What phantom limb pain really is - and why it’s not "all in your head"
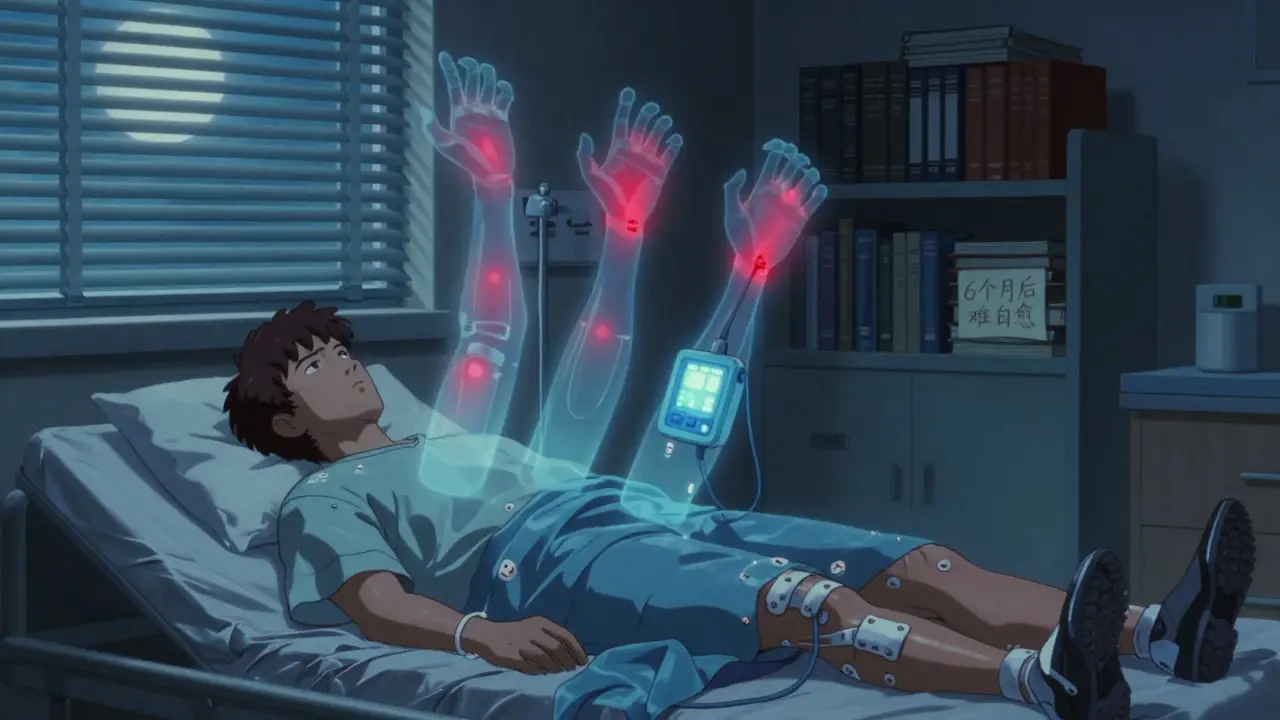
You lose a limb. The wound heals. But you still feel pain - sharp, burning, cramping - in the foot, hand, or leg that’s no longer there. This isn’t imagination. It’s phantom limb pain (PLP), a real neurological condition that affects 60% to 85% of amputees. For decades, doctors thought it was psychological. Then brain scans changed everything. When someone with PLP feels pain, the same areas of the brain that used to process signals from the missing limb light up. The brain hasn’t forgotten the limb. It’s still waiting for signals that will never come - and it’s screaming in confusion.
Most people start feeling this pain within days or weeks after surgery. It often hits hardest in the fingers, toes, or ends of the stump - the parts farthest from the body. Some get mild tingling. Others describe it like a claw digging into their missing foot. About 5% to 10% of cases are severe enough to wreck sleep, mood, and daily life. And if it’s still there after six months? The chances of it going away on its own are almost zero.
