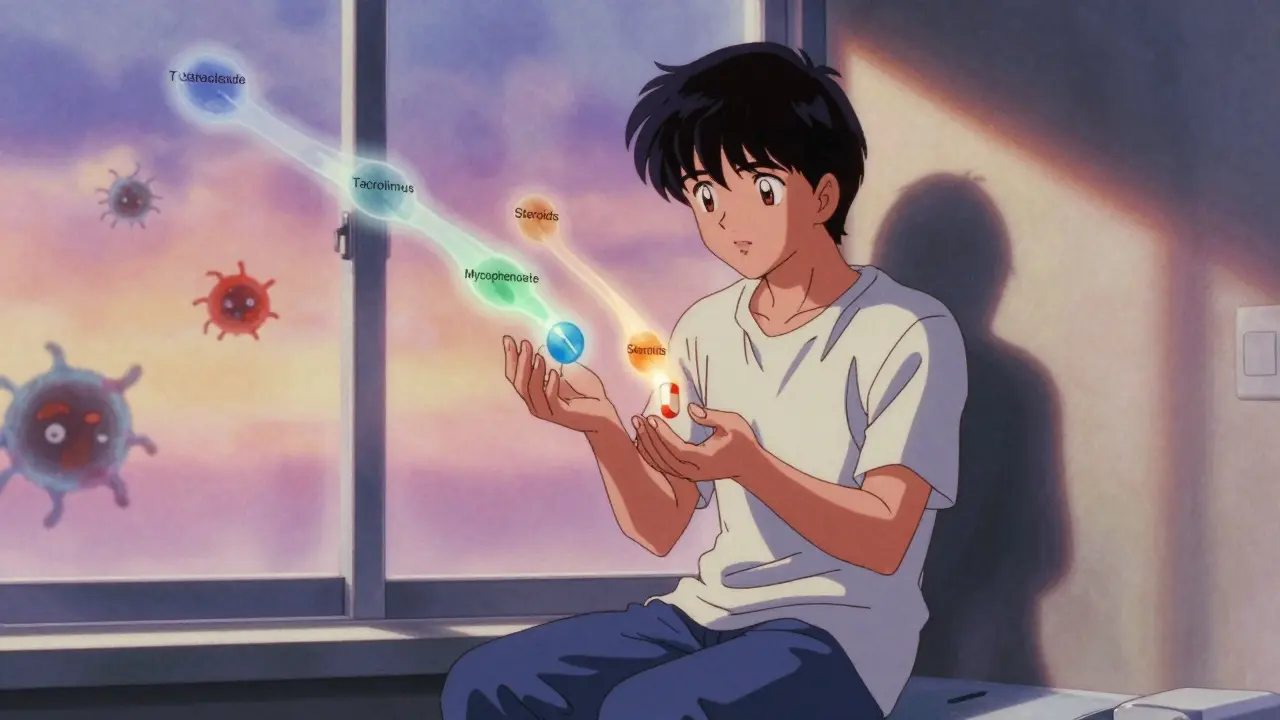
After a kidney transplant, your body doesn’t know the new organ isn’t a threat. It sees it as an invader and tries to attack it. That’s where tacrolimus, mycophenolate, and steroids come in. Together, they form the most common immunosuppression plan used worldwide for kidney transplant patients. This isn’t just a random combo-it’s the result of decades of research, trial, and refinement. Since the mid-1990s, this triple-drug approach has become the gold standard. But it’s not perfect. It saves lives, yes, but it also brings side effects that change how you live every day.
Why This Triple Drug Combo Exists
Before tacrolimus and mycophenolate, transplant patients mostly took cyclosporine. It worked, but not well enough. About 21% of patients still had acute rejection within the first year. That’s a lot of people losing their new kidney. Then came tacrolimus-more powerful, with fewer cosmetic side effects like tremors and excess hair growth. Mycophenolate joined next, blocking a key pathway immune cells need to multiply. Steroids? They’re the old-school fire extinguisher, dousing inflammation fast. Together, they cut rejection rates down to just 8.2%. That’s a 61% drop. It’s not magic, but it’s close.
