When you can’t sleep, your mind doesn’t rest. It races. It replays mistakes. It dreads tomorrow. For millions with depression or anxiety, insomnia isn’t just a side effect-it’s the engine driving the whole cycle. And treating it? That’s not an add-on. It’s often the key that unlocks recovery.
Why Insomnia Isn’t Just a Symptom
For years, doctors treated insomnia as a side effect of depression or anxiety. Sleep trouble? Give an antidepressant. Anxiety? Try a sedative. But research now shows that’s like trying to fix a leaky roof by mopping the floor. The real problem is still there. Insomnia is defined as trouble falling or staying asleep at least three nights a week for three months-even when you have the chance to sleep. And it’s not rare. Around 10 to 15% of adults in the U.S. meet the full diagnosis. During the pandemic, that number jumped. By 2021, one in three people reported clinical insomnia symptoms-more than double pre-pandemic levels. Here’s the critical part: people with chronic insomnia are 40 times more likely to develop severe depression than those who sleep well. That’s not correlation. That’s causation. Studies using genetic data (Mendelian randomization) confirm that poor sleep doesn’t just follow depression-it actually causes it to develop and worsen. The same goes for anxiety. Nighttime worry fuels hyperarousal. Your body stays stuck in fight-or-flight mode. Cortisol and other stress hormones stay high. Your brain doesn’t get the reset it needs. And without that reset, anxiety tightens its grip.CBT-I: The Gold Standard That Actually Works
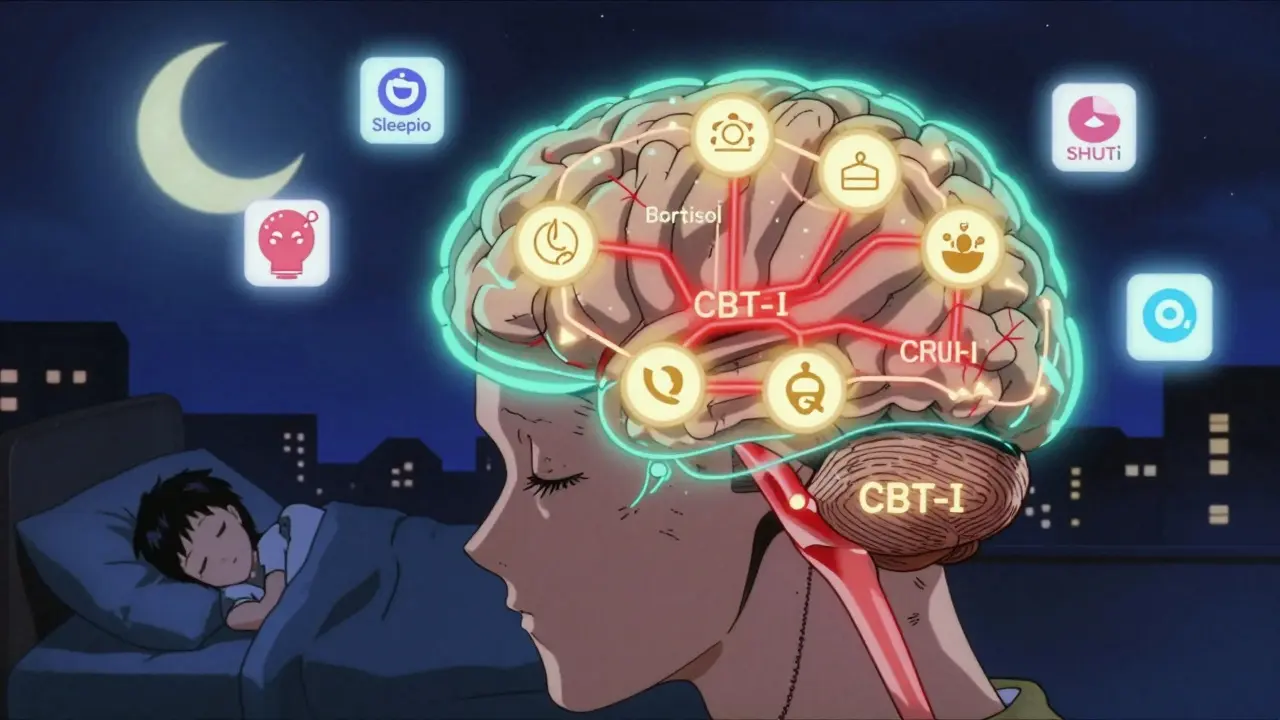
There’s one treatment that stands above all others for insomnia linked to depression and anxiety: Cognitive Behavioral Therapy for Insomnia, or CBT-I. Unlike sleeping pills, CBT-I doesn’t just mask symptoms. It rewires the thoughts and behaviors keeping you awake. It’s structured, evidence-based, and backed by over 180 studies. A 2023 review in Sleep journal analyzed 186 trials and found that CBT-I doesn’t just help you sleep-it lowers your risk of developing major depression. Here’s how it works in six core parts:- Stimulus control: Your bed is only for sleep and sex. No scrolling, no worrying, no watching TV. If you’re not asleep in 20 minutes, get up. Return only when sleepy.