Why your brain keeps sending pain signals
It’s not just about the stump. The problem lives in your nervous system. When a nerve is cut during amputation, it doesn’t just go quiet. It gets messy. Damaged nerve endings send out random electrical bursts. Your spinal cord picks them up and starts overreacting - a process called central sensitization. The brain, used to getting constant input from that limb, starts rewiring itself. Neighboring areas - like your face or upper arm - begin to take over the brain space once reserved for your missing hand or leg. Touch your cheek, and suddenly you feel it in your phantom fingers. That’s cortical remapping. It’s not magic. It’s biology.
Some triggers make it worse. Fatigue. Stress. Cold weather. An ill-fitting prosthesis pressing on the stump. Even an infection somewhere else in your body can flare up the pain. The brain doesn’t distinguish between local and distant threats - it just reacts. That’s why treating PLP isn’t just about the missing limb. It’s about calming the whole system.
Medications: What actually helps - and what doesn’t
Doctors start with drugs that were never meant for pain. Tricyclic antidepressants like amitriptyline (10-75 mg daily) and nortriptyline are the most common first-line treatment. They don’t fix your mood - they quiet the overactive nerves in your spinal cord. Many patients report 30-50% pain reduction, but side effects like drowsiness and dry mouth mean about 60% quit within a few weeks.
Anticonvulsants like gabapentin (300-3600 mg daily) and pregabalin (75-600 mg daily) are next. They stabilize nerve firing. On Reddit’s r/amputee community, 72% of users said gabapentin helped - but 58% stopped because of dizziness or brain fog. Pregabalin often causes weight gain. Still, for many, it’s the difference between sleeping and staring at the ceiling.
Over-the-counter painkillers like ibuprofen or naproxen? They help a little - at first. About 65% of patients feel better in the first month. But for 80% of them, the effect fades after three to six months. They’re not the answer for long-term pain.
For stubborn cases, ketamine - an anesthetic - can be given intravenously in small doses (0.1-0.5 mg/kg). It blocks NMDA receptors, which are stuck in overdrive in PLP. Results can be dramatic. But it’s not a daily fix. It’s a hospital-based option for when everything else fails.
