Antidepressant and Tryptophan Interaction Checker
When you take an antidepressant like fluoxetine or sertraline, you’re not just changing your mood-you’re tweaking a complex biochemical system built around serotonin. And if you’re also taking L-tryptophan, a common supplement sold for sleep or mood support, you might be stacking two things that do the same job: raising serotonin levels. Sounds harmless, right? It’s not. This combination can trigger something dangerous: serotonin syndrome. And it doesn’t take much to set it off.
How L-Tryptophan Actually Works in Your Brain
L-tryptophan isn’t just another amino acid. It’s the only building block your body uses to make serotonin. Without it, your brain can’t produce this key neurotransmitter at all. Once you eat or supplement with tryptophan, your body converts it first into 5-HTP, then into serotonin. That’s why it’s been studied for decades in depression research. Back in the 1980s, scientists found that giving depressed patients intravenous tryptophan boosted prolactin levels-a sign serotonin activity was increasing. Later studies confirmed that lowering tryptophan levels by 80-90% in just five hours slashes brain serotonin production by 95%.
This isn’t theoretical. The rapid tryptophan depletion method is a real lab tool used to test how sensitive someone’s brain is to serotonin changes. If you’re on an SSRI and your tryptophan drops, your mood crashes-fast. In one study, 47% of patients on SSRIs who were feeling better suddenly relapsed into depression within hours of tryptophan depletion. Their HAM-D depression scores jumped from 4.2 to nearly 19. That’s not a bad day. That’s a clinical relapse.
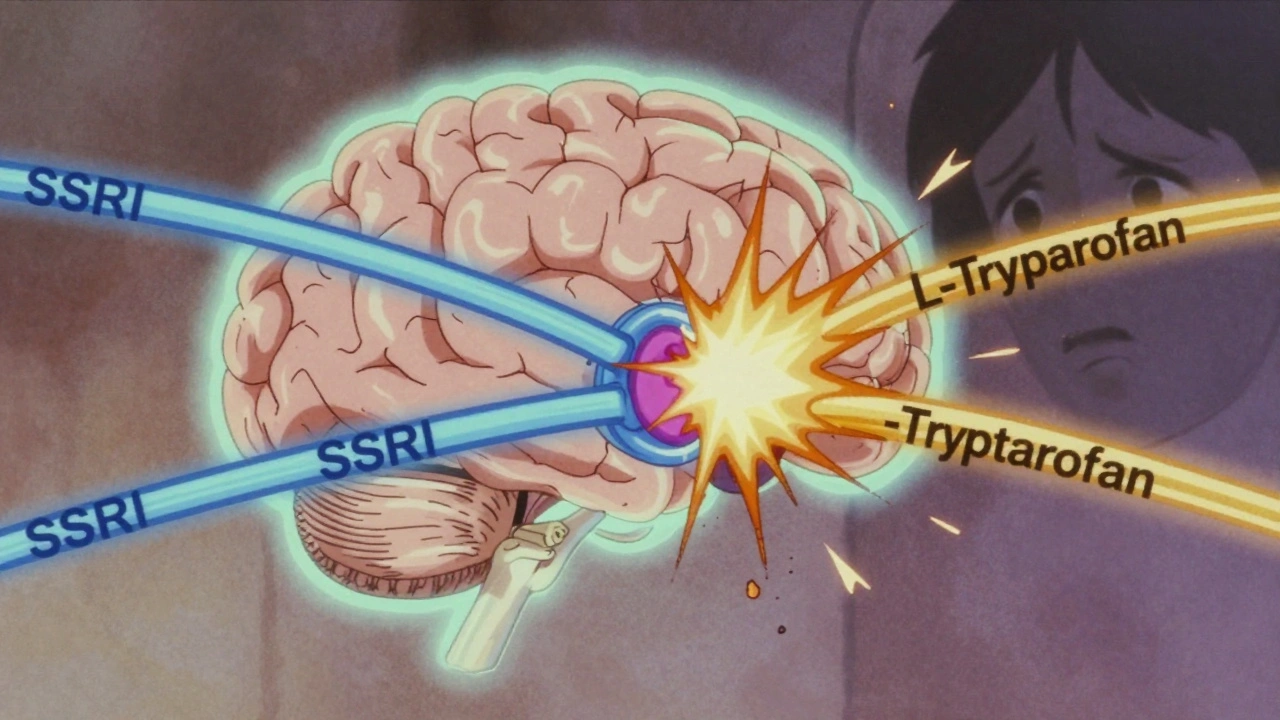
Why Antidepressants and Tryptophan Don’t Mix
SSRIs work by blocking the reabsorption of serotonin, leaving more of it floating around in your brain. Tryptophan, on the other hand, increases how much serotonin your brain can make. Put them together, and you’re not just adding fuel to the fire-you’re turning the whole engine up to max. The result? Too much serotonin in your system.