- Sleep restriction: You’re not sleeping 8 hours? Then don’t spend 8 hours in bed. Reduce time in bed to match your actual sleep. It’s uncomfortable at first-but it rebuilds sleep pressure.
- Relaxation techniques: Diaphragmatic breathing, progressive muscle relaxation. These lower heart rate and quiet the nervous system.
- Cognitive therapy: Challenge thoughts like “I’ll never sleep again” or “If I don’t sleep 8 hours, I’ll collapse tomorrow.” These beliefs keep your brain on high alert.
- Sleep hygiene: Consistent wake-up times, avoiding caffeine after noon, limiting screens before bed. Not magic, but necessary.
- Sleep diary tracking: Writing down sleep patterns helps spot triggers and track progress.
How CBT-I Changes Your Brain
It’s not just “thinking differently.” CBT-I changes your biology. People with depression and insomnia show overactive stress systems. Their hypothalamic-pituitary-adrenal (HPA) axis-your body’s alarm system-is stuck on high. Levels of CRH, ACTH, and cortisol stay elevated, even at night. This keeps you wired, even when you’re exhausted. CBT-I brings these levels down. One 2025 study in Frontiers in Psychiatry found that after CBT-I, stress hormone patterns normalized in patients with comorbid depression and insomnia. That’s not a coincidence. Better sleep = less biological stress = less depression. And it’s not just about hormones. CBT-I helps rebuild the brain’s sleep-wake rhythm. It restores circadian timing. It reduces nighttime hyperarousal. It teaches your brain that bed = safety, not stress.
Why Medications Fall Short
Pills like zolpidem (Ambien) or benzodiazepines can help you fall asleep faster. But they don’t fix the root problem. They’re like putting a bandage on a broken bone. A 2025 study in Nature Scientific Reports compared CBT-I and zolpidem. Both improved sleep and mood in the short term. But after six months, only the CBT-I group stayed better. The zolpidem group bounced back to their old patterns. Why? Because pills don’t change beliefs. They don’t teach you how to handle nighttime worry. They don’t reset your sleep drive. And they come with risks-dependence, grogginess, falls in older adults. CBT-I has no side effects. No withdrawal. No tolerance. Just lasting change.Real Results: Numbers That Matter
The data doesn’t lie:- CBT-I reduces depression symptoms as much as antidepressants-sometimes more. A 2018 meta-analysis found an effect size of -1.29 on the Hamilton Depression Scale. That’s a large, clinically meaningful drop.
- People who fully recover from insomnia during CBT-I cut their risk of future depression by 83%. Those who didn’t fully recover still cut risk by 41%.
- When CBT-I is added to antidepressant treatment, remission rates for depression jump 40% compared to medication alone.
- For every $1 spent on CBT-I, you save $2.50 to $3.50 in reduced healthcare visits, disability claims, and lost work days.
Barriers to Getting Help
So why isn’t everyone getting CBT-I? Because access is broken. Only 1 to 2% of people with insomnia get CBT-I. Why? Few therapists are trained. Insurance rarely covers it. Many providers still think “just take a pill.” In the U.S., only about 5% of psychologists have formal CBT-I training. And even when it’s available, patients struggle to stick with it. About 65-75% feel worse in the first two weeks because sleep restriction makes them tired. But if they push through, 70-80% see big gains. Digital CBT-I is changing that. Apps like Sleepio have over 150,000 users. Of those, 76% had a clinically meaningful drop in insomnia severity. And telehealth use jumped 300% between 2019 and 2022. Kaiser Permanente started screening all depression patients for insomnia in 2022. Since then, relapse rates dropped 22%. That’s not just good for patients-it’s good for the system.What to Do If You’re Struggling
If you have depression or anxiety and can’t sleep:- Don’t assume it’s just part of your illness. Insomnia is a treatable condition on its own.