Opioids like oxycodone or morphine? They’re controversial. Yes, they work. But the risk of dependence is real. The American Pain Society recommends staying under 50 morphine milligram equivalents per day. Long-term users on pain forums report addiction rates as high as 35%. Most doctors avoid them unless it’s a last resort.
Then there’s botulinum toxin (Botox). Injected into painful neuromas on the stump, it can reduce both pain and sweating. One 2023 case study saw pain drop from 8/10 to 3/10 for 12 weeks. It’s not widely used, but for some, it’s a game-changer.
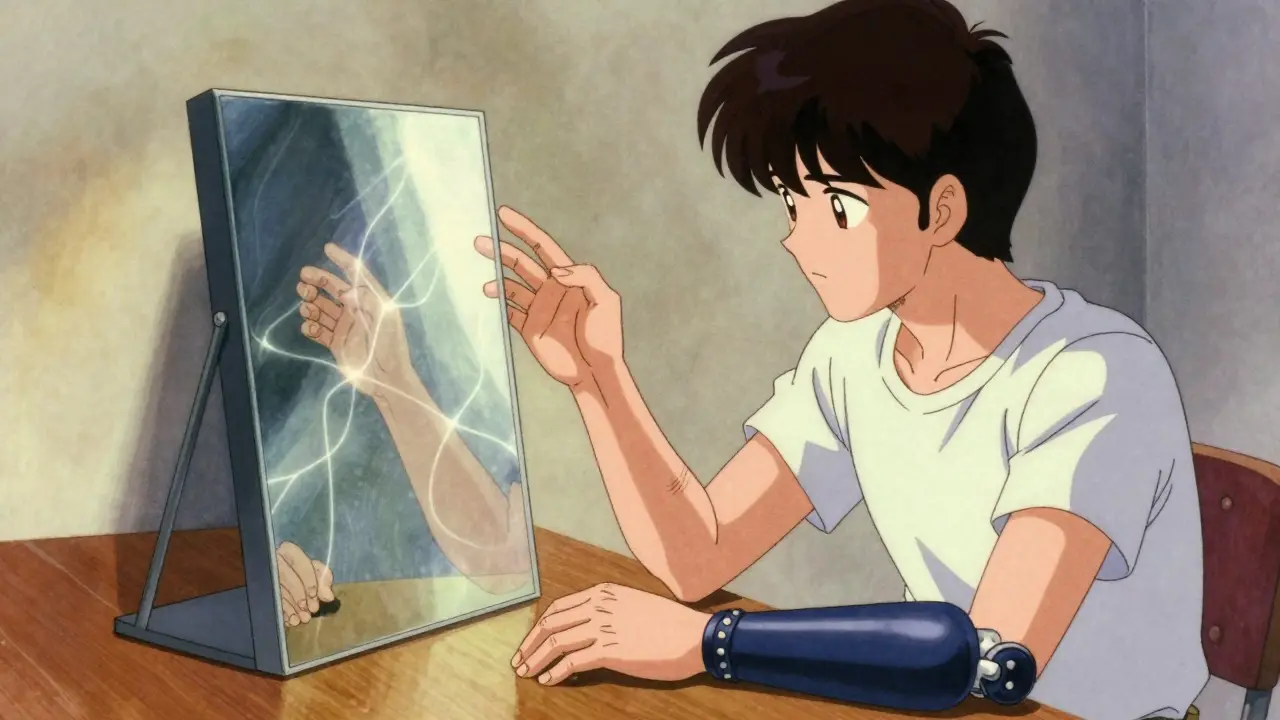
Mirror therapy: Seeing is believing
Here’s where things get strange - and brilliant. Mirror therapy uses a simple box with a mirror inside. You put your intact limb on one side, your stump on the other. The mirror reflects the good limb, making it look like the missing one is still there. Then you move it. You wiggle your fingers. You point your toes. Your brain sees movement - and starts to believe the phantom limb is moving too.
Why does this work? Because your brain is hungry for visual feedback. When it sees the missing limb moving without pain, it slowly rewrites the error message. The rewiring starts to reverse. Studies show mirror therapy can reduce pain by 30-60% in people who stick with it. But here’s the catch: 40% of patients quit within eight weeks. It’s boring. It takes time. You have to do it every day for 15-30 minutes.
It’s not a cure. But it’s one of the few treatments that actually changes how your brain works - not just masks the pain. And it has almost no side effects. No drowsiness. No weight gain. No addiction risk. That’s why experts say it should be tried early - even before heavy meds.
Other tools: TENS, biofeedback, and what’s coming next
Transcutaneous electrical nerve stimulation (TENS) uses small electrodes on the stump to deliver gentle pulses. It’s like a massage for your nerves. About 30-50% of users report moderate relief. It’s cheap, safe, and easy to use at home - but you need proper training. Wrong settings? It won’t help.
Biofeedback teaches you to control your body’s stress responses. With sensors on your skin, you learn to lower your heart rate or relax tense muscles. It helps about 25-40% of people. It’s slow, but it builds skills you can use for life.
