SSRI-NSAID Bleeding Risk Calculator
Your Risk Assessment
When you're managing chronic pain and depression at the same time, it's easy to assume your doctor has everything under control. But here's something most people don't know: taking an SSRI like sertraline or fluoxetine along with an NSAID like ibuprofen or naproxen can double your risk of a dangerous gastrointestinal bleed. This isn't a rare side effect-it's a well-documented, predictable, and preventable danger that affects millions.
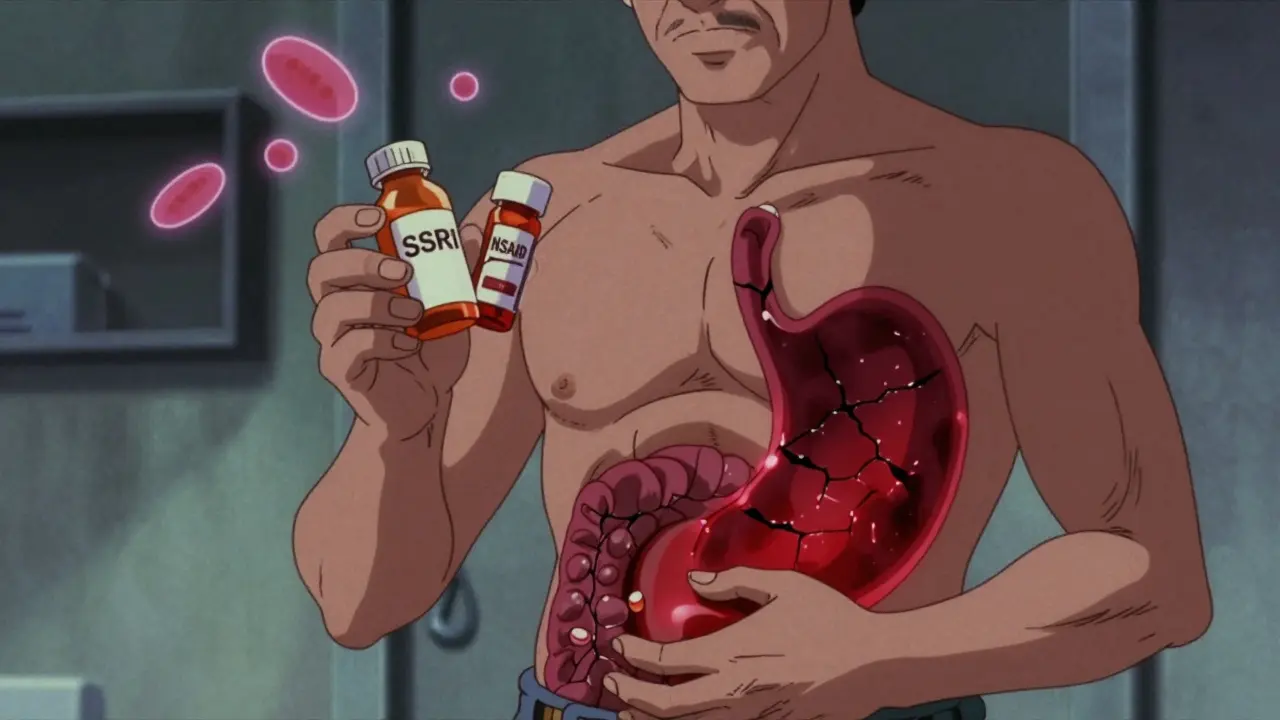
Why This Combination Is So Dangerous
SSRIs and NSAIDs work in completely different ways, but they both mess with your body's ability to stop bleeding. SSRIs, used for depression and anxiety, block serotonin reuptake in the brain. But serotonin isn't just a mood chemical-it's also critical for platelet function. Platelets are the cells that rush to seal cuts in blood vessels. When SSRIs drain serotonin from platelets, they can't stick together properly. That means even a small tear in your stomach lining might not clot, letting blood leak out slowly. NSAIDs, used for arthritis, headaches, or back pain, attack the stomach's natural defenses. They block COX-1 enzymes, which produce prostaglandins-the protective mucus and blood flow that shield your stomach lining from acid. Without that shield, your stomach becomes vulnerable. Take enough NSAIDs over time, and you can develop ulcers without even knowing it. Put them together? It's not 1 + 1 = 2. It's more like 1 + 1 = 4. A 2023 meta-analysis in Digestive Diseases and Sciences confirmed that using both drugs at the same time raises the risk of upper GI bleeding by 75% compared to using either one alone. That’s not a small increase. That’s the difference between a 1% risk and a 1.75% risk-and for older adults or people with past ulcers, that jump can mean the difference between a minor issue and a life-threatening emergency.Who’s Most at Risk?
