Tacrolimus Neurotoxicity Risk Calculator
Personal Risk Assessment
This tool helps you understand your individual risk of tacrolimus neurotoxicity based on multiple factors. Remember that blood levels alone don't tell the whole story.
When you’ve just had a transplant, the last thing you want is for the very drug keeping your new organ alive to start making you feel like you’re falling apart. But for 1 in 3 transplant patients, tacrolimus - the most common immunosuppressant used today - causes neurological side effects that are real, disruptive, and often misunderstood. Tremors that make holding a coffee cup impossible. Headaches so severe they feel like your skull is cracking. Insomnia, confusion, even difficulty speaking. These aren’t random bad days. They’re signs of tacrolimus neurotoxicity, a well-documented but under-discussed problem that can sneak up even when blood levels look perfect.
What Tacrolimus Neurotoxicity Actually Looks Like
Most people think of tacrolimus as a miracle drug. And it is - it cuts rejection rates by 20-30% compared to older drugs like cyclosporine. But that benefit doesn’t come without cost. Neurotoxicity hits about 20-40% of transplant recipients. And it doesn’t wait for high levels to show up. It can strike at 6 ng/mL, even 7.2 ng/mL - right in the middle of the so-called "therapeutic range." The most common symptom? Tremor. Studies show 65-75% of patients who develop neurotoxicity experience it. It’s not just a slight shake. It’s hands that won’t steady enough to button a shirt, write a check, or hold a spoon. For many, it’s the first red flag. One kidney transplant patient on a patient forum described it as "like my body forgot how to be still." Headache comes next - reported by nearly half of affected patients. These aren’t typical tension headaches. They’re deep, constant, crushing pains that don’t respond to ibuprofen or rest. Some patients say they feel like they’re wearing a tight helmet 24/7. Less common but more serious symptoms include dizziness, trouble walking (ataxia), slurred speech, double vision, and even delirium. In rare cases, it can lead to PRES - Posterior Reversible Encephalopathy Syndrome - a condition where fluid leaks into brain tissue, causing seizures or vision loss. Autopsy studies show central pontine myelinolysis, a type of brainstem damage, occurs in up to 17% of liver transplant patients on tacrolimus. These aren’t theoretical risks. They’re documented realities.Why Blood Levels Don’t Tell the Whole Story
Doctors check tacrolimus levels because they’re supposed to be the guide. For kidney transplants, the target is 5-15 ng/mL. For liver and heart, it’s 5-10 ng/mL. But here’s the problem: many patients develop neurotoxicity even when their levels are perfectly within range. A 2023 study found that 21.5% of patients with early neurotoxicity had levels above 15 ng/mL - but there was no clear difference in average levels between those who got sick and those who didn’t. That’s because tacrolimus doesn’t act the same in every body. Some people’s blood-brain barriers let more of the drug slip through. Others have genetic differences in how they