Spina Bifida Detection Guide
Lemon Sign
A scalloped frontal bone resembling a lemon in midsagittal view.
Banana Sign
Curved cerebellum appearing like a banana indicating posterior fossa abnormalities.
Ultrasound can detect early signs of spina bifida as early as 12-14 weeks during the first trimester. Definitive views usually occur around 18-22 weeks during the anatomy scan.
| Feature | Ultrasound | Fetal MRI |
|---|---|---|
| Timing of Detection | 12-14 weeks (early markers) | 20-24 weeks (optimal detail) |
| Key Signs | Lemon & Banana signs, spinal defect | Level of lesion, brain malformations |
| Safety | No radiation exposure | Safe, no ionizing radiation |
| Accessibility | Widely available | Limited to specialized centers |
Estimate your risk based on key factors:
Key Takeaways
- Ultrasound is the first‑line tool for spotting spina bifida as early as 12‑14 weeks.
- Typical ultrasound signs include the "lemon sign" of the skull and the "banana sign" of the cerebellum.
- Fetal MRI adds detail when ultrasound findings are unclear or when the pregnancy is beyond the second trimester.
- Maternal serum AFP and detailed anatomy scans together raise the detection rate above 90%.
- Early detection opens the door to fetal surgery, targeted counseling, and optimal post‑natal care.
What Is Spina Bifida?
Spina bifida is a neural tube defect (NTD) where the spine and spinal cord do not close completely during the first month of embryonic development. It can range from mild (spina bifida occulta) to severe forms that involve the brain (myelomeningocele). Incidence in the UK is roughly 1 in 1,000 live births, but early prenatal detection can dramatically improve outcomes.
How Ultrasound Works in Prenatal Screening
The first imaging modality used in pregnancy is the ultrasound a non‑invasive sound‑wave technique that creates real‑time images of the fetus
Standard practice includes a dating scan at 8‑10 weeks, a nuchal translucency (NT) scan at 11‑14 weeks, and an anatomy scan at 18‑22 weeks. During the anatomy scan, the sonographer evaluates the cranial vault, spine, and limbs for any abnormal patterns.
Key sonographic markers for spina bifida:
- "Lemon sign" - a scalloped frontal bone resembling a lemon, visible in the midsagittal view.
- "Banana sign" - a curved cerebellum that looks like a banana, indicating posterior fossa abnormalities.
- Reduced or absent intracranial cisterns.
- Direct visualization of a spinal defect, especially in open myelomeningocele.
These signs can appear as early as the first trimester, allowing a provisional diagnosis before the 14‑week mark.
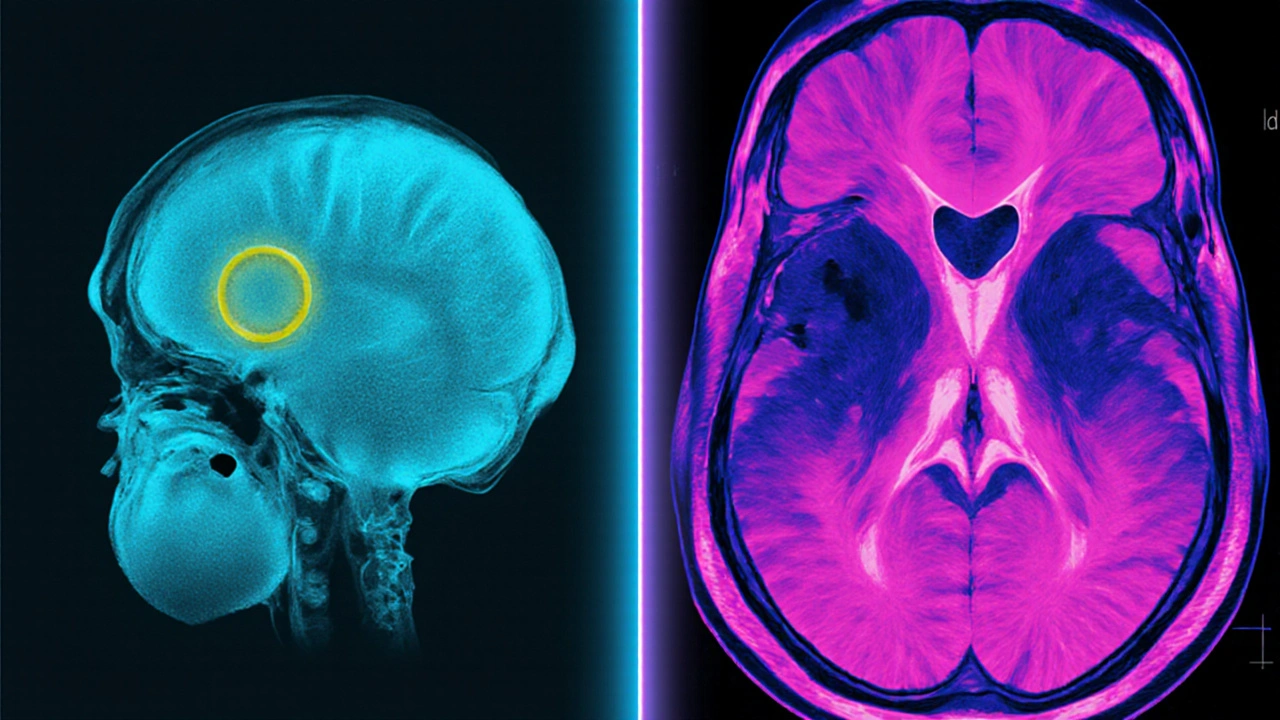
When Ultrasound Isn’t Enough - The Role of Fetal MRI
In about 10‑15% of cases, the ultrasound image is limited by fetal position, maternal habitus, or low‑grade acoustic windows. That’s where fetal magnetic resonance imaging (MRI) a high‑resolution imaging technique that uses magnetic fields to capture detailed anatomy without ionizing radiation
MRI excels at delineating the spinal cord, level of the defect, and associated brain malformations such as ventriculomegaly. It also helps the multidisciplinary team decide whether in‑utero repair is feasible.
Typical MRI protocol includes T2‑weighted single‑shot fast spin‑echo sequences in three orthogonal planes. The exam takes about 30‑45 minutes and can be performed safely after the 20‑week gestation mark.