- Ask your doctor for a referral to CBT-I. Look for a sleep psychologist or therapist trained in CBT-I.
- If in-person therapy isn’t available, try a digital CBT-I program. Sleepio, SHUTi, and CBT-I Coach are all clinically validated.
- Track your sleep. Use a notebook or app. Note bedtime, wake time, how long it took to fall asleep, and nighttime awakenings.
- Be patient. The first two weeks are hard. Sleep restriction feels brutal. But that’s when the brain starts relearning.
- Don’t quit. Stick with it for at least 6 weeks. The biggest gains come after the discomfort.
The Bigger Picture
Sleep isn’t a luxury. It’s the foundation of mental health. You can’t heal anxiety or depression if your brain never gets a chance to reset. Treating insomnia isn’t a side project. It’s the most powerful, cost-effective, and lasting intervention we have for depression and anxiety. It doesn’t replace therapy or medication-it makes them work better. The science is clear. The tools exist. The only thing missing is access. We need to stop treating sleep as an afterthought. Start treating it like the lifeline it is.Can treating insomnia help with depression even if I’m not sleeping perfectly?
Yes. Even partial improvement in sleep can lead to noticeable mood gains. Research shows that people who reduce their insomnia severity by half-without full remission-still cut their risk of depression relapse by 41%. You don’t need 8 hours of perfect sleep to feel better. Just consistent, deeper sleep for a few nights a week can shift your brain’s stress response.
Is CBT-I better than antidepressants for sleep problems in depression?
For insomnia specifically, CBT-I is more effective than any medication, including antidepressants. Antidepressants may help mood but often don’t fix sleep-and some, like SSRIs, can actually worsen insomnia. CBT-I targets the root causes of poor sleep: racing thoughts, bad habits, and fear of not sleeping. Studies show CBT-I reduces insomnia severity twice as much as antidepressants alone. When combined, they work even better.
How long does it take for CBT-I to work?
Most people start seeing changes in 2 to 4 weeks. Sleep efficiency (time asleep vs. time in bed) usually improves first. Mood improvements often follow within 4 to 6 weeks. But the real benefit comes after 8 weeks-when new sleep habits become automatic. The hardest part is the first 10 days, when sleep restriction makes you tired. That’s normal. It’s the brain adjusting. Stick with it.
Can I do CBT-I on my own with an app?
Yes. Digital CBT-I programs like Sleepio and SHUTi have been tested in clinical trials and show results nearly equal to in-person therapy. They follow the same evidence-based protocol: stimulus control, sleep restriction, cognitive restructuring, and relaxation. The key is consistency. Use the app daily, complete sleep diaries, and don’t skip sessions. Many users report better sleep and lower anxiety within 6 weeks.
Why isn’t CBT-I more widely available if it’s so effective?
Mainly because of training gaps and insurance barriers. Very few therapists are trained in CBT-I-it’s not part of most psychology programs. Insurance companies often won’t cover it unless you have a sleep disorder diagnosis. Many providers still default to prescribing pills because it’s faster and easier. But that’s changing. More clinics and telehealth platforms are now offering CBT-I, and research is pushing for it to become a standard part of depression care.
What if CBT-I doesn’t work for me?
About 30-40% of people don’t fully recover from insomnia with CBT-I alone. That doesn’t mean it failed-it means you might need a different approach. Some benefit from combining CBT-I with medication (like low-dose trazodone) for short-term help. Others need more intensive therapy or treatment for underlying conditions like sleep apnea or restless legs. Talk to your provider. There’s no one-size-fits-all. But don’t give up on treating sleep-it’s still your best starting point.


anthony epps
December 15, 2025 AT 05:56Been sleeping like crap since the pandemic. Tried melatonin, valerian, even that weird weighted blanket. Nothing worked until I tried Sleepio. First two weeks felt like hell, but now I’m actually sleeping. No pills. No magic. Just science.