metabolize it - especially variations in the CYP3A5 gene. If you’re a CYP3A5 expresser (about 30% of people of African descent, 10-15% of Caucasians), your body clears tacrolimus faster. You need higher doses to stay in range, which means you’re getting more of the drug overall - and more of it crossing into your brain. A 2021 study showed that tailoring doses based on CYP3A5 genotype reduced neurotoxicity by 27%. Electrolytes matter too. Low sodium - hyponatremia - is a major trigger. Even mild drops below 135 mmol/L can make neurotoxicity worse. Some patients see their tremors and headaches vanish just by correcting their sodium levels, without touching the tacrolimus dose at all. That’s why checking electrolytes isn’t optional - it’s essential.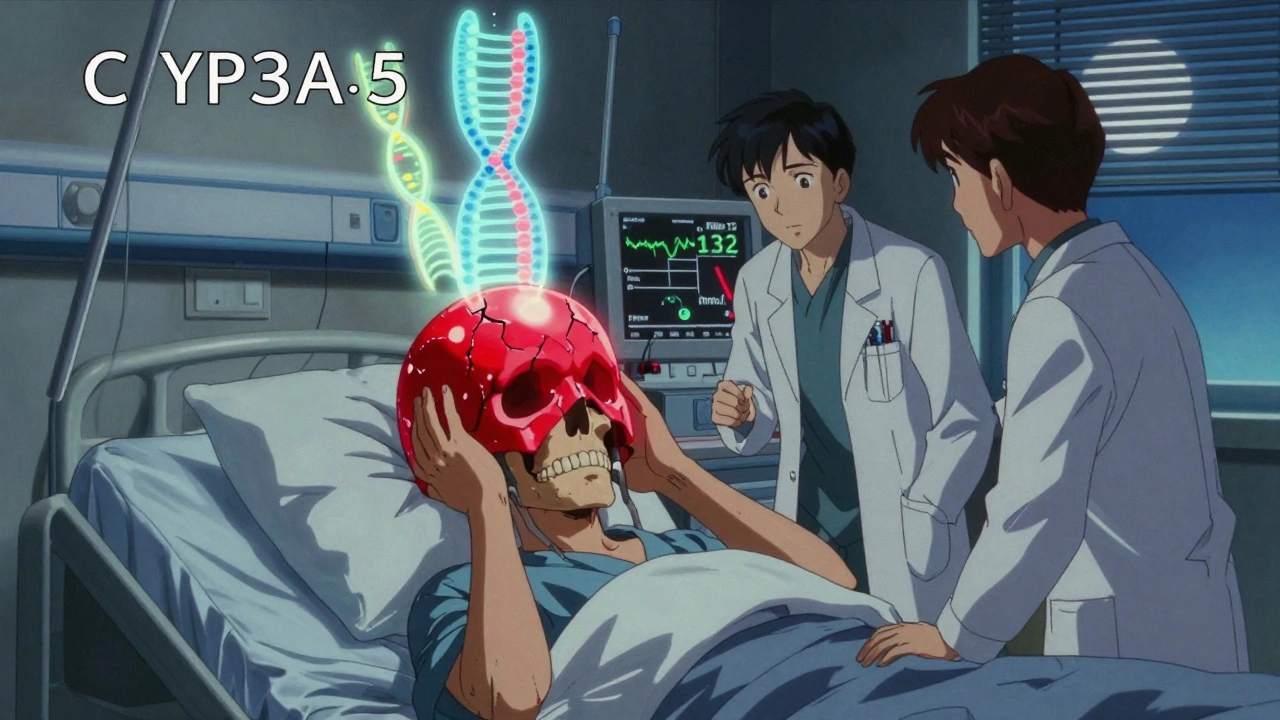
Who’s at Highest Risk?
Not everyone gets neurotoxicity. But some groups are far more likely to. Liver transplant recipients have the highest rate - 35.7%. Kidney recipients follow at 22.4%, then lung at 18.9%, and heart at 15.2%. Why? The liver is the main organ that breaks down tacrolimus. When it’s damaged or newly transplanted, metabolism is unpredictable. That means levels can spike unexpectedly. Age matters. Older patients are more sensitive. So are people with pre-existing neurological conditions, like migraines or essential tremor. And timing is everything. Most cases appear within the first 30 days after transplant, when the body is still adjusting and drug levels are being fine-tuned. That’s why the American Society of Transplantation now recommends routine neurological checks during that first month - not just blood tests. Another big risk factor? Drug combinations. Tacrolimus doesn’t play well with certain antibiotics, sedatives, or antipsychotics. Carbapenems, linezolid, midazolam, propofol, and even common drugs like lorazepam or risperidone can dramatically increase seizure risk when mixed with tacrolimus. Many patients don’t realize their new headache or tremor started after being given antibiotics for an infection. It’s not the infection - it’s the combo.What Happens When You Get Symptoms?
Too often, patients wait weeks before anyone connects the dots. One survey found 55% of patients said it took their medical team 2-3 weeks to realize their tremor or headache was from tacrolimus. That delay can turn mild symptoms into something more serious. The good news? Most cases improve quickly once recognized. The standard approach is simple: reduce the dose, switch to cyclosporine, or both. About 36% of patients get relief just by lowering the tacrolimus dose. Another 42% are switched to cyclosporine - which has lower neurotoxicity risk (15-20% lower) but higher rejection risk. The trade-off is real. Studies show rejection rates jump 15-20% after switching. So it’s not a decision made lightly. In mild cases, correcting sodium or magnesium levels can be enough. One patient reported his tremor vanished within 72 hours of dropping his tacrolimus dose from 0.1 mg/kg to 0.07 mg/kg - still within therapeutic range. Another found relief just by increasing salt intake and fluids after her sodium dropped to 132 mmol/L.
