Neuropathic pain doesn’t feel like a cut or a sprain. It’s burning, electric, or like pins and needles that won’t quit. For millions of people, this isn’t just discomfort-it’s a constant, exhausting reality. Diabetic nerve damage, shingles after the rash fades, or chemo-induced numbness can leave you trapped in a body that’s sending wrong signals. And when over-the-counter painkillers do nothing, doctors turn to two main drugs: gabapentin and pregabalin. Both are gabapentinoids. Both target nerve pain. But they’re not the same. Choosing between them isn’t just about what’s prescribed-it’s about how your body responds, your budget, and your daily life.
How Gabapentin and Pregabalin Actually Work
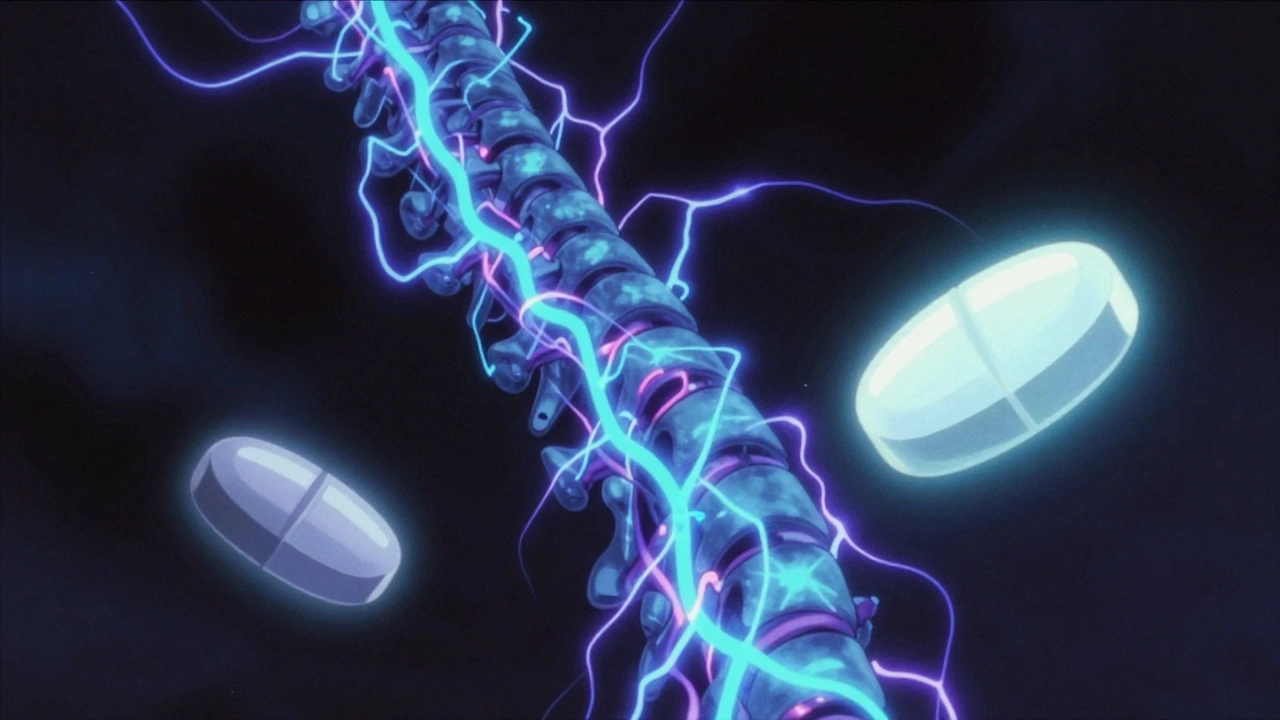
Neither drug is a typical painkiller. They don’t block pain signals like ibuprofen or opioids. Instead, they calm overactive nerves. Both bind to the α2δ subunit of calcium channels in nerve cells. This reduces the release of chemicals like glutamate and substance P that fire up pain signals in the spinal cord. Think of it like turning down the volume on a broken speaker that’s screeching nonstop.
Here’s the key difference: pregabalin binds about six times more tightly to that target than gabapentin does. That means, at the same dose, pregabalin has a stronger effect on nerve signaling. It also does something gabapentin doesn’t: it stops the α2δ protein from moving from nerve cell bodies to the spinal cord, where pain signals get amplified. This might explain why some people feel relief faster with pregabalin.
And despite their names sounding like they’re related to GABA (the brain’s calming chemical), neither drug actually interacts with GABA receptors. That’s a common myth. Their structure is similar, but their action is entirely different.
Pharmacokinetics: Why Timing and Dosing Matter
If you’ve ever tried gabapentin and felt like the effect was hit-or-miss, you’re not imagining it. Gabapentin has terrible absorption. At low doses, maybe 60% gets into your bloodstream. But at higher doses-say, 1,200 mg or more-your body can’t absorb it efficiently anymore. Bioavailability drops to 33%. That means doubling your dose doesn’t double your pain relief. It just gives you more side effects.
