SSRIs are the most common type of antidepressant prescribed today. If you’ve been told you might benefit from one, you’re not alone. About 13% of Americans over age 12 take antidepressants, and nearly 70% of those are SSRIs. These drugs aren’t magic pills, but they’ve helped millions regain control over their moods, energy, and daily lives. Still, they don’t work the same for everyone-and side effects can be confusing, even scary. So how do they actually work? And what should you expect when you start taking one?
How SSRIs Change Your Brain Chemistry
SSRIs stand for Selective Serotonin Reuptake Inhibitors. That’s a mouthful, but the idea is simple: they help more serotonin stick around in your brain.
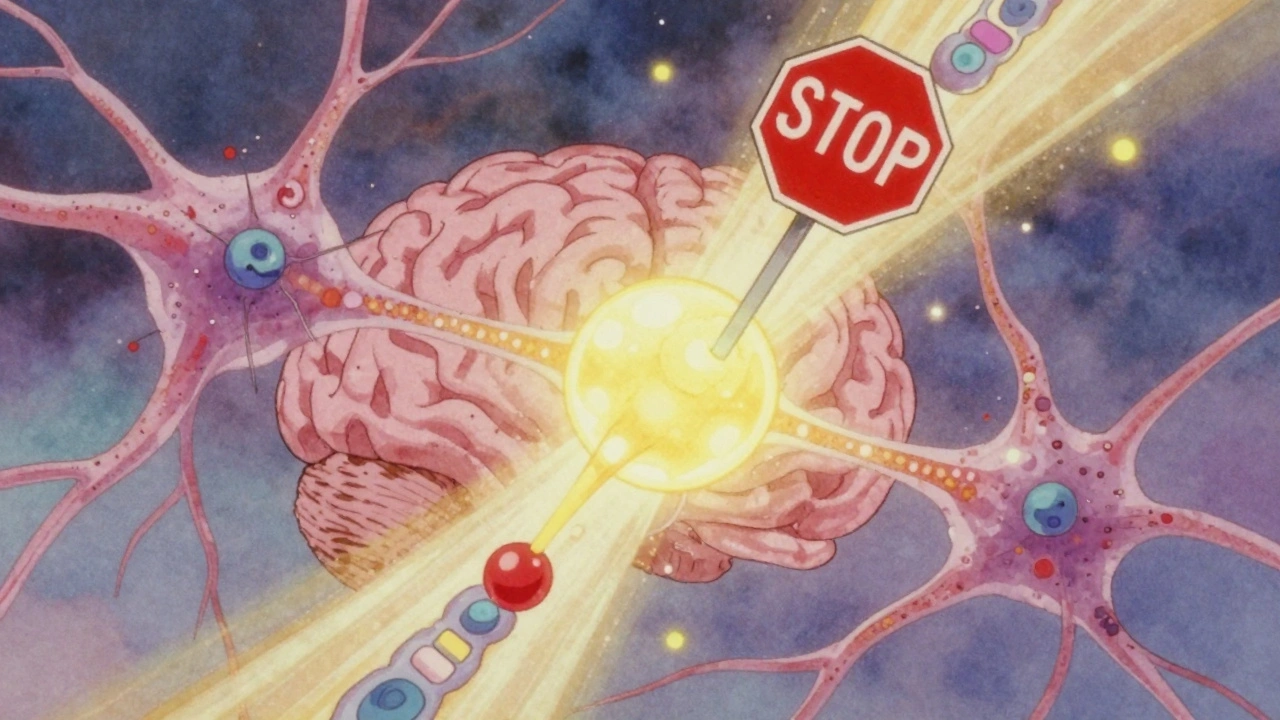
Serotonin is a chemical messenger, or neurotransmitter, that plays a big role in mood, sleep, appetite, and anxiety. When nerve cells send signals, they release serotonin into the space between them-the synaptic cleft. Normally, after the signal is sent, serotonin gets sucked back into the sending cell through a protein called the serotonin transporter (SERT). SSRIs block that transporter. Think of it like putting a stop sign on the serotonin’s way back home. More serotonin stays in the gap, giving your brain more of it to work with.