What’s Next? Better Tools on the Horizon
The current system is reactive. We wait for tremors, then react. But the future is proactive. The TACTIC trial, launching in 2024, is testing a new algorithm that combines CYP3A5 genetics, magnesium levels, blood pressure, and tacrolimus dosing to predict and prevent neurotoxicity before it starts. If it works, we’ll move from guessing to precision. There’s also new drug development. LTV-1, a next-generation calcineurin inhibitor designed to barely cross the blood-brain barrier, entered phase 2 trials in 2023. If approved by 2027 as expected, it could replace tacrolimus for many patients - offering the same protection against rejection without the brain fog and shaking. Until then, the message is clear: don’t ignore the tremor. Don’t dismiss the headache. Don’t assume your levels are "fine" just because they’re in range. If you’re on tacrolimus and something feels off - your body is telling you something. Speak up. Ask for a neurological evaluation. Check your sodium. Ask about your CYP3A5 status. You’re not overreacting. You’re protecting your brain - and your future.When to Call Your Transplant Team
Don’t wait. If you’re on tacrolimus and notice any of these, contact your team immediately:- New or worsening hand tremors, especially if they interfere with daily tasks
- Headaches that are different from your usual pattern - constant, crushing, or unresponsive to painkillers
- Difficulty walking, dizziness, or loss of balance
- Confusion, memory lapses, or feeling "foggy"
- Double vision, blurred vision, or trouble focusing
- Sudden weakness in arms or legs
- Slurred speech or trouble swallowing
Can tacrolimus neurotoxicity be reversed?
Yes, in most cases. Symptoms like tremor and headache often improve within days to a week after reducing the tacrolimus dose or switching to another immunosuppressant like cyclosporine. Even mild cases linked to low sodium can resolve quickly with electrolyte correction. However, severe cases involving PRES or brainstem damage require urgent care and may leave lasting effects if not treated promptly.
Are my tremors really from tacrolimus if my blood level is normal?
Absolutely. Neurotoxicity can occur even when tacrolimus levels are within the therapeutic range. Individual differences in how the drug crosses the blood-brain barrier, genetic factors like CYP3A5 status, and interactions with other medications or electrolyte imbalances can all trigger symptoms regardless of blood concentration. Your symptoms are real - and they’re likely related to the drug.
Should I ask for a CYP3A5 genetic test?
If you’re on tacrolimus and have experienced side effects - or if you’re at high risk (e.g., African ancestry, liver transplant), yes. Studies show CYP3A5 genotype-guided dosing reduces neurotoxicity by 27%. While not yet standard everywhere, many transplant centers offer it, especially for patients with unexplained symptoms. It’s a simple blood or saliva test that can help tailor your dose before problems start.
Can other medications make tacrolimus neurotoxicity worse?
Yes. Several common drugs - including antibiotics like linezolid and carbapenems, sedatives like midazolam and propofol, and antipsychotics like risperidone and haloperidol - can increase the risk of seizures and worsen neurological symptoms when taken with tacrolimus. Always tell your transplant team about every new medication, even over-the-counter or herbal ones.
Is switching to cyclosporine a good option if I have neurotoxicity?
It’s a common and often effective choice. Cyclosporine has lower neurotoxicity risk than tacrolimus, and many patients feel better after switching. But it carries a higher risk of rejection - about 15-20% more - and can cause more kidney damage over time. The decision should be made carefully with your transplant team, weighing your symptoms against your rejection risk.
How long does it take for neurotoxicity symptoms to go away?
Most patients see improvement within 3 to 7 days after adjusting the dose or switching drugs. Tremors and headaches often fade fastest. More severe symptoms like confusion or ataxia may take longer - up to 2 weeks. In rare cases of permanent brain damage, symptoms may not fully resolve. Early recognition is key to full recovery.
Can I just stop taking tacrolimus if the side effects are bad?
Never stop tacrolimus without medical supervision. Stopping suddenly can trigger acute rejection, which can lead to organ failure and death. If side effects are severe, work with your transplant team to safely adjust your regimen. There are alternatives - but they must be managed carefully.


Billy Schimmel
December 7, 2025 AT 11:54pallavi khushwani
December 9, 2025 AT 10:30People need to know this isn't just 'side effect' - it's a clue.
Max Manoles
December 11, 2025 AT 10:28Failure to implement pre-emptive genotyping constitutes a breach of the standard of care in transplant medicine. The 27% reduction in neurotoxicity is not a marginal gain-it is a moral imperative.
Katie O'Connell
December 12, 2025 AT 23:00Annie Gardiner
December 13, 2025 AT 04:00Kumar Shubhranshu
December 14, 2025 AT 10:11Kenny Pakade
December 15, 2025 AT 10:05brenda olvera
December 16, 2025 AT 21:28olive ashley
December 17, 2025 AT 00:51joanne humphreys
December 17, 2025 AT 16:43Priya Ranjan
December 18, 2025 AT 07:40Gwyneth Agnes
December 19, 2025 AT 13:00Kay Jolie
December 20, 2025 AT 20:39Dan Cole
December 22, 2025 AT 08:52pallavi khushwani
December 23, 2025 AT 07:26Genetics isn’t magic. It’s just science that finally caught up.