Serotonin syndrome isn’t a myth. It’s real, measurable, and sometimes deadly. Symptoms start mild: shivering, sweating, restlessness. Then they escalate: muscle rigidity, high fever, seizures. In extreme cases, it leads to organ failure. The CDC documented over 1,500 cases of eosinophilia-myalgia syndrome in 1989 after a contaminated batch of L-tryptophan killed 37 people. That’s why the FDA banned it for years. Even today, 15% of Amazon reviews for tryptophan supplements mention serotonin syndrome risk-mostly from people who didn’t know they were combining it with their antidepressants.
It’s not just SSRIs. MAOIs are even more dangerous when mixed with tryptophan. These older antidepressants stop the enzyme that breaks down serotonin, so any extra serotonin from tryptophan just piles up. The risk is so high that most psychiatrists won’t touch this combo. A 2022 survey of 487 psychiatrists found that 73% actively avoid recommending tryptophan to anyone on SSRIs or MAOIs.
Not All Antidepressants Are the Same
Here’s the twist: not every antidepressant behaves the same way with tryptophan. If you’re on bupropion (Wellbutrin), which works on dopamine and norepinephrine instead of serotonin, you’re in the clear. Studies show zero relapse risk from tryptophan depletion in people taking bupropion. The same goes for some older tricyclics like desipramine, which have weaker serotonin effects.
But if you’re on fluoxetine, escitalopram, or venlafaxine-drugs that strongly boost serotonin-you’re playing with fire. Charney’s 1984 study showed that amitriptyline (a TCA) actually made the brain more responsive to tryptophan after weeks of use. That means even if you’re not on an SSRI, some antidepressants still heighten the risk. The key isn’t just the drug class-it’s how much serotonin each one affects.

The Hidden Danger: Supplements Don’t Warn You
Most L-tryptophan supplements don’t say what they should. A 2021 FDA inspection found that 41% of the 127 tryptophan products they checked didn’t include any warning about serotonin syndrome or interactions with antidepressants. You’ll see labels saying “supports mood” or “promotes sleep,” but nothing about the risk of combining it with your prescription.
Meanwhile, the European Food Safety Authority says you can safely take up to 1 gram per day for “maintenance of normal psychological function.” But that’s not the same as treating depression. Clinical trials use 1-3 grams daily, and even then, only after careful monitoring. The gap between what’s sold on shelves and what’s studied in labs is huge. One woman in Bristol told her GP she’d been taking 1,500 mg of tryptophan nightly for insomnia while on sertraline. She ended up in A&E with tremors and a fever of 39°C. She didn’t know it was dangerous.
Who Might Actually Benefit?
There’s a small group of people who might safely use tryptophan-but only under strict supervision. These are patients who’ve tried SSRIs but only got partial relief. In a 2018 study, doctors added 3 grams of tryptophan daily to SSRI treatment and saw a 63% improvement in symptoms. But here’s the catch: they waited seven to ten days after stopping any other serotonergic drug. They monitored blood tryptophan levels. They checked in weekly. No one just started taking a capsule on their own.
And even then, it’s not for everyone. People with a history of mood disorders, anxiety, or impulsivity are more vulnerable. A 2009 study found that tryptophan depletion made adolescents with ADHD 28% more impulsive and aggressive. If your brain is already sensitive, adding more serotonin might push you over the edge.
What to Do If You’re Already Taking Both
If you’re currently taking L-tryptophan and an antidepressant, don’t stop either cold turkey. That can cause its own problems. Instead:
- Call your doctor or psychiatrist. Don’t rely on online forums or supplement labels.
- Be ready to describe what you’re taking: brand, dose, how long you’ve been using it.
- Watch for symptoms: agitation, rapid heartbeat, confusion, sweating, muscle twitching.
