When medicines vanish and prices spike
It started with insulin. Then came the antibiotics. By late 2021, hospital pharmacists in Bristol were calling suppliers three times a week just to confirm if a basic drug was in stock. One nurse told me she had to switch 12 patients off their usual blood pressure pill because the batch had been out of stock for 11 weeks. This wasn’t a glitch. It was a pattern. Across the UK, the US, and Europe, essential medicines, medical devices, and even simple supplies like IV bags began disappearing from shelves. At the same time, prices for what was still available jumped - sometimes by 30%, 50%, even 100% in a single year.
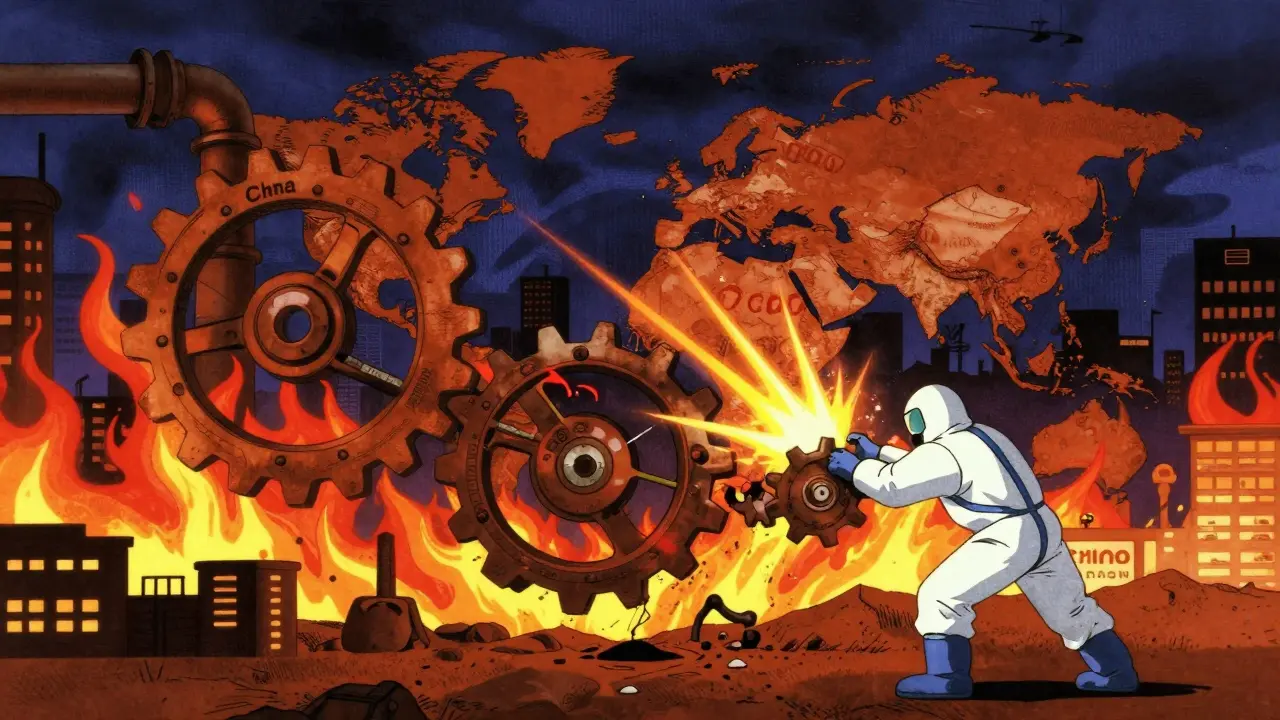
What happened? Two things crashed into each other: pricing pressure and shortages. They didn’t just happen together. They fed each other. When factories couldn’t make enough, prices rose. When prices rose too fast, governments stepped in to cap them. That made shortages worse. And when shortages got worse, prices rose again. It was a loop - and healthcare felt it hardest.
Why did this happen? It wasn’t just the pandemic
People blame the pandemic, and yes, lockdowns broke global supply chains. But that’s only half the story. The real problem was how fragile the system was to begin with. For years, hospitals and drugmakers had been chasing efficiency. They cut inventory. They relied on single suppliers - often in just one country. When China shut down in early 2020, 80% of the world’s active pharmaceutical ingredients came from there. No backup. No buffer. One shock, and the whole chain snapped.
Then came the energy crisis. In 2021, UK wholesale gas prices hit £200 per therm. Pre-pandemic? £40. That didn’t just raise heating bills. It made factories that produce medicines - which need heat, power, and chemicals - suddenly unprofitable. A single chemical plant in Germany shut down for three months because it couldn’t afford the gas. That one plant supplied 40% of Europe’s heparin, a blood thinner used in every ICU. Suddenly, hospitals were rationing it.
And then there was labor. The Federal Reserve found that through mid-2022, the US labor force was still 1.5 percentage points smaller than before the pandemic. That meant fewer workers to pack pills, drive delivery trucks, or test medical devices. One UK medical distributor told me they lost 18% of their warehouse staff in 18 months. They couldn’t hire replacements. So they cut shifts. Inventory piled up. Orders went unfulfilled.