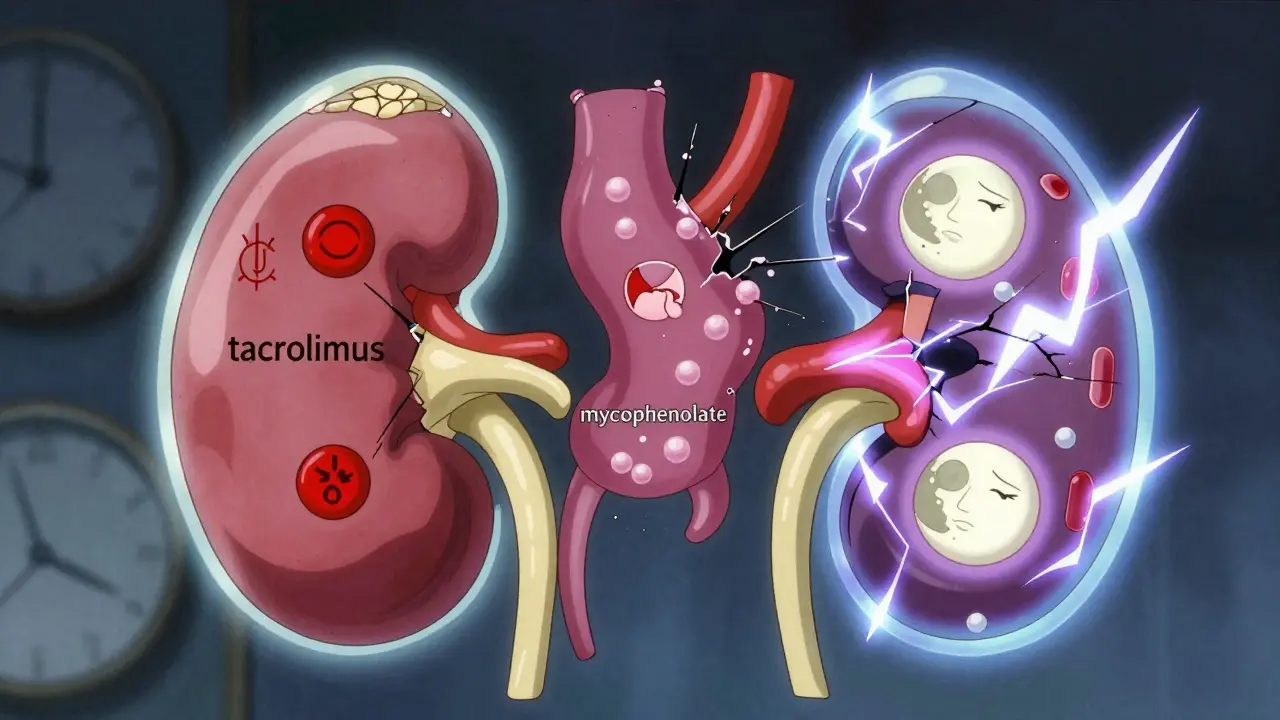
Think of it like a three-layer security system. Tacrolimus stops T-cells from activating. Mycophenolate cuts off their food supply. Steroids shut down the whole alarm system. Alone, each has gaps. Together, they cover each other’s blind spots.
How Each Drug Works
Tacrolimus is a calcineurin inhibitor. It’s taken twice daily, usually in the morning and evening. It hits the bloodstream in under an hour, but its real job is to stay steady. Doctors aim for a blood level between 5 and 10 ng/mL in the first year. Too low? Rejection risk goes up. Too high? You risk kidney damage, shaking hands, or even diabetes. It’s a tightrope walk. About 18-21% of patients develop new-onset diabetes after transplant because of it. That’s not rare-it’s expected.
Mycophenolate mofetil (MMF) is the workhorse. It’s taken as 1 gram twice a day, usually with meals. But here’s the catch: it doesn’t play nice with your stomach. About 25-30% of people get bad diarrhea. Another 15% develop low white blood cell counts, making infections more likely. Many end up cutting their dose to 500 mg twice daily-or stopping it entirely. The good news? It’s one of the best predictors of long-term graft survival. If you can stay on it, your kidney lasts longer.
Steroids (usually prednisone or methylprednisolone) start strong. Right in the operating room, you get 1,000 mg intravenously. Then, over the next few weeks, it’s slowly turned down. By week 3-4, you’re on 15 mg a day. By 2-3 months, it’s 10 mg. That’s the plan. But steroids bring weight gain, acne, mood swings, and brittle bones. Many patients say the cosmetic side effects are worse than the surgery. That’s why some centers now try to ditch them entirely after the first few weeks.
What You’ll Actually Experience
You won’t feel the drugs working. That’s the point. But you’ll feel the side effects.
- Diarrhea that comes and goes? That’s MMF.
- Feeling hungrier than usual, gaining weight around your middle? That’s the steroids.
- Headaches, tingling in your fingers, or trouble sleeping? That’s tacrolimus.
- Getting sick more often? Your immune system is turned down too far.
Some people manage fine. Others can’t tolerate even half the dose. That’s why dose adjustments aren’t a failure-they’re part of the process. One patient I spoke with (in a transplant support group) said she went from 1,000 mg of MMF twice daily to 500 mg, and her diarrhea vanished. Her doctor didn’t see it as giving up. He saw it as adjusting for her body.
Timing matters too. Tacrolimus and MMF are often spaced 2-4 hours apart. Why? Because they compete for the same gut enzymes. Take them together? You might absorb less of both. That’s not just advice-it’s science.
The Steroid Debate
For years, everyone assumed steroids were necessary. Then came a 2005 study that changed everything. Researchers gave one group the full triple therapy. Another group skipped steroids but added a short course of daclizumab (an induction drug). Guess what? Both groups had the same rejection rate: 16.5%. No difference.