This doesn’t happen instantly. Within an hour, serotonin levels in the brain rise from about 0.1-0.5 nanomolar to 2-3 nanomolar. But you won’t feel better right away. It usually takes 4 to 6 weeks before you notice any real change in how you feel. Why the delay?
Scientists believe it’s because your brain needs time to adapt. Early on, extra serotonin triggers receptors that actually slow down serotonin production. But after 2-3 weeks, those receptors calm down. Then, your brain starts firing serotonin signals more strongly-by 40-60% in some areas. This is called autoreceptor desensitization. It’s not just about having more serotonin; it’s about your brain learning to use it better.
There’s also evidence SSRIs boost brain-derived neurotrophic factor (BDNF), a protein that helps brain cells grow and connect. After 8 weeks of treatment, responders show a 25-30% increase in BDNF levels. That’s not just mood repair-it’s brain repair.
The Six Main SSRIs You’ll Hear About
There are six SSRIs approved in the U.S. Each has slight differences in how long they last in your body and how they’re processed:
- Fluoxetine (Prozac) - Longest half-life (4-16 days). Often used for depression, OCD, and panic disorder. Less risk of withdrawal.
- Sertraline (Zoloft) - Most commonly prescribed first-line option. Good balance of effectiveness and tolerability.
- Escitalopram (Lexapro) - Active form of citalopram. Often rated highest for user satisfaction.
- Citalopram (Celexa) - Similar to escitalopram but slightly less potent.
- Paroxetine (Paxil) - Shortest half-life (21 hours). Higher risk of withdrawal symptoms.
- Fluvoxamine (Luvox) - Used mainly for OCD and social anxiety. Also has some effects on sigma receptors.
Doctors often start with sertraline or escitalopram because they’re well-tolerated and effective for most people. Doses vary: sertraline usually starts at 50 mg/day, escitalopram at 10 mg/day. Most people reach their full dose over 4-6 weeks.
Side Effects: What’s Common-and What’s Not
Side effects are the biggest reason people stop taking SSRIs. But not everyone gets them, and many fade within a few weeks.
Here’s what most people experience in the first 1-2 weeks:
- Nausea - Often mild and goes away. Taking the pill with food helps.
- Headache - Usually temporary.
- Insomnia or drowsiness - Depends on the drug. Fluoxetine can be stimulating; paroxetine can make you sleepy.
- Increased anxiety - Surprisingly common in the first 10-14 days. It’s not the drug making you worse-it’s your brain adjusting. Tell your doctor if it’s severe.
Longer-term side effects are more persistent:
- Sexual problems - Affects 40-60% of users. This includes reduced libido, trouble getting aroused, or delayed orgasm. It’s one of the most common reasons people quit. Escitalopram and sertraline tend to cause fewer sexual issues than paroxetine.
- Emotional blunting - Some people say they feel "numb" or like they’ve lost their edge. It’s not depression-it’s a dulling of emotions, both good and bad. Studies show about 42% of users report this.
- Weight gain - Occurs in about 25% of long-term users. Not everyone gains weight, and some SSRIs (like fluoxetine) are less likely to cause it.
Withdrawal symptoms (also called discontinuation syndrome) are real-and often misunderstood. If you stop suddenly, especially with short-acting SSRIs like paroxetine or sertraline, you might get:
- Dizziness
- "Brain zaps" (electric shock-like sensations)
- Flu-like symptoms
- Increased anxiety or mood swings
These aren’t addiction symptoms. They’re your nervous system reacting to the sudden drop in serotonin. The fix? Taper slowly under medical supervision. Never quit cold turkey.
Who Benefits Most-and Who Doesn’t
SSRIs work best for moderate to severe depression, panic disorder, OCD, social anxiety, and bulimia. They’re less effective for mild depression, where therapy or lifestyle changes might be enough.
But here’s the hard truth: about 30-40% of people don’t respond to their first SSRI. That doesn’t mean you’re broken. It means your brain chemistry might need a different approach. The STAR*D trial, the largest depression study ever done, found that only 28-33% of people went into remission with their first medication. Many needed to try two or three different drugs.
Some people respond better to other types of antidepressants. For example, MAOIs are more effective for atypical depression (characterized by oversleeping, overeating, and mood reactivity), but they require strict dietary rules. Newer drugs like vortioxetine or agomelatine may work better for some, but SSRIs still win on safety and cost.