- If you have any of these, go to urgent care. Tell them you’re on an antidepressant and took tryptophan.
There’s no safe “low dose” if you’re on an SSRI. Even 500 mg can be enough to trigger symptoms in sensitive people. And if you’ve been taking it for months, your body may have adapted-making withdrawal harder.
The Bigger Picture: Is Serotonin Even the Real Problem?
Here’s the latest twist: the whole serotonin theory of depression might be wrong. A massive 2022 review of 17 studies involving over 116,000 people found no solid proof that low serotonin causes depression. Brain scans showed no consistent drop in serotonin transporter activity in depressed patients. Some researchers now think the real issue might be inflammation, stress hormones, or how the body breaks down tryptophan into other compounds like kynurenine-not serotonin itself.
That doesn’t mean tryptophan is useless. It still helps make serotonin. But it might not be the answer to depression the way we thought. And if serotonin isn’t the root cause, then stacking it with antidepressants might not fix anything-and could just make things riskier.
Bottom Line: Don’t Guess. Get Guidance.
L-tryptophan isn’t a harmless vitamin. It’s a powerful biochemical tool with real risks when mixed with antidepressants. The science is clear: combining them can cause serotonin syndrome, a potentially life-threatening condition. Even if you feel fine, your brain might be teetering on the edge.
If you’re thinking about trying tryptophan for sleep or mood, talk to your doctor first. If you’re already taking it with an antidepressant, don’t panic-but don’t ignore it either. Schedule a quick appointment. Bring your supplement bottle. Ask: “Could this be interacting with my medication?”
There’s no shortcut to safety here. And no supplement label will tell you what your doctor should.
Can I take L-tryptophan with my SSRI for better sleep?
No. Combining L-tryptophan with SSRIs like sertraline, fluoxetine, or escitalopram increases your risk of serotonin syndrome-even at low doses like 500 mg. While some people report improved sleep, the potential danger outweighs the benefit. Safer sleep aids like melatonin or cognitive behavioral therapy for insomnia don’t carry this risk.
What are the signs of serotonin syndrome from tryptophan and antidepressants?
Early signs include shivering, sweating, restlessness, and a rapid heartbeat. As it worsens, you may develop muscle rigidity, high fever (over 38.5°C), confusion, hallucinations, or seizures. Symptoms usually appear within hours of combining the two. If you notice any of these, seek emergency care immediately. Do not wait.
Is there a safe dose of L-tryptophan if I’m on antidepressants?
There is no established safe dose when combined with SSRIs or MAOIs. Even 250 mg has triggered symptoms in sensitive individuals. Clinical studies only use tryptophan with antidepressants under strict supervision, with washout periods and blood monitoring. Self-administering is not advised.
What antidepressants are safest to combine with L-tryptophan?
Bupropion (Wellbutrin) is the only common antidepressant that doesn’t affect serotonin and has shown no risk of serotonin syndrome with tryptophan. Other non-serotonergic options like mirtazapine (at low doses) or vortioxetine may be safer, but only under medical supervision. Never assume a drug is safe without checking with your prescriber.
Why do supplement labels not warn about antidepressant interactions?
Supplements are not regulated like drugs. In the U.S. and UK, manufacturers aren’t required to prove safety or list drug interactions unless they make a medical claim. A 2021 FDA inspection found 41% of tryptophan products lacked any warning about serotonin syndrome. You can’t rely on labels-you need to talk to your doctor.
How long should I wait after stopping an SSRI before taking tryptophan?
For most SSRIs, a 7-10 day washout period is recommended before starting tryptophan. Fluoxetine (Prozac) has a longer half-life, so you may need to wait 2-3 weeks. This isn’t just a suggestion-it’s a medical standard to prevent dangerous serotonin buildup. Always confirm timing with your prescriber.

Jaswinder Singh
December 2, 2025 AT 01:27Bro this is wild I took tryptophan for months with sertraline and never thought twice. Ended up in the ER with muscle spasms and sweating like I was in a sauna. No one warned me. Supplements are a wild west.