Dylan Smith
December 16, 2025 AT 04:06I used to think insomnia was just me being weak. Like if I just tried harder I’d fall asleep. Turns out my brain was wired wrong. CBT-I didn’t fix me overnight but it gave me back my life. No more 3am panic spirals. Just quiet. Finally.
Tiffany Machelski
December 16, 2025 AT 23:53my dr said just take ambien. i said no thanks. i dont wanna be one of those people who cant sleep without pills. cbt-i is the real deal. i did it through my insurance and it changed everything. thanks for posting this.
James Rayner
December 17, 2025 AT 00:43There’s something deeply spiritual about sleep, isn’t there? It’s not just biology-it’s the soul’s nightly reset. When we deny ourselves rest, we’re not just tired-we’re spiritually fractured. CBT-I doesn’t just retrain your brain; it restores your inner rhythm. And in a world that glorifies burnout, that’s revolutionary.
Souhardya Paul
December 18, 2025 AT 05:00For anyone thinking about CBT-I: don’t wait until you’re at rock bottom. I started because I was falling asleep at my desk. Six weeks in, I felt like a new person. My anxiety didn’t vanish, but it lost its power. And the best part? I didn’t need to change my whole life-just my bedtime habits. Small shifts, huge results.
Josias Ariel Mahlangu
December 18, 2025 AT 15:35This is why America is falling apart. People used to tough it out. Now we need apps and therapists just to sleep. Weakness is being marketed as a medical condition. Take a pill or deal with it. Stop treating sleep like it’s some sacred ritual.
Andrew Sychev
December 18, 2025 AT 20:43CBT-I? Yeah right. They’re just pushing this because Big Pharma hates it. Sleepio? That’s owned by a tech conglomerate that sells your data. They don’t care if you sleep-they care if you click. Wake up. This is all a distraction. Real healing is in nature, fasting, and silence. Not apps.
Dan Padgett
December 20, 2025 AT 06:28Back home in Nigeria, we say 'the night is not your enemy'. But here, people treat sleep like a task to optimize. CBT-I feels like therapy for your soul’s clock. I tried it after my cousin died-couldn’t sleep for months. The sleep diary? Made me realize I was punishing myself with screens. Changed my whole relationship with night.
Hadi Santoso
December 22, 2025 AT 01:37Just finished CBT-I through my VA health. Best thing I’ve done since coming home. I used to lie there thinking about IEDs and loud noises. Now I just… rest. No meds. No guilt. Just quiet. If you’re military or a veteran and struggling-ask for CBT-I. They’ll help you. It’s not weakness. It’s wisdom.
Arun ana
December 23, 2025 AT 00:02Been doing CBT-I for 3 weeks. Still tired. Still wake up at 2am. But now I’m not panicking. I just breathe and read. No phone. No stress. And that’s progress. I’m not fixed, but I’m not falling apart either. 🙏
Kayleigh Campbell
December 23, 2025 AT 18:04So let me get this straight. We spent decades telling people to 'just sleep better'... and now we’re surprised that people need a 6-week app to unlearn trauma? 🤦♀️ We’re not broken. We’re just exhausted by a system that treats rest like a luxury. CBT-I isn’t the solution-it’s the bare minimum.
Dave Alponvyr
December 24, 2025 AT 15:07My therapist said CBT-I was the only thing that actually works. I didn’t believe her. Now I’m the one telling everyone else. First two weeks? Brutal. After that? Life-changing. No drama. No hype. Just sleep.
Cassandra Collins
December 24, 2025 AT 23:02Did you know the government is using sleep tracking to monitor your stress levels? Sleepio is a spy tool. They’re collecting your sleep data to predict depression before you even feel it. That’s why they’re pushing it so hard. Wake up. This isn’t healthcare. It’s surveillance.
James Rayner
December 25, 2025 AT 15:42That’s a terrifying thought… but also not entirely false. Data is the new oil, and sleep is the new frontier. But that doesn’t make CBT-I less valid. If anything, it makes it more urgent. We need to reclaim our rest-not from Big Tech, but from the idea that we’re disposable. The app helps. The movement? That’s on us.