Not everyone who takes both drugs will bleed. But certain people are playing with fire:- People over 65-stomach lining thins with age
- Those with a history of peptic ulcers or GI bleeding
- Patients also taking blood thinners like warfarin or aspirin
- People on high-dose or long-term NSAIDs
- Those with H. pylori infection (a common stomach bacteria that weakens the lining)
Which Drugs Are the Worst?
Not all SSRIs are equal, and not all NSAIDs are created the same. For NSAIDs, the risk isn't uniform:- High risk: Naproxen, diclofenac, piroxicam, ketorolac
- Lower risk: Ibuprofen (at standard doses)
- Safest option: Celecoxib (a COX-2 inhibitor)-it doesn’t block the protective prostaglandins as much
What Should You Do? A 3-Step Plan
If you're on both an SSRI and an NSAID, here’s what to do right now:- Ask yourself: Do I really need the NSAID? For many people, acetaminophen (Tylenol) works just as well for pain without the bleeding risk. It doesn’t affect platelets or stomach lining. Try it first.
- If you must keep the NSAID, switch to celecoxib. It’s more expensive, but it’s far safer. Talk to your doctor about whether your insurance covers it.
- Always add a proton pump inhibitor (PPI). Omeprazole 20mg daily, pantoprazole, or esomeprazole cuts the excess bleeding risk by 70%. This isn’t optional for high-risk patients. It’s standard care.
What About the Other Options?
Sometimes, you can avoid the problem entirely by switching medications.- For depression: Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelets. It’s a solid alternative for people who need to avoid bleeding risks.
- For pain: Physical therapy, heat/cold therapy, or even acupuncture can reduce reliance on NSAIDs. For arthritis, duloxetine (Cymbalta)-an SNRI-can treat both pain and depression without the same bleeding risk as SSRIs.
Real Stories, Real Consequences
Reddit threads and patient forums are full of warnings. One user described black, tarry stools for three days before going to the ER-only to find out they had a bleeding ulcer from sertraline and daily ibuprofen. Another person, on naproxen for rheumatoid arthritis and fluoxetine for anxiety, ended up in the hospital with a hemoglobin level of 7.8 (normal is 12-16). They needed two units of blood. But there are success stories too. One Drugs.com user switched from naproxen to celecoxib, added omeprazole, and went 18 months without a single GI issue. That’s the kind of outcome we should be seeing more of.Why Isn’t This Being Fixed?
The problem isn’t lack of evidence. The FDA added warnings to SSRI labels in 2019. The EMA did the same in 2020. Studies have been consistent since 2002. Yet, a 2022 audit of 2.1 million patient records found nearly 30% of SSRI users were also prescribed NSAIDs in the same six months. That’s over 9 million people at risk. Doctors aren’t ignoring it-they’re overwhelmed. A 2022 Medscape survey found 68% of patients weren’t warned about this interaction. It’s not malpractice. It’s system failure. The average primary care visit is 15 minutes. There’s no time to check every possible drug interaction unless the system forces it. That’s why hospitals like Cleveland Clinic started embedding automated alerts in their electronic records back in 2019. Since then, they’ve seen a 42% drop in GI bleeding admissions among dual-therapy patients. It works. We just need it everywhere.The Bottom Line
This isn’t a "maybe" risk. It’s a confirmed, measurable, and preventable danger. If you’re taking an SSRI and an NSAID together:- Stop assuming it’s safe
- Don’t wait for symptoms like black stools, vomiting blood, or dizziness
- Don’t assume your doctor knows-ask them
Every year, this interaction costs the U.S. healthcare system over $1.2 billion. But behind every dollar is a person who almost died because no one told them. You don’t have to be one of them.
Can I take ibuprofen with sertraline?
Taking ibuprofen with sertraline increases your risk of upper GI bleeding by about 75% compared to using either drug alone. While ibuprofen is one of the safer NSAIDs, it still blocks protective stomach lining defenses. The safest approach is to avoid combining them. If you must use both, take a proton pump inhibitor like omeprazole daily and limit ibuprofen to the lowest effective dose for the shortest time possible.
What’s the safest NSAID to take with an SSRI?
Celecoxib (Celebrex) is the safest NSAID option when combined with an SSRI. Unlike traditional NSAIDs, it doesn’t significantly inhibit COX-1 enzymes, which protect the stomach lining. Studies show its bleeding risk is close to baseline levels (OR 1.16), making it a much better choice than naproxen, diclofenac, or even ibuprofen. However, it still carries some risk, so pairing it with a proton pump inhibitor is strongly recommended.
Do all SSRIs increase bleeding risk equally?