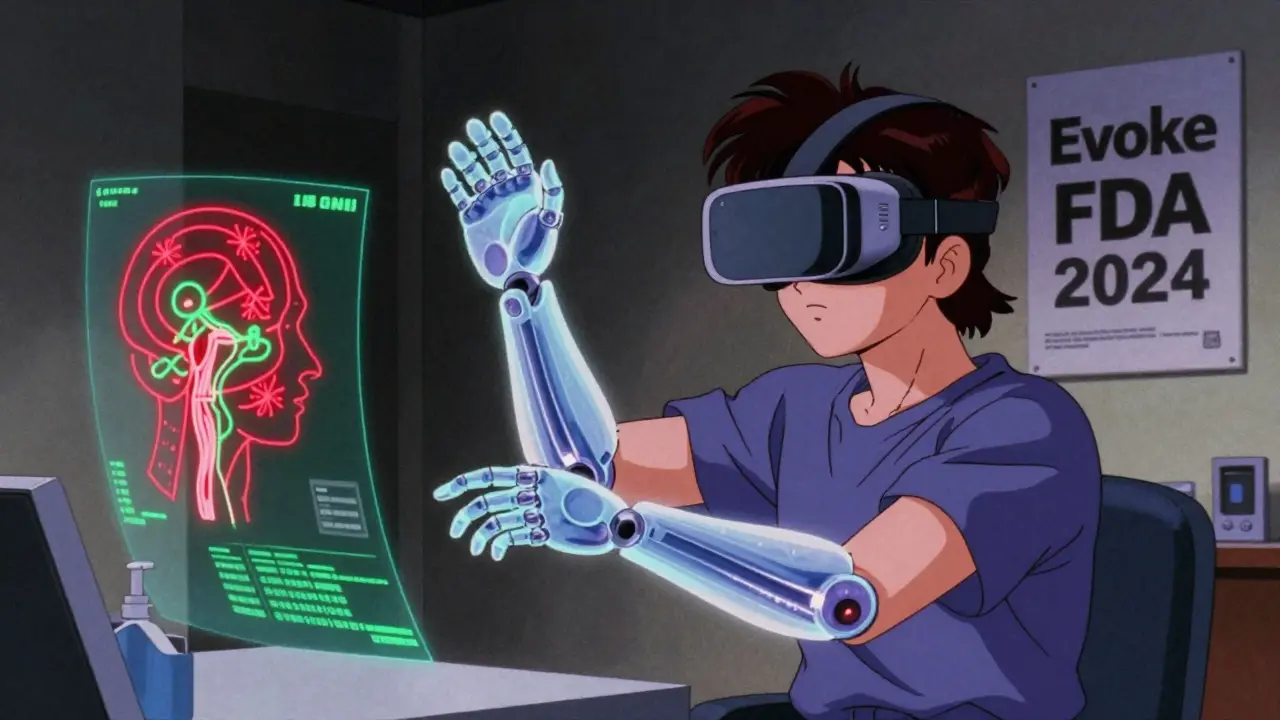
New tech is coming fast. In January 2024, the FDA approved a new spinal cord stimulator called Evoke by Saluda Medical. It adjusts its pulses automatically based on your pain levels - no remote needed. In trials, it cut pain by 65% on average. Another breakthrough: targeted muscle reinnervation combined with osseointegration. Surgeons reroute nerves from the amputated limb to muscles in the stump. Then they attach a metal implant directly to the bone. The result? Better control of prosthetics - and less phantom pain. One 2024 study saw 70% pain reduction in 24 patients.
Virtual reality mirror therapy is on the horizon. Instead of a physical mirror, you wear a headset and see a digital version of your missing limb moving in real time. Early tests show it could boost adherence by 25%. By 2027, it might be standard.
What works best - and how to start
There’s no single solution. The best outcomes come from stacking treatments. Start with low-dose amitriptyline at bedtime. Add mirror therapy every day. Try TENS if you’re comfortable with the device. If pain doesn’t improve in 4-6 weeks, talk to your doctor about gabapentin or a referral to a pain clinic.
Don’t wait. The sooner you act, the better. After six months, PLP becomes harder to reverse. Your brain’s rewiring becomes more fixed. Early intervention - even before you leave the hospital - can make a huge difference. Some hospitals now use epidural anesthesia during amputation to try to calm the nervous system before pain takes root. It’s not guaranteed, but it’s worth asking about.
And don’t go it alone. The Amputee Coalition supports over 12,000 people every year. Peer stories matter. You’re not broken. Your brain is just confused. And with the right tools, it can learn to be quiet again.
What to ask your doctor
- Can we start with amitriptyline or gabapentin? What’s the lowest dose to try?
- Do you have a mirror therapy box I can borrow or buy?
- Is TENS an option for me? Can you show me how to use it?
- Should I be referred to a pain specialist or a clinic that handles phantom limb pain?
- Are there any clinical trials for new treatments I might qualify for?
Is phantom limb pain real, or is it just in my mind?
It’s absolutely real - and it’s not psychological. Brain scans show clear activity in the areas that once controlled your missing limb. This isn’t imagination. It’s your nervous system misfiring after trauma. The pain comes from your spinal cord and brain, not from any physical damage in the stump.
