When you hear gabapentin, a prescription medication primarily used to treat nerve pain and certain types of seizures. Also known as Neurontin, it's one of the most commonly prescribed drugs in the U.S. for chronic pain conditions like diabetic neuropathy and postherpetic neuralgia. But gabapentin isn’t just a pain reliever—it affects your brain chemistry in ways that can be helpful, risky, or even dangerous if misused.
Gabapentin works by calming overactive nerves, which is why it helps with pain that feels like burning, tingling, or shooting. It’s also used to control partial seizures in people with epilepsy. But here’s the catch: it doesn’t work the same way as opioids or NSAIDs. It doesn’t reduce inflammation or block pain signals the same way. Instead, it changes how nerves send signals to your brain. That’s why it’s often paired with other meds—but also why it can cause trouble when mixed with things like alcohol, opioids, or even some sleep aids. The risk of slowed breathing or extreme drowsiness goes up fast when you combine gabapentin with these substances. The FDA has even issued warnings about this, especially for older adults or people with lung problems.
People often take gabapentin for years without issues, but side effects like dizziness, weight gain, and brain fog are common. Some users report feeling detached or emotionally flat. And while it’s not addictive like opioids, dependence is real—you can’t just stop it cold turkey without risking seizures or rebound pain. Tapering off slowly under a doctor’s care is key. If you’ve been on it for more than a few weeks, talk to your provider before making any changes.