Complementary Tests: Serum AFP and Amniocentesis
Ultrasound does not work in isolation. Maternal serum alpha‑fetoprotein (AFP) is a protein produced by the fetal liver; elevated levels in the second trimester suggest open neural tube defects.
When AFP is high, the next step is often an amniocentesis a procedure that withdraws a small amount of amniotic fluid for laboratory analysis. The fluid can be tested for AFP and acetylcholinesterase, both of which are more specific for spina bifida. Genetic analysis (e.g., karyotype, microarray) may also be performed to rule out chromosomal abnormalities that sometimes accompany NTDs.
Risk Factors and Prevention
Understanding why spina bifida occurs helps clinicians advise families on prevention. Major risk factors include:
- Maternal diabetes - poorly controlled blood sugar raises NTD risk by up to 60%.
- Low intake of folic acid a B‑vitamin essential for DNA synthesis and neural tube closure before conception. The UK recommends 400µg daily; higher doses (5mg) are advised for high‑risk women.
- Obesity, certain antiepileptic drugs, and a family history of NTDs.
Public health campaigns in Britain have increased periconceptional folic acid supplementation to over 70% of women of childbearing age, trimming NTD rates by roughly 15% over the past decade.
Management After a Prenatal Diagnosis
Once spina bifida is confirmed, the care pathway branches based on severity, gestational age, and parental choice.
- Fetal surgery - for selected cases of open myelomeningocele, a prenatal repair (usually between 19‑26 weeks) can improve motor outcomes and reduce the need for shunting.
- Post‑natal surgery - closure of the defect shortly after birth remains the standard for many infants.
- Multidisciplinary counseling - neonatology, neurosurgery, orthopedics, and pediatric rehab teams meet with parents to set realistic expectations.
- Delivery planning - most babies are delivered by scheduled cesarean at a tertiary centre equipped for neonatal intensive care.
Long‑term follow‑up involves monitoring for hydrocephalus, orthopedic deformities, and neurodevelopmental milestones.

Ultrasound vs. MRI: Quick Comparison
| Feature | Ultrasound | Fetal MRI |
|---|---|---|
| Timing of first reliable detection | 12‑14 weeks (first‑trimester markers) | 20‑24 weeks (optimal image quality) |
| Key visual signs | Lemon & banana signs, spinal defect | Exact level of lesion, associated brain malformations |
| Safety | Established safety, no radiation | Safe (no ionizing radiation), but limited availability |
| Cost & accessibility | Widely available, low cost | Higher cost, requires specialist centre |
| Impact on management decisions | Initial diagnosis, guides need for further testing | Refines surgical planning, determines candidacy for fetal repair |
Common Questions Parents Ask
- Can we see spina bifida on a routine 20‑week scan? - Yes, most structural defects are visible, especially with a skilled sonographer.
- Is the ultrasound harmful to the baby? - No. Diagnostic ultrasound uses low‑intensity sound waves and is considered safe throughout pregnancy.
- What are the chances of a successful fetal surgery? - Studies from the MOMS trial show a 40‑50% reduction in the need for shunting and better motor outcomes.