Genetics might play a role too. A 2024 study found that certain versions of the SLC6A4 gene predict SSRI response with 78% accuracy. That means someday, doctors might test your DNA before prescribing. Right now, it’s trial and error.
The Controversy: Is the Serotonin Theory Even True?
For decades, we’ve been told depression is caused by low serotonin. That’s why SSRIs make sense-they boost serotonin, so you feel better.
But recent science challenges that idea. Dr. David Nutt and others point out that only 25-30% of depressed patients actually have low serotonin levels. Some people with normal serotonin still respond to SSRIs. Others with low serotonin don’t improve.
So why do SSRIs work if the theory is flawed? The answer might be simpler: it doesn’t matter how they work-just that they do. We’ve known for years that drugs like aspirin relieve pain without fully understanding the mechanism. The same might be true for SSRIs.
What we do know is this: SSRIs change brain activity in measurable ways. Brain scans show that after successful treatment, the subcallosal cingulate cortex-a region linked to sadness and rumination-becomes less overactive. That’s real, physical change. Whether it’s serotonin, BDNF, or something else, the brain is rewiring.
Real Stories: What People Actually Experience
On forums like Reddit and HealthUnlocked, users share honest experiences:
- "Fluoxetine gave me back my ability to feel emotions after 3 months. I cried for the first time in years-not from sadness, but from relief."
- "Sertraline cut my panic attacks from daily to once every few weeks. I started going out again."
- "Paroxetine wrecked my sex life. When I tried to quit, I had brain zaps for three months. I wish I’d been warned."
Consumer Reports rated SSRIs 3.4 out of 5. Escitalopram got the highest score (3.7), paroxetine the lowest (3.1). The biggest complaints? Sexual side effects and withdrawal.
But for many, the trade-off is worth it. One user wrote: "I was suicidal. After 6 weeks on sertraline, I didn’t want to die anymore. That’s all that mattered."
What to Do If You’re Starting an SSRI
If your doctor suggests an SSRI, here’s what to keep in mind:
- Give it time. Don’t judge it after 1 week. Wait at least 4-6 weeks before deciding if it’s working.
- Track your symptoms. Use a simple journal: rate your mood, sleep, energy, and anxiety on a scale of 1-10 each week.
- Don’t panic about side effects. Nausea and anxiety often fade. Talk to your doctor before stopping.
- Never stop suddenly. Taper slowly, even if you feel fine.
- Combine with therapy. SSRIs work better with counseling. CBT, in particular, helps rewire negative thought patterns.
And remember: if one SSRI doesn’t work, it’s not a failure. It’s data. Your next option might be another SSRI, a different class of antidepressant, or a non-medication approach. There’s no single right answer.
Final Thoughts: SSRIs Are Tools, Not Cures
SSRIs aren’t perfect. They come with side effects. They don’t work for everyone. And the science behind them is still evolving.
But for millions, they’ve been a lifeline. They don’t make you happy. They don’t fix your life. But they can give you the mental space to start fixing it yourself.
They’re not the end of the journey. They’re just one step. And sometimes, that’s enough.
How long does it take for SSRIs to start working?
Most people start noticing small improvements after 2-4 weeks, but full effects usually take 4-6 weeks. Some may need up to 8-12 weeks to feel the full benefit. It’s important to stick with the medication even if you don’t feel better right away.
Can SSRIs cause weight gain?
Yes, about 25% of long-term users experience weight gain. This is more common with paroxetine and citalopram. Fluoxetine is less likely to cause it. Weight changes often stabilize after the first few months. Diet, exercise, and monitoring your intake can help manage this side effect.
Do SSRIs cause addiction?
No, SSRIs are not addictive. You won’t crave them or need higher doses to get the same effect. But stopping suddenly can cause withdrawal symptoms like dizziness, brain zaps, or nausea. That’s not addiction-it’s your nervous system adjusting. Always taper off under medical supervision.
Why do SSRIs cause sexual side effects?
Serotonin plays a role in sexual response. Increasing serotonin levels can reduce libido, delay orgasm, or make it harder to get aroused. This affects 40-60% of users. Some SSRIs, like escitalopram and sertraline, have lower rates than others. If this is a major issue, talk to your doctor about adjusting the dose or switching medications.