There’s also growing concern about how gabapentin is prescribed. It’s often used off-label for anxiety, insomnia, or even bipolar disorder—even though the evidence for those uses is weak. That means some people are taking it without a clear benefit, just because it was easy to get. Meanwhile, others who could really use it—like someone with severe nerve pain after shingles—are still struggling to find relief because doctors are wary of side effects.
What you’ll find below are real, practical posts that dig into the details: how gabapentin interacts with other drugs like alcohol and opioids, what long-term use really does to your body, how it compares to alternatives like pregabalin, and why some people have bad reactions while others don’t. You’ll also see how manufacturing issues, dosage errors, and lack of monitoring can turn a safe medication into a serious risk. These aren’t theoretical concerns—they’re based on real cases, FDA reports, and patient experiences. Whether you’re taking gabapentin now, considering it, or just trying to understand a loved one’s prescription, this collection gives you the facts you need to make smarter choices.
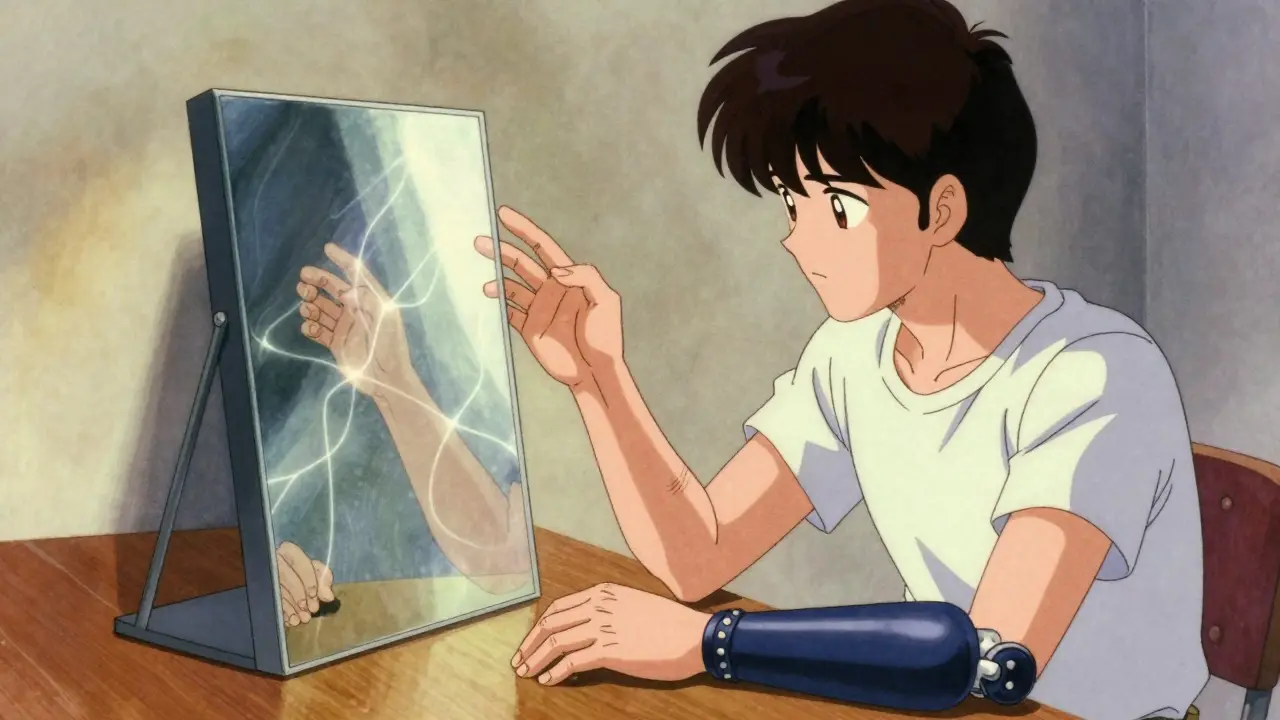
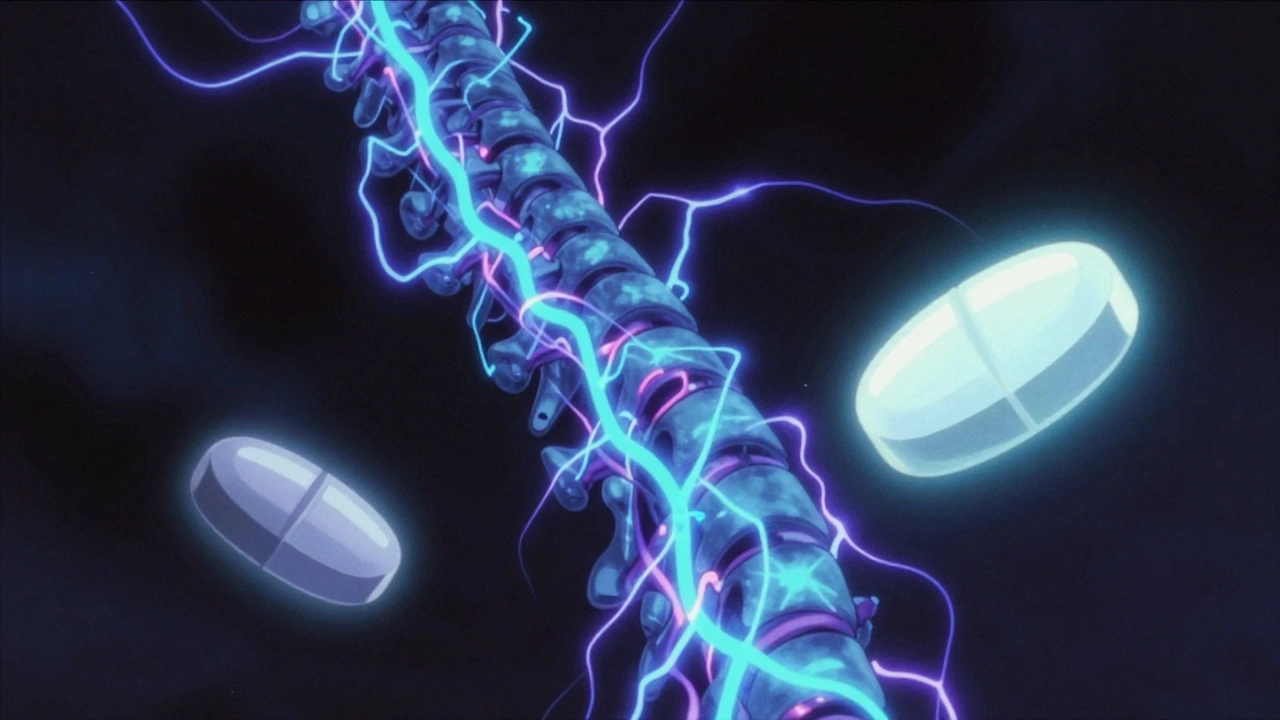
Phantom limb pain is a real neurological condition affecting 60-85% of amputees. Learn how mirror therapy and medications like gabapentin and amitriptyline work, what actually helps, and what new treatments are emerging in 2026.
Gabapentin and pregabalin are first-line treatments for neuropathic pain, but they differ in effectiveness, dosing, cost, and side effects. Learn which one may be better for your condition.