How long does phantom limb pain last?
For some, it fades within weeks. But if it lasts more than six months, the chance of it disappearing on its own is extremely low. That’s why early treatment matters. The longer the pain persists, the more your brain rewires itself to keep feeling it.
Can mirror therapy cure phantom limb pain?
It doesn’t cure it, but it can significantly reduce pain - sometimes by half. It works by tricking your brain into thinking the missing limb is moving without pain, which helps reverse faulty wiring. Success depends on consistency. You need to do it daily for at least 15-30 minutes. Many people quit too soon.
Are opioids safe for long-term phantom limb pain?
Opioids can help in the short term, but they’re not safe for long-term use. The risk of dependence is high, and studies show 35% of long-term users develop addiction. Experts recommend limiting opioids to 30-50 morphine milligram equivalents per day. They should only be used if other treatments fail - and never as a first choice.
Why do some medications stop working over time?
Your body can build tolerance to drugs like gabapentin or amitriptyline. Also, the underlying nerve changes may progress, making the same dose less effective. That’s why treatment often needs to be adjusted. Switching meds, combining therapies, or adding non-drug options like mirror therapy or TENS can help reset your system.
Is there a new treatment I should know about?
Yes. In early 2024, the FDA approved a new spinal cord stimulator called Evoke, which adjusts its signals automatically based on your pain levels. Early results show 65% average pain reduction. Also, virtual reality versions of mirror therapy are being tested and could boost adherence by 25% by 2027. These aren’t widely available yet, but ask your doctor if you qualify for clinical trials.

Mandy Vodak-Marotta
February 5, 2026 AT 05:20Okay so I’ve been dealing with this since my below-knee amputation in 2020, and let me tell you - mirror therapy is the unsung hero. I thought it was a joke at first, like, ‘you’re telling me to stare at a mirror and wiggle my good foot and suddenly my phantom toe stops feeling like it’s in a vise?’ But after two weeks of doing it while watching Netflix? It went from 8/10 pain to 3/10. No drugs. No needles. Just a $20 mirror box from Amazon and patience. I still do it every morning like brushing my teeth. If you’re skeptical, try it for 10 days. No promises, but I’m living proof it’s not magic - it’s neuroplasticity.
Nathan King
February 6, 2026 AT 19:42While the anecdotal evidence for mirror therapy is compelling, one must exercise caution in extrapolating clinical efficacy from self-reported outcomes. The placebo effect remains a formidable confounder in pain studies, particularly when visual feedback is involved. Furthermore, the neuroanatomical reorganization described - while empirically documented - does not inherently validate the therapeutic mechanism without controlled longitudinal trials. The pharmacological regimens cited, particularly the use of gabapentinoids, require scrutiny regarding their risk-benefit ratio in light of recent FDA advisories on CNS depression.
rahulkumar maurya
February 8, 2026 AT 06:42Let’s be real - most of you are wasting time with mirrors and TENS units. The real solution? Ketamine infusions. I’ve seen it. I’ve lived it. 0.3 mg/kg IV, three sessions, and suddenly my phantom foot didn’t feel like it was being slowly crushed by a hydraulic press. Yes, it’s expensive. Yes, you need a clinic. But if you’re still taking amitriptyline like it’s vitamin C, you’re just delaying the inevitable. Stop treating the symptom. Treat the circuitry. And no, ‘it’s all in your head’ isn’t a joke - it’s a diagnosis you’re ignoring.
Demetria Morris
February 8, 2026 AT 17:37I find it deeply irresponsible that this article promotes ketamine and spinal stimulators as viable options without emphasizing the moral obligation to exhaust conservative, non-invasive methods first. People are vulnerable. They’re in pain. And now you’re handing them a chemical escape hatch like it’s a solution, not a last resort. What about dignity? What about learning to live with it instead of numbing it into oblivion? This isn’t a tech fix. It’s a human experience.