Pregabalin doesn’t have this problem. It absorbs almost completely-over 90%-no matter how much you take. That’s why its effects are more predictable. You can titrate it steadily. If 75 mg twice daily isn’t enough, bumping to 150 mg twice daily gives you a clear, proportional increase in pain control.
Another big difference? Speed. Pregabalin hits peak blood levels in under an hour. Gabapentin takes 3 to 4 hours-and even longer if you take it with food or at higher doses. For someone with sudden, sharp nerve pain, that hour can mean the difference between sleeping through the night or lying awake in agony.
Dosing: What Your Doctor Will Actually Prescribe
Doctors don’t just pick a dose out of thin air. They follow guidelines based on years of clinical trials.
For gabapentin, the typical start is 300 mg once a day. Every 3 to 7 days, your doctor might add another 300 mg. The goal is usually 900 to 3,600 mg per day, split into three doses. But here’s the catch: many people never reach the upper end because side effects-dizziness, drowsiness, swelling-get too strong before pain fully improves.
Pregabalin starts lower: 75 mg twice daily. Within a week, most patients move to 150 mg twice daily. The usual target is 300 to 600 mg per day. Unlike gabapentin, pregabalin keeps working up to 600 mg. Studies show that 50% of patients get at least half their pain reduced at this dose. That’s a lot better than placebo, which only helps 15-20% of people.
Both drugs need kidney adjustments. If your creatinine clearance is below 60 mL/min (common in older adults or people with kidney disease), your dose must be lowered. Pregabalin’s dosing is simpler: cut it in half. Gabapentin requires a more complex calculation using the Mawer equation, which many primary care doctors don’t remember offhand. That’s one reason specialists prefer pregabalin.
Effectiveness: What the Science Says
Major medical groups don’t treat them equally. The European Federation of Neurological Societies (EFNS) gives pregabalin a Level A rating for diabetic neuropathy and postherpetic neuralgia-that means strong, consistent evidence from multiple high-quality trials. Gabapentin? Level B. Probably effective, but with more mixed results.
A 2022 review in the Journal of Pain Research found that pregabalin’s linear pharmacokinetics make it more reliable for rapid titration. If you’re recovering from surgery and suddenly developing nerve pain, pregabalin can be ramped up safely within days. Gabapentin? You might need weeks to find a dose that works, and even then, it might not be enough.
But effectiveness isn’t just about numbers. Real people report different experiences. On patient forums, some say pregabalin gave them relief within 24 hours. Others swear by gabapentin’s nighttime effect. One user on Reddit wrote: “900 mg of gabapentin at bedtime keeps me asleep. Pregabalin wears off too fast.” That’s because gabapentin’s half-life stretches at higher doses, giving longer coverage. Pregabalin’s 6.3-hour half-life means it clears faster-so some people need a third dose at night.
Side Effects: What You’ll Actually Feel
Both drugs cause dizziness, drowsiness, and swelling in the hands or feet. About 1 in 3 people report dizziness with pregabalin, compared to 1 in 4 with gabapentin. Weight gain is common too-around 25% of users gain 5 pounds or more over 6 months.
But here’s something rarely discussed: gabapentin can cause unusual side effects like mood swings, confusion, or even suicidal thoughts in rare cases. The FDA issued a warning about this in 2008. Pregabalin carries the same risk, but because it’s more potent and used at lower doses, the overall incidence might be lower.
One big concern in recent years is misuse. Between 2012 and 2021, gabapentinoid-related overdose deaths tripled. Most of these cases involved people combining them with opioids. Pregabalin was involved in 68% of those deaths-even though it’s prescribed far less often than gabapentin. That’s because it’s more potent and has a stronger euphoric effect in some users. That’s why pregabalin now requires a Risk Evaluation and Mitigation Strategy (REMS) program in the U.S., meaning pharmacies must verify prescriptions more carefully.
Cost: The Real-World Decision Maker
In the U.S., generic gabapentin costs about $10 to $20 a month. Pregabalin? Even as a generic, it’s $150 to $250. That’s a 10-fold difference. Insurance often blocks pregabalin unless you’ve tried gabapentin first. Many patients switch to gabapentin not because it’s better-but because they can’t afford the other.
But cost isn’t just about the pill price. If gabapentin doesn’t work well, you might need more doctor visits, more dose adjustments, maybe even emergency care for uncontrolled pain. That adds up. Pregabalin’s higher upfront cost might save money long-term if it gets you back to work or sleep faster.
Outside the U.S., in places like the UK, both are available as generics and priced more similarly. But even there, pregabalin is often reserved for cases where gabapentin failed.
What’s New in 2025?
The gabapentinoid field isn’t standing still. In 2023, the FDA approved Enseedo XR-a new extended-release version of pregabalin that you take once a day. Early trials showed 22% fewer peaks and troughs in blood levels. That means steadier pain control and fewer side effects like dizziness.
Researchers at UCSF are also testing next-gen compounds that target only the α2δ-1 subunit, not α2δ-2. Early animal studies suggest this could cut dizziness by 40% while keeping pain relief. That’s huge. If it works in humans, it could change how we treat nerve pain entirely.
