When you take a bleeding risk, the chance of uncontrolled or dangerous bleeding due to medication effects. Also known as hemorrhagic risk, it’s not just a footnote on a prescription label—it’s a daily concern for millions on blood thinners, pain meds, or even common supplements. This isn’t theoretical. People end up in the ER every day because they didn’t realize that a cold medicine, an aspirin, or a new antibiotic could turn a small cut into a life-threatening event.
Many of the drugs that raise bleeding risk are things you’d never think twice about. NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen and diclofenac. Also known as painkillers, they’re everywhere—from OTC bottles to prescriptions for arthritis. But they don’t just hurt your stomach—they thin your blood. Then there’s warfarin, a classic blood thinner used for atrial fibrillation, clots, and heart valve replacements. Also known as Coumadin, it’s been around for decades, but its narrow safety window means even small changes in diet or other meds can push you into danger. And don’t forget macrolides, antibiotics like azithromycin that can interfere with heart rhythm and indirectly affect bleeding by altering how other drugs are processed. These aren’t rare cases. They’re common interactions buried in drug guides most people never read.
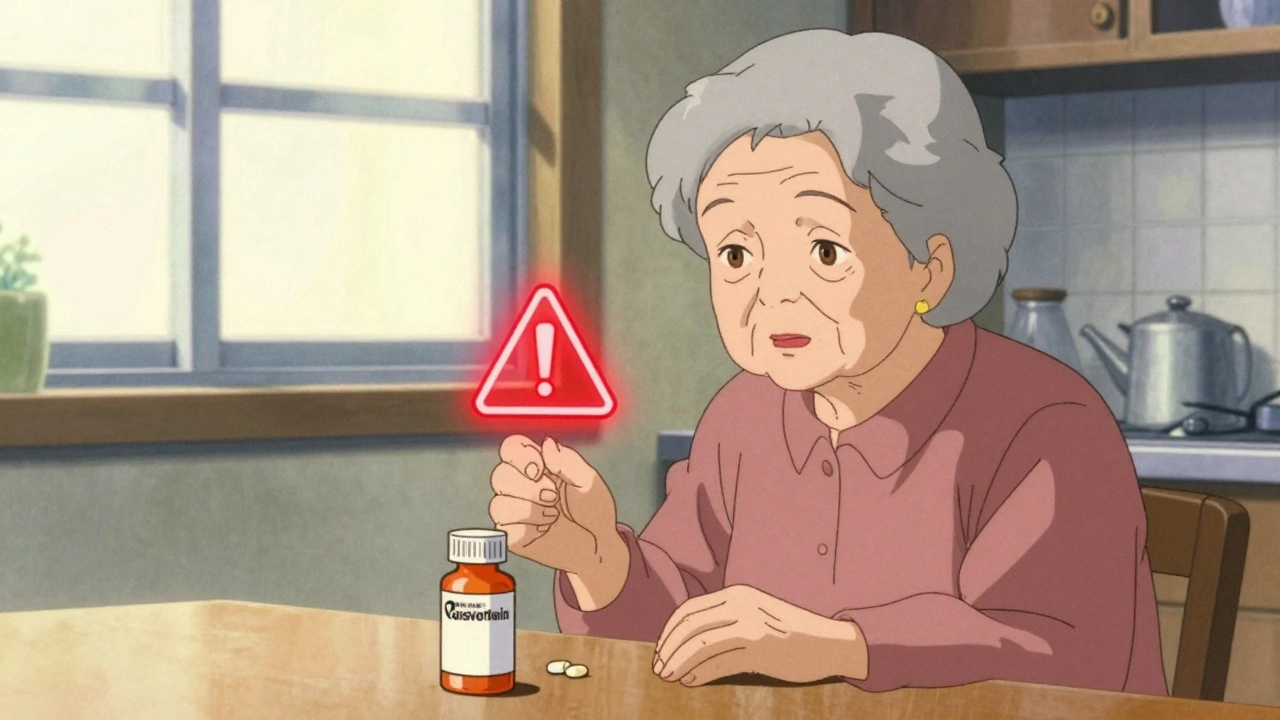
Who’s most at risk? Older adults on multiple meds, people with kidney or liver issues, those with a history of ulcers or bleeding disorders, and anyone mixing prescriptions with OTCs or herbal stuff like fish oil or ginkgo. It’s not about being careless—it’s about not knowing what’s in your medicine cabinet. One pill you’ve taken for years can suddenly become risky when you start a new one. That’s why reading labels isn’t enough—you need to understand how drugs talk to each other.