Susheel Sharma
February 9, 2026 AT 02:11LOL at the mirror therapy hype. I tried it. My cat knocked over the mirror. I cried. Then I took 600mg gabapentin and watched anime. Pain went from 9/10 to 4/10. Who needs neuroplasticity when you have a 10-year-old prescription? 😅 Also, Botox? That’s just a fancy way to say ‘pay $2k to not feel your ghost foot for 3 months.’ Still better than opioids though. #PhantomLife
Janice Williams
February 9, 2026 AT 03:10It is appalling how this article glorifies experimental neurotechnology while dismissing the spiritual and psychological dimensions of chronic pain. To reduce such a profound human experience to a series of electrodes and pharmaceuticals is not merely reductionist - it is dehumanizing. One does not cure phantom pain by rewiring the brain; one must reconcile with the soul’s memory of the body. Have you considered meditation? Or prayer? Or simply sitting in silence with your grief?
Roshan Gudhe
February 9, 2026 AT 15:05What’s beautiful here is how science and suffering meet. The brain doesn’t care about your limb being gone - it cares about continuity. Mirror therapy isn’t magic - it’s the brain begging for coherence. And yeah, the meds? They’re bandaids on a broken symphony. But we’re learning. Slowly. That’s the thing - we’re not just treating pain anymore. We’re listening to what the nervous system is screaming. And that’s worth more than any pill. 🌱
Rachel Kipps
February 9, 2026 AT 16:30I’ve been on gabapentin for 8 months and it helped at first, but now I just feel foggy all the time. I started mirror therapy last week and I’m already noticing a difference - not in pain, but in how I feel about it. Like, I’m not just waiting for the pain to stop anymore. I’m doing something. It’s small, but it matters. (Sorry for typos - tired.)
Alex LaVey
February 10, 2026 AT 03:07To anyone reading this who feels alone - you’re not. I lost my leg in a motorcycle crash. Thought I’d never sleep again. Now I do yoga, use TENS on my stump, and do mirror therapy with my kid holding the mirror. We laugh. We cry. We keep going. It’s not perfect. But it’s ours. And that’s enough. You got this.
Jhoantan Moreira
February 11, 2026 AT 13:45Just wanted to say - the Evoke device sounds incredible. I’m in the UK and we don’t have access yet, but I’ve been pushing my NHS rep for info. If you’re eligible for trials, DO IT. Also, mirror therapy is free. Literally. A mirror, a box, 15 minutes. No side effects. Why aren’t hospitals handing these out like candy? 🤔
Justin Fauth
February 13, 2026 AT 00:06Ugh, another ‘miracle cure’ article from the US. In my country, we don’t have access to half this stuff. We get a pamphlet and a ‘stay strong’ from our GP. Meanwhile, you guys are getting FDA-approved brain hacks and IV ketamine. It’s not fair. But hey - at least you’ve got the meds. I’ll just keep gritting my teeth and pretending I’m not screaming every night.
Meenal Khurana
February 13, 2026 AT 03:45Mirror therapy works. Did it for 3 months. Pain cut in half. No drugs. Just consistency.
Zachary French
February 13, 2026 AT 04:45Okay, so let me get this straight - you’re telling me that after amputation, my brain literally hallucinates pain because it’s still expecting input? And the solution is… a MIRROR? Like, a 1990s optical illusion? Meanwhile, Big Pharma is pushing ketamine like it’s a TikTok trend. This is either genius or the most elaborate joke ever played on amputees. I’m not mad. I’m just… confused. But also kinda impressed. 🤯
Daz Leonheart
February 14, 2026 AT 19:53you’re not broken. your brain is just confused. i heard that from a therapist after my above-knee and it stuck. mirror therapy is boring as hell but it’s the only thing that made me feel like i had control again. started with 10 mins, now i do 30. no more crying at 3am. you can do this. one day at a time.
Coy Huffman
February 16, 2026 AT 03:04Just read this whole thing and felt seen. I’ve been on pregabalin for a year - gained 20 lbs, felt like a zombie, but the pain was bearable. Then I tried mirror therapy with my daughter’s tablet and a VR app. Didn’t expect it to work. But last week? I moved my phantom toes and didn’t feel a thing. For 10 whole seconds. I cried. Not because it’s gone - but because it’s changing. Slowly. Like a tide. 💙