
Why do I need to check my INR every month?
Because your vitamin K intake can change without you noticing-through new foods, restaurants, or even cooking methods. INR checks catch these shifts before they cause bleeding or clots. Monthly monitoring is standard care for warfarin users.
Can I switch from warfarin to a DOAC to avoid diet restrictions?
Maybe, but not always. DOACs don’t interact with vitamin K, but they’re not approved for people with mechanical heart valves or certain clotting disorders. Warfarin is still the only option for many. Talk to your doctor before making any changes.
What’s the best way to track my vitamin K intake?
Use a food-tracking app like CoumaDiet or keep a written log with portion sizes measured in cups. Track for two weeks to find your average daily intake. Then aim to stay within 10% of that number every day. Consistency beats perfection.
Next Steps
Start today. Don’t wait for your next INR check.- Check your last INR result. Is it in range?
- Look at your last week of meals. Did you eat different greens every day?
- Pick one high-vitamin K food you like (kale, broccoli, spinach). Decide to eat the same amount every day.
- Download CoumaDiet or start a food log. Track for 14 days.
- Ask your clinic if they have a dietitian who works with warfarin patients.
You don’t need to be perfect. You just need to be consistent. That’s the only thing that keeps your INR stable, your blood flowing right, and you out of the hospital.


Fabio Raphael
December 25, 2025 AT 05:11Just wanted to say this is one of the clearest explanations I’ve ever read on warfarin and vitamin K. I’ve been on it for 8 years and no one ever broke it down like this. Seriously, thank you.
My INR used to swing like a pendulum until I started eating exactly one cup of steamed broccoli every day. No more guessing. No more panic calls to my anticoagulation clinic.
Consistency isn’t sexy, but it saves lives.
Nikki Brown
December 26, 2025 AT 05:07Wow. Just… wow. People still don’t get it. You don’t ‘avoid’ vitamin K-you treat it like a medication. If you can’t commit to eating the same amount of greens every day, maybe you shouldn’t be on warfarin. It’s not that hard. It’s just inconvenient for people who think kale is a ‘trend’ and not a life-saving tool.
Also, stop eating ‘healthier’ lettuce. Romaine isn’t safer. It’s just less predictable. And that’s dangerous.
Amy Lesleighter (Wales)
December 26, 2025 AT 16:16i just eat one cup of spinach every day. no big deal. my inr is perfect. no drama. no apps. no stress. if you make it complicated, you’ll mess it up. keep it simple. same food. same amount. done.
ps: stop listening to people who say ‘just avoid greens.’ they dont know what they’re talking about.
roger dalomba
December 27, 2025 AT 06:13So… you’re telling me I can’t just eat a kale smoothie every morning and call it a day? What a surprise. Next you’ll say smoking is bad for your lungs.
Anyway, congrats on writing a 2,000-word essay on salad. I’m sure the FDA is taking notes.
Peter sullen
December 28, 2025 AT 08:39Thank you for this meticulously researched, clinically grounded, and patient-centered exposition on the critical interplay between dietary vitamin K and anticoagulant efficacy.
As a certified anticoagulation specialist with over 15 years of clinical experience, I can affirm that the 70% TTR improvement associated with consistent vitamin K intake is not merely statistically significant-it is clinically transformative.
Further, the integration of AI-driven predictive modeling, as referenced from Mayo Clinic, represents a paradigm shift in personalized anticoagulation management. This is the future-and it’s here.
Sophia Daniels
December 29, 2025 AT 12:33OMG I’m so mad right now. I ate a giant salad with spinach and kale after being on iceberg for a month. My INR went to 4.1. I bled out of my nose for 20 minutes. My husband had to hold a towel to my face while I cried. And then my doctor just shrugged and said ‘you should’ve known.’
But guess what? I’m not dumb. I just didn’t know. And now I know. And I’m never eating another leafy green unless I measure it with a cup.
Also, I hate kale. It’s overrated. And so are people who act like it’s a virtue to eat it every day.
Steven Destiny
December 30, 2025 AT 14:23Look, I get it. This is hard. But you’re not failing. You’re fighting a system that makes you count every spinach leaf like it’s a calorie. That’s not fair.
But here’s the thing-you can do this. I did. I ate one cup of broccoli every day for 11 months. No apps. No logs. Just… I remembered. And my INR never budged.
You got this. Don’t quit. You’re not alone.
Erwin Asilom
December 31, 2025 AT 02:04Consistency over perfection. This is the mantra. I’ve worked with hundreds of patients on warfarin. The ones who track their intake-even just with a notebook-are the ones who stay out of the ER.
Don’t overcomplicate it. Pick one food. Stick to it. Measure it. Do it daily. That’s it.
And if you travel? Pack apples. They’re safe. And they don’t judge you.
Sumler Luu
January 1, 2026 AT 03:19Thank you for writing this. I’ve been scared to eat anything green since I started warfarin. But this makes sense now. I’m not going to stop eating vegetables. I’m just going to eat the same ones, the same way, every day.
I’m going to start with carrots. They’re easy. And I like them.
sakshi nagpal
January 2, 2026 AT 14:32As someone from India, I never realized how much this applies globally. My aunt on warfarin used to eat curry with lots of coriander and spinach. Her INR was always out of range. Now she eats one cup of boiled spinach every Tuesday and Friday. Her numbers are stable.
Consistency works everywhere. Not just in the US.
Sandeep Jain
January 3, 2026 AT 08:08i read this and i cried. my mom died because she ate a big bowl of kale after a week of only rice. her inr was 5.2. no one told her. no one warned her. i wish i had this article 5 years ago.
thank you for writing this. i’m sharing it with everyone i know.
Brittany Fuhs
January 4, 2026 AT 12:54Of course the American Heart Association says this. They’re funded by pharma. They want you to stay on warfarin so you keep buying blood tests and apps. DOACs are better. Period.
But since you’re stuck with warfarin, at least don’t be a nutrition idiot. Eat the same damn spinach every day. Or get off it.
Becky Baker
January 5, 2026 AT 04:14My husband is on warfarin. I used to make him salads with kale, spinach, arugula, and quinoa. Now? I give him one cup of steamed broccoli and a banana. He hasn’t had an INR scare in 14 months.
It’s not about being healthy. It’s about being smart.
Rajni Jain
January 6, 2026 AT 07:46i started using coumadiet last month. i eat one cup of cooked collard greens every day. my inr is 2.4. i’m so proud. i used to think i had to give up greens forever. turns out i just had to be boring. and it worked.
ps: i love my collards. they taste like home.