Most SSRIs carry similar bleeding risks because they all reduce platelet serotonin, which is needed for clotting. Some studies suggest escitalopram may have a slightly lower risk than fluvoxamine or paroxetine, but the difference is small and not enough to rely on. If you’re on an SSRI and need an NSAID, switching SSRIs won’t solve the problem-you need to address the NSAID or add a PPI.
Can I just take a PPI and keep using both drugs?
Yes, adding a proton pump inhibitor (PPI) like omeprazole or pantoprazole daily reduces the excess bleeding risk from SSRI-NSAID use by about 70%. For many patients, this is a safe and effective strategy. But it’s not a free pass. PPIs aren’t harmless-they can affect nutrient absorption and increase infection risk with long-term use. So the goal should be to use the lowest effective dose for the shortest time, and ideally, avoid the combination altogether if possible.
Are there antidepressants that don’t raise bleeding risk?
Yes. Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelet serotonin and carries no increased bleeding risk. Duloxetine (Cymbalta), an SNRI, also has a lower bleeding risk than SSRIs and can even help with chronic pain. If you’re on an SSRI and need long-term NSAID use, talking to your doctor about switching to one of these alternatives could eliminate the interaction entirely.

Jacob den Hollander
February 10, 2026 AT 04:59I’ve been on sertraline for 5 years, and honestly? I didn’t even know ibuprofen was a problem-my doctor just said "take it if you need it"... I’ve been popping Advil for my back pain like it’s candy. Now I’m scared. I just called my pharmacist and they said I should switch to Tylenol and get a PPI. I’m gonna do it. Thanks for the wake-up call.
John Watts
February 10, 2026 AT 15:06This is why I tell everyone: don’t trust your doctor to catch every interaction. They’re drowning in charts and time limits. I used to take naproxen with fluoxetine-until I had black stools and ended up in the ER at 3 a.m. They gave me a transfusion. I’m now on celecoxib + omeprazole. No more scares. If you’re on both, don’t wait for symptoms. Act now. Your stomach will thank you.
Monica Warnick
February 10, 2026 AT 18:42So... let me get this straight. Depression meds + pain meds = stomach bleeding? And we’re just now talking about this? Like, why isn’t this on every pill bottle? Why isn’t there a giant red warning? I feel like Big Pharma is letting this slide because they make more money selling PPIs than preventing bleeding. And now I’m supposed to trust a drug company that’s been lying to us for decades? Nope. I’m switching to CBD oil. And maybe a crystal. Just in case.
Jonah Mann
February 12, 2026 AT 12:10Y’all need to chill. I’m on sertraline and ibuprofen daily for migraines. I’ve been doing this for 8 years. No issues. My GI doc said the risk is real but overblown for healthy people under 50. Also, celecoxib is expensive as hell and my insurance won’t cover it. So I’m gonna keep taking ibuprofen and just drink milk with it. Works for me. Also, PPIs cause vitamin B12 deficiency-don’t ignore that. Balance, people.
Tatiana Barbosa
February 13, 2026 AT 00:09Let’s get real. The data is clear: SSRI+NSAID = 75% higher GI bleed risk. But here’s the thing-most people don’t even know what a PPI is. We need public health campaigns. Billboards. TikTok videos. Not just medical journals. I’m a nurse. I’ve seen patients bleed out because no one told them. This isn’t about being paranoid. It’s about basic safety. If you’re on both, talk to your pharmacist. Ask for omeprazole. It’s $10 at Walmart. Do it.
Random Guy
February 14, 2026 AT 05:37Oh wow, so now I can’t take ibuprofen for my headache without risking death? Cool. Next you’ll tell me water is dangerous if you drink it while on antidepressants. I’m sure the FDA will slap a warning on oxygen next. I mean, come on. I’ve been doing this for a decade. I’m fine. Maybe my body just doesn’t care about your studies.
Andy Cortez
February 14, 2026 AT 15:19So the real danger isn’t the drugs-it’s the system. Doctors are paid per visit, not per outcome. They don’t have time to explain this. Pharmacies don’t warn you. Insurance blocks celecoxib. And now we’re supposed to be the ones to fix it? Yeah, right. I’m not gonna play doctor. I’m gonna keep taking my meds and hope for the best. This isn’t personal. It’s capitalism.
Patrick Jarillon
February 16, 2026 AT 08:38Did you know the FDA didn’t mandate these warnings until 2019? That’s because the pharmaceutical industry lobbied hard to delay them. They knew. They knew for decades. And now they’re selling you PPIs like they’re miracle cures. But PPIs are linked to kidney failure, dementia, and bone loss. They’re just trading one risk for another. The real solution? Stop trusting the system. Go off SSRIs. Go off NSAIDs. Find a naturopath. Or better yet-move to Iceland. They don’t even use these drugs.
Kathryn Lenn
February 16, 2026 AT 23:47