What you’ll find in the posts below isn’t just a list of warnings. It’s real-world guidance: how to spot hidden bleeding risks in cold meds, why certain antibiotics are dangerous with blood thinners, what to do if you’re on warfarin and need pain relief, and how to talk to your doctor without sounding paranoid. These aren’t theory pieces—they’re tools for people who’ve been there, seen it, and want to avoid the next mistake.

SSRIs can increase bleeding risk by depleting serotonin in platelets, impairing clotting. Learn which antidepressants carry the highest risk, how to reduce danger, and what to watch for-without stopping essential treatment.
Ginkgo Biloba may increase bleeding risk when taken with blood thinners like warfarin, aspirin, or clopidogrel. Learn what the evidence says, which interactions are dangerous, and what steps to take to stay safe.
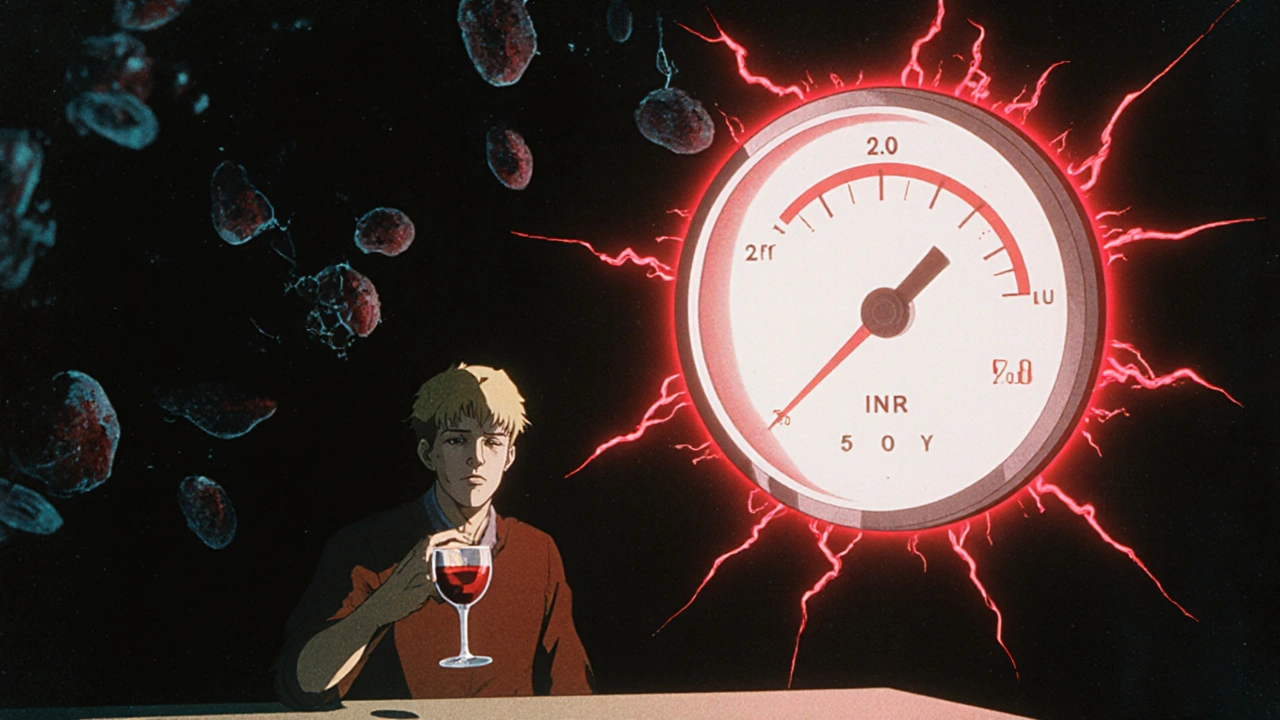
Alcohol can cause dangerous INR fluctuations in people taking warfarin, increasing bleeding risk. Learn how drinking affects your blood thinning levels, what's safe, and what warning signs to watch for.