- Will my baby need lifelong care? - Many children lead active lives, but ongoing monitoring for hydrocephalus and orthopaedic issues is typical.
- How can I lower my risk in future pregnancies? - Take 400µg folic acid daily before conception, control diabetes, maintain a healthy weight, and discuss medication adjustments with your doctor.
Key Points to Remember
- Early ultrasound screening (first trimester) can flag spina bifida before many other anomalies appear.
- Combine imaging with maternal serum AFP for the highest detection rate.
- When ultrasound is equivocal, fetal MRI provides decisive detail.
- Preventive folic acid supplementation remains the single most effective strategy to reduce incidence.
- Timely diagnosis expands treatment options, from fetal surgery to tailored post‑natal care.
Frequently Asked Questions
How early can spina bifida be detected with ultrasound?
The first‑trimester scan at 12‑14 weeks can reveal indirect markers such as the lemon sign. A definitive view of the spinal defect often becomes clear at the 18‑22‑week anatomy scan.
What does a high maternal serum AFP mean?
Elevated AFP suggests an open neural tube defect like spina bifida. It prompts a targeted ultrasound and possibly an amniocentesis for confirmatory testing.
Is fetal MRI safe for the baby?
Yes. MRI uses magnetic fields and radio waves, not ionizing radiation. It is considered safe after the first trimester, especially when performed at experienced centers.
Can spina bifida be cured before birth?
In‑utero repair can close the open lesion for selected cases, reducing neurological complications. However, it does not ‘cure’ the condition; long‑term monitoring is still required.
What lifestyle steps lower the risk of spina bifida?
Take 400µg folic acid daily before conception, manage diabetes tightly, achieve a healthy BMI, and avoid teratogenic medications without medical guidance.


Alex Bennett
October 5, 2025 AT 17:27First off, the lemon and banana signs are like the secret handshake of fetal ultrasound – if you spot them, you’ve basically unlocked the early detection level. It’s wild how a simple midsagittal view can give you a heads‑up on something as serious as spina bifida before most people even think about a coffee break. The timing numbers (12‑14 weeks for first‑trimester markers, 18‑22 weeks for a solid anatomy scan) are not just stats; they’re the window where intervention options start to become real choices. And yes, the safety profile of ultrasound is solid – no radiation, just sound waves bouncing around, which makes it a go‑to for most obstetric clinics worldwide.
Mica Massenburg
October 14, 2025 AT 10:39While everyone’s raving about the clarity of the lemon sign, you have to wonder who’s really pulling the strings behind the scenes – why do we only get full access to high‑resolution images after the 20‑week mark? It feels like a coordinated effort to keep the public in the dark until it’s too late for any meaningful choice. And don’t even get me started on the “widely available” claim for ultrasound; many rural clinics can’t even guarantee a decent probe, let alone a skilled sonographer who can spot those subtle cues. There’s definitely more to the story than what the glossy charts want us to believe.
Sarah Brown
October 23, 2025 AT 03:51Let’s break this down step by step, because the information here is crucial for anyone navigating a pregnancy complicated by spina bifida. First, the early detection window of 12‑14 weeks offers a chance for parents to understand the condition well before the anatomy scan, which typically occurs between 18‑22 weeks. This early insight is not merely academic; it opens doors to prenatal counseling, which can dramatically influence decision‑making and mental preparation. Second, the lemon and banana signs, while seemingly simple visual cues, are backed by extensive research linking them to neural tube defects, making them reliable markers when interpreted by an experienced sonographer.
Third, the integration of maternal serum AFP testing creates a powerful two‑pronged approach. Elevated AFP levels act as a biochemical flag that prompts a more detailed ultrasound, increasing overall detection rates above 90 percent. Fourth, when ultrasound images are suboptimal – due to fetal position, maternal habitus, or limited acoustic windows – fetal MRI steps in as a high‑resolution adjunct, delineating the exact level of the spinal lesion and any associated brain malformations. This is critical for surgical planning, especially if in‑utero repair is being considered.
Fifth, let’s not overlook the preventive side: periconceptional folic acid supplementation remains the single most effective public‑health measure to reduce the incidence of neural tube defects. Studies consistently show that 400 µg daily, or a higher dose for high‑risk groups, can lower spina bifida rates by up to 70 percent. Sixth, the multidisciplinary team approach – involving obstetricians, fetal medicine specialists, neurosurgeons, and neonatal intensive care teams – ensures that parents receive comprehensive counseling covering surgical options, potential neurodevelopmental outcomes, and long‑term care considerations.