ANN JACOBS
December 3, 2025 AT 17:19Thank you for this incredibly thorough and scientifically grounded breakdown. As a clinical researcher with over two decades in neuropharmacology, I can attest that the serotonin syndrome risk is not merely theoretical-it is mechanistically inevitable when combining serotonergic agents without proper pharmacokinetic calibration. The FDA’s 1989 ban on L-tryptophan was not an overreaction; it was a necessary intervention in the face of unregulated biochemical experimentation by the public. The fact that 41% of current supplements lack warnings speaks to a systemic failure in consumer protection. We must advocate for mandatory labeling, not just for legal compliance, but for ethical responsibility. The human cost of ignorance here is not abstract-it is measured in ICU admissions, lost cognitive function, and preventable deaths.
Eric Vlach
December 4, 2025 AT 02:48My cousin took 1500mg of tryptophan with Lexapro for sleep and ended up shaking so bad she dropped her coffee mug and cut her hand. She thought it was just 'anxiety' until her pulse hit 140. Don't be that person. Talk to your doctor. Seriously.
Bee Floyd
December 4, 2025 AT 09:59Man I’ve seen this play out so many times. People think 'natural' means 'safe'-but your body doesn’t care if the molecule came from a lab or a bean. Tryptophan’s just a stealthy serotonin booster. If you’re on an SSRI, you’re already flooding the system. Adding more is like pouring gasoline on a candle you thought was out. Just… don’t. There’s melatonin. There’s CBT-I. There’s magnesium. There’s literally a thousand safer ways to sleep. You don’t need to risk your brain to get eight hours.
Jeremy Butler
December 6, 2025 AT 06:36The serotonin hypothesis, as currently formulated, is a reductive anthropomorphism of neurochemical dynamics. To ascribe depression to a simple deficit of a single neurotransmitter is to mistake the map for the territory. The very notion that increasing serotonin levels-regardless of synaptic context, receptor sensitivity, or downstream signaling cascades-constitutes therapeutic intervention is a relic of 1980s pharmacological reductionism. The fact that L-tryptophan supplementation may exacerbate pathological states under SSRI co-administration does not invalidate the molecule’s biochemical utility-it reveals the inadequacy of our current diagnostic paradigms. We are treating symptoms with crude tools while ignoring the systemic dysregulation of tryptophan metabolism along the kynurenine pathway, which is far more relevant to neuroinflammation and glutamate excitotoxicity than serotonin synthesis alone.
Courtney Co
December 7, 2025 AT 22:38I took tryptophan with Zoloft for 6 months and felt amazing-like a new person. Why are you all so scared? I’m not some lab rat. My body just works differently. You’re all so paranoid about side effects you forget what it’s like to actually feel good. Maybe the problem isn’t the combo-it’s your fear.
Shashank Vira
December 9, 2025 AT 16:16How quaint. The American public, armed with Amazon reviews and supplement bottles, believes it can outmaneuver neurochemistry. The fact that you require a 1200-word post to warn against something that should be obvious-do not combine serotonergic agents-speaks to the collapse of medical literacy. In India, we still respect the sanctity of the prescription. You treat SSRIs like coffee. You treat tryptophan like oatmeal. This is not progress. This is pharmacological naivety dressed as self-care.
Souvik Datta
December 10, 2025 AT 02:36Hey everyone-let’s not panic, but let’s also not ignore the science. I’ve worked with patients who’ve used tryptophan under supervision and seen real improvements-when done right. But the key is supervision. It’s not about fear. It’s about awareness. If you’re on an SSRI and thinking about trying tryptophan, don’t Google it. Don’t ask Reddit. Call your prescriber. Bring the bottle. Ask: 'Is this safe for me?' That’s all it takes. You don’t need to be a genius to stay safe-you just need to be responsible. And if you’re already taking both? Don’t quit cold turkey. Talk to someone. You’re not alone in this.
Priyam Tomar
December 10, 2025 AT 22:15Wow so you're telling me that people who take supplements might get sick? Groundbreaking. Next you'll say smoking causes cancer or that drinking bleach is bad. This whole post reads like a PSA from a 1998 health class. If you're dumb enough to mix tryptophan with SSRIs without reading the tiny print, you deserve what you get. The real problem isn't the supplement-it's the people who think they know more than their doctors.
Jack Arscott
December 12, 2025 AT 02:50Just wanted to say thank you for this. I’ve been on Lexapro for 3 years and took tryptophan for insomnia last winter. Didn’t know it was risky. I stopped it after reading this. 🙏 Stay safe out there.