Price caps made things worse - and here’s why
The UK government capped energy prices to protect households. It sounded fair. But when energy companies couldn’t pass on rising costs, they started losing money. Between August and December 2021, 27 small energy providers collapsed. The same thing happened in pharma.
When the NHS set fixed prices for certain drugs, manufacturers had two choices: absorb the loss or stop making them. Most chose to stop. A 2022 study by the Office for Budget Responsibility found that price controls led to a 19% drop in the number of generic drugs available in the UK within 12 months. Patients didn’t just pay more - they often got nothing.
Harvard economist Martin Weitzman called this "shortage deformation." When prices are held artificially low, people don’t just buy what they need. They hoard. A Reddit thread from September 2021 described how Tesco’s freezer aisles stayed empty for weeks because families were buying 3-4 packs of insulin instead of one. The system didn’t break because there wasn’t enough. It broke because demand surged when people feared there wouldn’t be any.
Who got hit hardest? The sick, the poor, and the elderly
Not everyone felt this equally. People with chronic conditions - diabetes, heart disease, asthma - were the most vulnerable. If your medication runs out, you don’t wait for a sale. You need it now. One 72-year-old in Bristol told me she skipped her heart medication for three weeks because her pharmacy ran out and the next batch wasn’t due for six weeks. She ended up in A&E with atrial fibrillation.
Small clinics and care homes suffered too. Big hospitals could negotiate bulk deals. Smaller providers couldn’t. A GP practice in Bath reported that in Q3 2022, they had to delay 34% of non-emergency prescriptions because suppliers couldn’t guarantee delivery. That meant patients waited. Worsened. Got sicker.
And then there’s the hidden cost: time. Nurses spent hours tracking down drugs. Pharmacists called 10 suppliers for one order. Doctors changed treatment plans on the fly. All of that adds up. The Cleveland Federal Reserve found that supply shocks reduce employment by 0.15% - but in healthcare, that’s not just jobs lost. It’s care delayed, lives at risk.
What’s changing? And what’s not
By early 2023, things started to ease. The Global Supply Chain Pressure Index - a measure of disruptions - returned to pre-pandemic levels. Inflation in the US fell from 9.1% in June 2022 to 3.0% by June 2023. That’s good news. But don’t mistake it for recovery.
Many shortages are still lingering. The World Trade Organization says global trade volumes in 2021 were 2.5 percentage points lower than they could have been because of supply issues. And the International Monetary Fund warns that supply chain pressures will stay 15-20% above normal through 2025. Why? Geopolitical tension. Climate disruptions. China’s shifting policies. All of it makes the system less predictable.
Some companies are adapting. McKinsey found that firms using dual sourcing - buying from two different suppliers - recovered from disruptions 35% faster. Others are investing in digital tools that track inventory in real time. One UK hospital network cut stockouts by 28% after installing a system that alerts them when a drug is running low.
But structural fixes are slow. The UK government still doesn’t require drugmakers to maintain minimum stockpiles. The NHS still pays fixed prices for generics. And most hospitals still rely on just-in-time delivery - a system that works perfectly until it doesn’t.

What’s next? The new normal in health economics
There’s no going back to the way things were. The old model - cheap, efficient, global - is broken. The new model will be more expensive. More local. More resilient.
Companies are already moving. Goldman Sachs predicts that by 2025, 60% of global health firms will use "digital twin" simulations to test how their supply chains react to shocks. That means fewer surprises. But it also means higher costs - 8-12% more, by some estimates.
Policy makers are starting to wake up. Germany relaxed competition rules in 2021 to let pharmaceutical companies share inventory during shortages. It cut shortages by 19% in six weeks. The EU approved €1.8 trillion in aid for energy-intensive industries. The US fined ocean freight companies for price gouging.
But the biggest change won’t come from regulations. It’ll come from recognition: healthcare isn’t a commodity. It’s a lifeline. And when lifelines break, you don’t fix them with cost-cutting. You fix them with foresight.
What you can do - even if you’re not a policymaker
If you’re a patient, keep a 14-day supply of essential meds on hand. Not to hoard. Just to buffer against delays. Talk to your pharmacist. Ask if your drug has alternatives. If your GP prescribes a generic, ask if it’s from a reliable source.
If you’re a caregiver or family member, track delivery times. If a prescription is late, call the pharmacy early. Don’t wait until the last day.
If you work in healthcare, push for visibility tools. Ask your hospital to map its supply chain. Know where your drugs come from. Who makes them? Where are the backups?
These aren’t big changes. But in a system that’s been brittle for years, small actions add up. The next crisis won’t be a surprise. It’ll be a warning. And we’ll be ready - or we won’t.


Thomas Anderson
December 15, 2025 AT 11:05Edward Stevens
December 17, 2025 AT 05:54Alexis Wright
December 18, 2025 AT 02:06Daniel Wevik
December 18, 2025 AT 04:17Rich Robertson
December 19, 2025 AT 10:12Natalie Koeber
December 20, 2025 AT 06:16Rulich Pretorius
December 21, 2025 AT 00:44Wade Mercer
December 21, 2025 AT 07:20Dwayne hiers
December 22, 2025 AT 17:32Jonny Moran
December 23, 2025 AT 11:02