Seventh, for families eligible for fetal surgery, the evidence from the MOMS trial indicates a substantial reduction in the need for postnatal shunting and improvements in motor outcomes. However, it’s essential to balance these benefits against the risks of preterm birth and maternal complications associated with the procedure.
Eighth, postnatal management should not be overlooked. Even after successful repair, close monitoring for hydrocephalus, orthopedic issues, and neurodevelopmental milestones is essential. Lastly, the emotional and psychological support for families throughout this journey cannot be overstated; ongoing counseling and support groups play a vital role in coping with the complexities of spina bifida.
In summary, the combination of early ultrasound markers, biochemical screening, advanced imaging, preventive folic acid supplementation, and multidisciplinary care creates a comprehensive framework that maximizes detection, informs treatment options, and ultimately improves outcomes for both the child and the family.
Max Canning
October 31, 2025 AT 20:03Yo, this guide is exactly what you need when you’re staring at those ultrasound screens and wondering if that weird shape is a lemon or just a weird artifact. The energy in the first‑trimester scan is insane – you get that early heads‑up and can start planning, whether it’s bringing in a specialist or just getting your mind right. And the way they broke down the lemon and banana signs keeps it simple enough for anyone to remember, even if you’re not a medical pro. Plus, the MRI part? Total game‑changer when the ultrasound can’t give you the full picture. Keep those folic acid pills popping, and you’ll be doing the right thing before you even know you need to.
Nick Rogers
November 9, 2025 AT 13:15Excellent overview; concise, clear, and well‑structured, providing essential information efficiently.
Tesia Hardy
November 18, 2025 AT 06:28Hey there! I just wanted to say that this whole spina bifida detection thing is super important, and I think the guide does a great job of breaking it down. The lemon and banana signs are kinda funny names, but they actually mean a lot when you’re looking at a baby’s brain. Also, don’t forget to take your folic acid – it’s easy to miss, especially when you’re busy with work and stuff. If you ever feel unsure about a scan, just ask the sonographer to explain what they see. We all need a little help sometimes, right? Stay positive and keep informed!
Matt Quirie
November 26, 2025 AT 23:40Thank you for the detailed guide; it provides a comprehensive overview of ultrasound and MRI modalities, emphasizing safety, accessibility, and the impact on clinical decision‑making while maintaining a respectful and informative tone.
Pat Davis
December 5, 2025 AT 16:52From a cultural perspective, it is essential to recognize how prenatal screening practices differ worldwide, yet the fundamental principles-early detection, informed consent, and equitable access-remain universal. This guide adeptly balances technical detail with sensitivity to diverse patient experiences, reinforcing the importance of culturally competent counseling when discussing conditions such as spina bifida.
Mary Wrobel
December 14, 2025 AT 10:04Wow, the science behind the lemon and banana signs is like a secret language between doctors and babies – a real peek‑a‑boo of the future! It’s amazing how early we can spot issues, and the way the article breaks down the timelines makes it super easy to follow. I’m especially impressed by the comparison table; seeing the pros and cons side by side really paints a clear picture. And let’s not forget the power of folic acid – that little pill truly works like a superhero cape for expecting moms. Great read, folks, keep the info flowing!
Lauren Ulm
December 23, 2025 AT 03:16Isn't it fascinating how the medical community keeps dropping new tech while the big players keep us in the dark about the real risks? 🤔 The lemon sign might look innocent, but who's to say the data isn't being filtered? And those MRI machines? Definitely a fancy way to keep control over what we actually see. 🌐 Keep questioning the narrative, stay curious! 🌱
Michael Mendelson
December 31, 2025 AT 20:28Honestly, this whole guide feels like it's trying too hard to be "helpful" while letting the jargon slide in. The lemon and banana references are cute, but the underlying complexity gets glossed over. You need a real deep dive, not just a surface skim of tables. Also, the mention of folic acid is over‑simplified – it's not a one‑size‑fits‑all miracle. If you're looking for substance, dig beyond the bullet points and ask the experts who actually write the protocols.
Ibrahim Lawan
January 9, 2026 AT 13:40Reflecting on the intricacies of prenatal imaging, it becomes evident that early ultrasound screening is not merely a diagnostic step but a profound philosophical act – it bridges uncertainty with knowledge, granting families agency in the face of potential adversity. The convergence of sonographic markers, biochemical assays, and advanced MRI illustrates a harmonious interplay of technology and human insight, underscoring the ethical imperative to provide clear, compassionate counsel. As we champion folic acid supplementation, we also honor the collective responsibility to disseminate preventive measures across diverse populations, ensuring equitable access to the benefits of early detection. Ultimately, this guide serves as both an informative resource and a reminder of our shared commitment to nurture life with both scientific rigor and empathetic care.