Are SSRIs safe for teenagers?
SSRIs are approved for teens with depression and OCD, but they carry a FDA black box warning for increased suicidal thoughts in people under 25, especially in the first few weeks. This doesn’t mean they’re dangerous-it means close monitoring is essential. Regular check-ins with a doctor during the first month are critical.
Can I drink alcohol while taking SSRIs?
It’s not recommended. Alcohol can worsen depression and anxiety symptoms. It also increases drowsiness and dizziness, especially when combined with SSRIs. Even moderate drinking can reduce the effectiveness of the medication. If you choose to drink, do so very sparingly and talk to your doctor first.
What’s the difference between generic and brand-name SSRIs?
There’s no meaningful difference in effectiveness. Generic SSRIs contain the same active ingredient as brand names like Prozac or Zoloft. The FDA requires them to be bioequivalent. The main difference is cost-generics are often 80-90% cheaper. In the U.S., over 90% of SSRI prescriptions are for generics.

Ernie Blevins
December 7, 2025 AT 07:52SSRIs are just chemical crutches. People don't need pills to feel better, they need to get off the couch and stop being so soft. I took one once for a week and felt like a zombie. Quit cold turkey. No big deal.
Ted Rosenwasser
December 9, 2025 AT 04:29Let’s be clear: the serotonin hypothesis is a 1980s marketing ploy invented by Big Pharma to sell pills to people who just need to meditate or read Nietzsche. The fact that SSRIs work despite being based on a debunked theory is either a miracle or proof that neuroscience is still in the Stone Age. BDNF? Autoreceptor desensitization? Sounds like jargon dressed up as science.
Helen Maples
December 9, 2025 AT 21:15People need to stop dismissing side effects as 'just temporary.' Sexual dysfunction isn't something you 'get used to'-it's a life-altering consequence. And emotional blunting? That's not 'adjusting,' that's losing your humanity. If your doctor says 'it's normal,' ask for a second opinion. Your feelings matter more than their convenience.
Ashley Farmer
December 10, 2025 AT 07:33I’ve been on escitalopram for 3 years. The first month was hell-nausea, anxiety, crying for no reason. But after 6 weeks, I woke up and realized I hadn’t thought about killing myself in 10 days. That’s not magic. That’s science. I still have bad days, but now I have the space to deal with them. You’re not broken if it doesn’t work right away. You’re just human.
David Brooks
December 10, 2025 AT 15:15THIS. THIS IS THE TRUTH. I was suicidal. I couldn’t hold a job. I didn’t recognize my own face in the mirror. Then I took sertraline. Six weeks later, I cried because I saw a sunset and it made me feel something. Not happy. Not fixed. But alive. SSRIs didn’t cure me. They gave me the chance to save myself. And if you think that’s not worth it, you’ve never been that deep in the dark.
Nicholas Heer
December 10, 2025 AT 17:51SSRIs are part of the New World Order brainwash program. The FDA, WHO, and Big Pharma are pushing these to make people docile. Did you know the original SSRI trials were funded by pharmaceutical lobbyists? And those 'brain zaps'? That’s not withdrawal-that’s electromagnetic interference from 5G towers messing with your neurotransmitters. They don’t want you to know this. But now you do.
Sam Mathew Cheriyan
December 12, 2025 AT 09:05Bro in USA think SSRIs are magic. In India, we use yoga, turmeric, and chanting. No pills needed. SSRIs only work because people believe in them. Placebo effect. 100%. Also, why do Americans take so many pills? We eat spicy food and still live to 90. You guys are weak.
Nancy Carlsen
December 13, 2025 AT 05:05Just wanted to say thank you to everyone sharing their stories. It’s scary to start one of these meds. I was terrified of the sexual side effects, but I talked to my therapist first and we made a plan. Now I’m 8 months in and my anxiety is under control. It’s not perfect, but I’m here. And that’s enough. You’re not alone.
Jennifer Anderson
December 13, 2025 AT 10:41took lexapro for 2 years. lost 15 lbs cause i stopped eating. then i got my sex drive back after switching to zoloft. dont let anyone tell you its one size fits all. listen to your body. and if your doc doesnt listen? find a new one. your mental health is worth it.