When you hear the word antidepressants, medications used to treat depression, anxiety, and some chronic pain conditions by balancing brain chemicals. Also known as mood stabilizers, they’re among the most prescribed drugs in the U.S.—but many people start them without knowing how they really work or what to expect. Not all antidepressants are the same. The most common type, SSRIs, a class of antidepressants that increase serotonin levels by blocking its reabsorption in the brain. Also known as serotonin reuptake inhibitors, they include drugs like sertraline and fluoxetine and are often the first choice because they’re generally well-tolerated. But even SSRIs take weeks to kick in, and side effects like sexual dysfunction, brain zaps during withdrawal, or nausea can be enough to make people quit before they see results.
Then there are other types—SNRIs, TCAs, MAOIs—each with different rules, risks, and benefits. Medication interactions, how antidepressants react with other drugs, supplements, or even alcohol. Also known as drug interactions, they’re a hidden danger. For example, mixing an SSRI with Ginkgo Biloba or quercetin supplements can raise bleeding risk or cause dangerous spikes in drug levels. Even something as simple as taking calcium with thyroid meds can interfere with absorption. And if you’re on blood thinners like warfarin, some antidepressants can throw your INR off balance, increasing the chance of internal bleeding.
It’s not just about the pill itself—it’s about your body, your other meds, your lifestyle, and how long you’ve been taking it. Cumulative toxicity can sneak up after months or years. Elderly patients are especially vulnerable because aging changes how drugs are processed. And if you’re switching or stopping, withdrawal symptoms like dizziness, irritability, or electric-shock sensations aren’t just "in your head"—they’re real and often poorly explained.
This collection of posts cuts through the noise. You’ll find clear breakdowns of how SSRIs actually work, why some people get brain zaps, what happens when antidepressants mix with alcohol or herbal supplements, and how to spot dangerous interactions before they hurt you. There’s no fluff—just facts about what’s safe, what’s risky, and what to ask your doctor before you start, stop, or switch.

SSRIs can increase bleeding risk by depleting serotonin in platelets, impairing clotting. Learn which antidepressants carry the highest risk, how to reduce danger, and what to watch for-without stopping essential treatment.
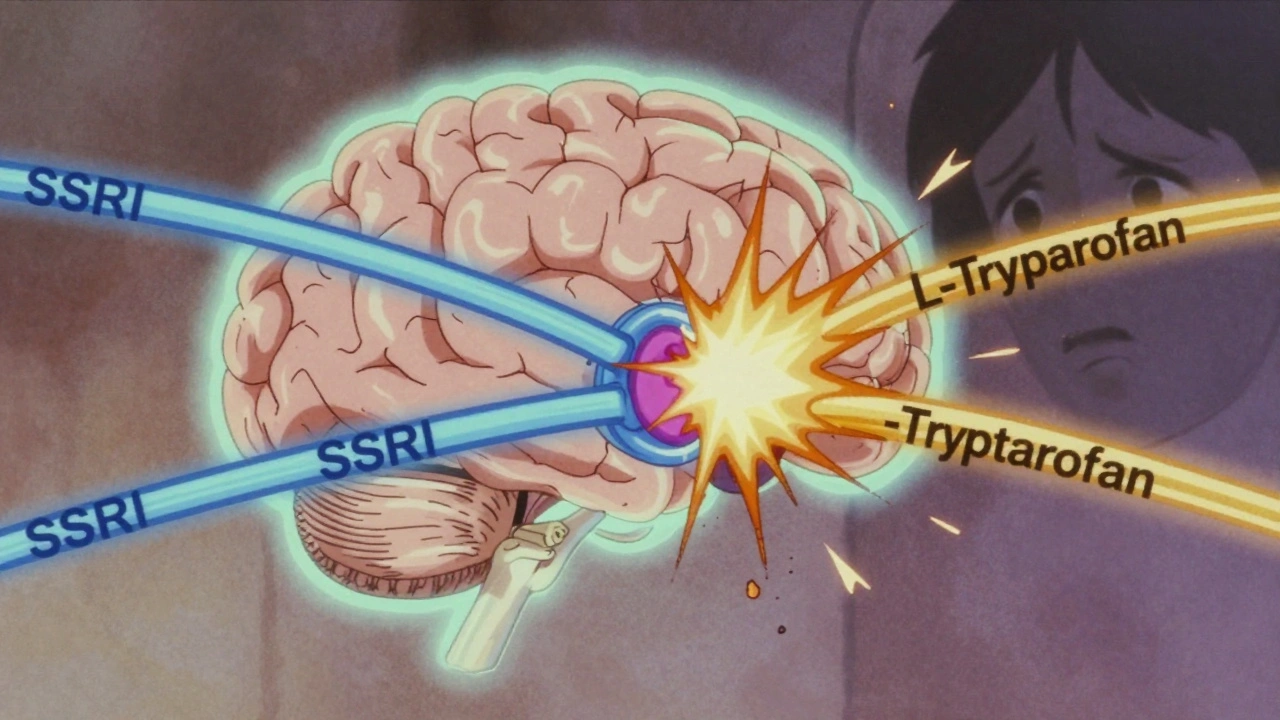
L-Tryptophan boosts serotonin, just like SSRIs. Together, they can trigger serotonin syndrome-a serious, sometimes fatal condition. Learn who’s at risk, what symptoms to watch for, and why most doctors won’t recommend this combo.