Meanwhile, the American Diabetes Association estimates that half of all diabetics will develop neuropathy. That’s 12 million Americans alone. With aging populations and rising diabetes rates, demand for these drugs will keep growing. Gabapentin will likely stay the most prescribed-but pregabalin will keep growing in specialty care.
Which One Should You Choose?
There’s no universal answer. But here’s how to think about it:
- If you need fast, predictable relief and can afford it-pregabalin is the better choice.
- If you’re on a tight budget, have stable pain, and don’t mind slower titration-gabapentin still works.
- If you’re older or have kidney issues, pregabalin’s simpler dosing may be safer.
- If you struggle with sleep due to nighttime pain, gabapentin’s longer effect at high doses might help more.
- If you’ve tried one and it didn’t work, don’t assume the other won’t. About 30% of people respond to one but not the other.
Start low. Go slow. Track your pain on a scale of 1 to 10 every day. Note side effects. Give it 4 to 6 weeks before deciding. And never stop either drug cold turkey-withdrawal can cause anxiety, insomnia, and even seizures.
Neuropathic pain is complex. No drug is perfect. But gabapentin and pregabalin are the best tools we have right now. Knowing the difference between them isn’t just academic-it’s the key to getting your life back.
Can gabapentin and pregabalin be taken together?
No, they are not typically prescribed together. Both drugs work the same way, so combining them doesn’t usually improve pain relief-it just increases the risk of side effects like dizziness, drowsiness, and swelling. Doctors avoid this unless under very specific, closely monitored circumstances, such as in a pain clinic setting with no other options.
How long does it take for pregabalin to work for nerve pain?
Most people notice some improvement within 1 to 2 weeks. Some report feeling better within 24 to 48 hours, especially for sharp, shooting pain. But full benefits usually take 4 to 6 weeks. Patience is key-rushing to increase the dose can lead to side effects without better pain control.
Is gabapentin or pregabalin better for diabetic neuropathy?
Pregabalin has stronger clinical evidence for diabetic neuropathy. Multiple large trials show it reduces pain by 50% or more in 30-40% of patients, compared to 15-20% with placebo. Gabapentin helps too, but results are more variable. Guidelines from the EFNS and IASP rank pregabalin as a first-line option for this condition.
Do these drugs cause weight gain? Can I avoid it?
Yes, weight gain is common-about 1 in 4 users gain 5 pounds or more. It’s likely due to increased appetite and fluid retention. You can’t always avoid it, but eating a balanced diet, avoiding sugary snacks, and staying active can help minimize it. If you gain more than 10% of your body weight, talk to your doctor about alternatives.
Are there natural alternatives to gabapentin and pregabalin?
Some people try supplements like alpha-lipoic acid, acetyl-L-carnitine, or CBD oil. A few small studies show modest benefits, especially for diabetic neuropathy. But none are as consistently effective as gabapentinoids. The American Academy of Neurology doesn’t recommend them as first-line treatments. They might help as add-ons, but don’t replace prescribed medication without consulting your doctor.
Can I drink alcohol while taking pregabalin or gabapentin?
No. Alcohol increases drowsiness, dizziness, and the risk of falls. It can also worsen depression or anxiety, which are already possible side effects. Even one drink can be dangerous. Most doctors strongly advise complete avoidance. If you drink regularly, talk to your doctor before starting either drug.
What happens if I stop gabapentin or pregabalin suddenly?
Stopping abruptly can cause withdrawal symptoms: anxiety, insomnia, nausea, sweating, and even seizures. Always taper off slowly under medical supervision. A typical taper is reducing the dose by 25% every week. If you’ve been on it for more than 6 weeks, don’t stop without talking to your doctor.
Final Thoughts
Neuropathic pain is invisible, but it’s real. And treating it isn’t about finding a magic pill-it’s about matching the right tool to your body, your life, and your goals. Gabapentin is the workhorse: affordable, widely used, and effective for many. Pregabalin is the precision instrument: faster, more predictable, and often more effective-but at a higher cost and with stricter controls.
There’s no shame in trying one, then switching. Many patients do. What matters is that you’re not stuck with pain that doesn’t have to be there. With the right approach, relief is possible.

Shawna B
December 3, 2025 AT 18:30Jerry Ray
December 5, 2025 AT 07:28Victor T. Johnson
December 5, 2025 AT 19:17Nicholas Swiontek
December 7, 2025 AT 14:57Robert Asel
December 7, 2025 AT 19:16Shannon Wright
December 8, 2025 AT 09:48vanessa parapar
December 8, 2025 AT 15:27Ben Wood
December 9, 2025 AT 13:18Sakthi s
December 9, 2025 AT 20:51Rachel Nimmons
December 10, 2025 AT 18:01Robert Altmannshofer
December 11, 2025 AT 20:23Kathleen Koopman
December 12, 2025 AT 13:48Melania Dellavega
December 13, 2025 AT 05:06Bethany Hosier
December 13, 2025 AT 17:46