That’s huge. It means steroids aren’t always needed. And in 88.8% of patients who skipped them, they stayed steroid-free at six months. No weight gain. No moon face. No mood crashes. That’s the future many doctors are pushing toward: steroid minimization.
But here’s the catch: it only works if you have a strong induction drug and perfect monitoring. Not every center can do it. And if you’re high-risk-say, you had a deceased donor kidney or prior rejection-you might still need steroids longer.
Monitoring: More Than Just Blood Tests
Most clinics still check your tacrolimus level the same way: a single morning blood draw. That’s the trough. But that’s like judging a car’s fuel efficiency by checking the tank once a day. It’s incomplete.
Newer centers use AUC monitoring-tracking how much drug is in your blood over 12 hours. It’s more accurate. It shows if you’re under-dosed in the afternoon or over-dosed at night. Same with MMF. The area under the curve tells you if your body is absorbing enough. This isn’t science fiction. It’s happening in UK transplant centers right now.
But it’s not easy. You need multiple blood draws. It costs more. Not every hospital can afford it. But if you’re struggling with side effects or rejection, it might be worth asking for.

What’s Next? Personalized Immunosuppression
The future isn’t one-size-fits-all. Some patients metabolize tacrolimus fast. Others slow it down. Genetic tests can now predict that. One study found that a simple gene test (CYP3A5) could cut the time it takes to reach the right dose by half.
And it’s not just genes. Researchers are looking at immune cell patterns, infection history, even gut bacteria. The goal? To give you just enough drug to protect your kidney-not enough to wreck your health.
By 2030, experts predict 15-20% fewer people will be on the full triple-drug combo. Instead, you’ll get a custom plan: maybe tacrolimus and MMF, no steroids. Or tacrolimus with a new drug like belatacept, which doesn’t hurt your kidneys.
The Hard Truth
Even with this powerful combo, 25% of adult kidney transplant recipients lose their graft within five years. That’s 1 in 4. Why? Because these drugs don’t stop chronic injury-the slow, invisible damage that builds over time. It’s not rejection. It’s scarring. It’s fibrosis. We don’t have a magic bullet for that yet.
And the drugs? They’re not harmless. Diabetes. High cholesterol. Bone thinning. Skin cancer. You’re trading one set of risks for another. That’s why staying on top of your labs, your diet, and your sun protection isn’t optional. It’s survival.
There’s no perfect answer. But there is a path: stay informed, ask questions, and don’t be afraid to push back if your side effects are unbearable. Your transplant team wants you to thrive-not just survive.
Can I stop taking my immunosuppressants if I feel fine?
No. Even if you feel great, stopping your meds can cause your body to reject the transplant within days. The immune system doesn’t ‘remember’ you’re fine-it only remembers the organ is foreign. Never stop or change doses without your transplant team’s approval.
Why do I need blood tests so often?
Because these drugs have narrow safety windows. Too little and your kidney gets rejected. Too much and you damage your kidneys, liver, or nerves. Blood tests track your levels so your dose can be fine-tuned. Early after transplant, you might have blood drawn weekly. Later, it drops to every few months-but never stops.
Are there alternatives to steroids?
Yes. Many centers now use induction drugs like basiliximab or daclizumab to replace steroids in the early phase. Some patients can stop steroids completely by 3 months. Others stay on low doses longer. It depends on your risk level, donor type, and how your body responds. Talk to your specialist about whether steroid withdrawal is an option for you.
What should I do if I get diarrhea from my mycophenolate?
Don’t stop it cold turkey. Call your transplant team. They may reduce your dose to 500 mg twice daily or switch you to mycophenolic acid (MPA), which is easier on the stomach. Sometimes, taking it with food or splitting doses helps. If diarrhea continues, they’ll check for infections like C. difficile before deciding to discontinue it.
Can I take other medications with this regimen?
Many over-the-counter drugs interact dangerously. Antacids, proton pump inhibitors (like omeprazole), and some antibiotics can lower your mycophenolate levels. Grapefruit juice can spike your tacrolimus. Always check with your transplant pharmacist before taking anything new-even herbal supplements. A simple cold medicine could put your kidney at risk.
What You Can Do Today
- Keep a log of side effects: diarrhea, headaches, weight changes.
- Ask about AUC monitoring if you’re having trouble with side effects or rejection.
- Request a pharmacy review-many transplant centers have pharmacists who specialize in this.
- Get annual skin checks. Immunosuppression raises skin cancer risk.
- Don’t skip your blood tests. They’re not bureaucracy-they’re your lifeline.
This regimen saved your kidney. But it’s not a cure. It’s a tool. And like any tool, it works best when you understand how to use it-and when to ask for help.

Jack Havard
February 10, 2026 AT 16:52Gloria Ricky
February 10, 2026 AT 23:25Stacie Willhite
February 11, 2026 AT 17:24Jason Pascoe
February 13, 2026 AT 12:09Annie Joyce
February 14, 2026 AT 14:02Rob Turner
February 16, 2026 AT 08:02Luke Trouten
February 16, 2026 AT 10:59Gabriella Adams
February 16, 2026 AT 21:50