Every year, millions of people on warfarin reach for an OTC cold medicine when they feel under the weather. They think it’s harmless-just a cough drop or a decongestant. But for someone taking warfarin, that small decision can send their INR skyrocketing, leading to internal bleeding, emergency room visits, or worse. This isn’t theoretical. It’s happening right now, in kitchens and pharmacies across the country.
Why Warfarin Is So Sensitive
Warfarin isn’t like other medications. It has a narrow window where it works safely. Too little, and you risk a stroke or clot. Too much, and you could bleed internally without warning. Most people on warfarin need their INR kept between 2.0 and 3.0. For some, like those with mechanical heart valves, it’s even tighter: 2.5 to 3.5. Even a small change in how your body processes warfarin can push you out of that range.The drug works by blocking vitamin K, which your body needs to make clotting factors. But it doesn’t take much to throw that balance off. Many OTC cold medicines interfere with how warfarin is broken down in your liver-or they add their own bleeding risk on top of it.
The Most Dangerous OTC Ingredients
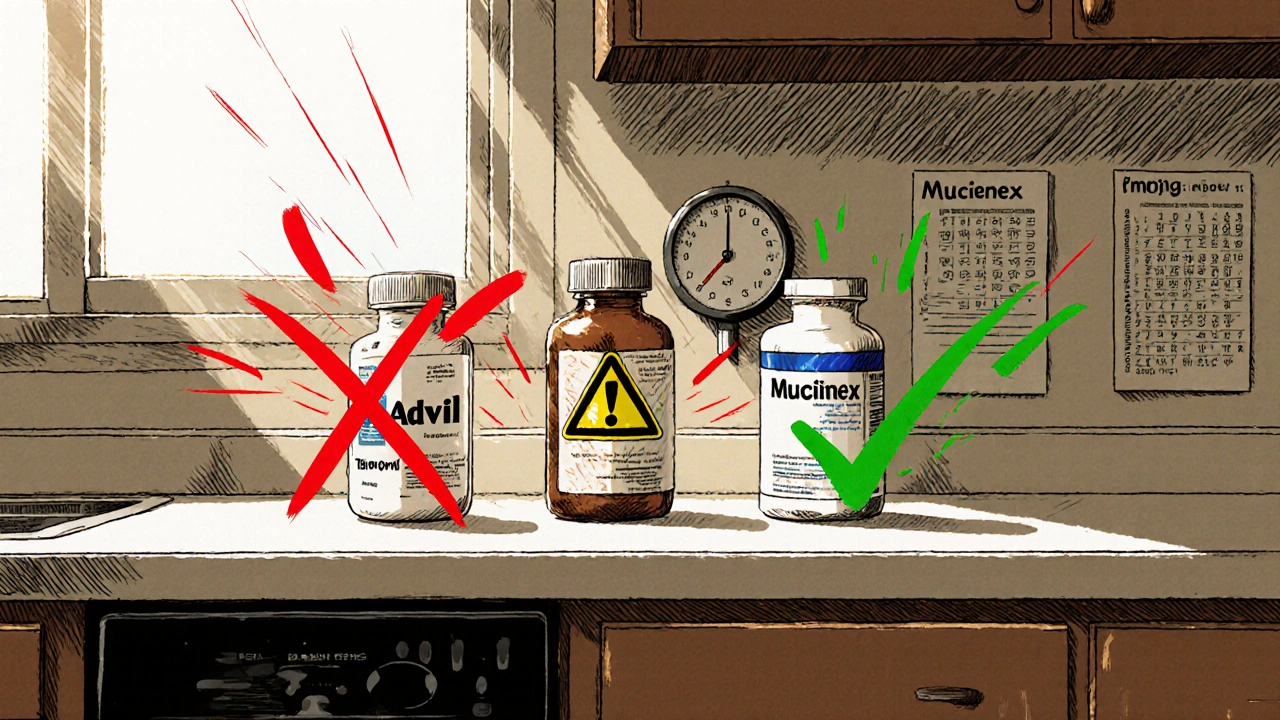
Not all cold meds are created equal. Some are safe. Others are ticking time bombs. Here’s what you need to avoid:- NSAIDs-ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin (Bayer, Excedrin). These don’t just thin your blood-they irritate your stomach lining. When combined with warfarin, the risk of gastrointestinal bleeding jumps by 4.5 times. Even "aspirin-free" products like Doan’s Pills contain magnesium salicylate, which does the same damage.
- Acetaminophen (Tylenol)-it’s often called the "safe" choice, but only if you stay under 2,000 mg per day. Taking more than that for three days straight can impair platelet function and raise bleeding risk. That’s easy to do if you’re taking multiple cold products that all contain acetaminophen.
- Cimetidine (Tagamet)-this heartburn med might seem unrelated, but it slows down how your liver breaks down warfarin. That can cause warfarin levels to spike by 30-50%.
- Quinidine-sometimes added to cough syrups like certain versions of Robitussin. It boosts warfarin levels by 25%.
- St. John’s wort, ginkgo biloba, and fish oil-these supplements aren’t OTC drugs, but people take them without realizing they’re dangerous. St. John’s wort cuts warfarin’s effectiveness by half. Ginkgo and fish oil increase bleeding risk by more than double.
What’s Actually Safe
You don’t have to suffer through a cold untreated. There are safe options-if you know what to look for.- Pseudoephedrine (Sudafed) and phenylephrine (Sudafed PE)-both are safe decongestants at standard doses. No known interaction with warfarin.
- Diphenhydramine (Benadryl) and chlorpheniramine (Chlor-Trimeton)-first-gen antihistamines. Safe for allergy and cold symptoms.
- Cetirizine (Zyrtec) and loratadine (Claritin)-second-gen antihistamines. Also safe, and less likely to cause drowsiness.
- Guaifenesin (Robitussin, Mucinex)-an expectorant that helps loosen mucus. No interaction with warfarin when used as directed.
Here’s the catch: You can’t trust the product name. A bottle labeled "Cold & Flu Relief" might have three different active ingredients. One might be safe. The others? Not so much.
How to Read Labels Like a Pro
The FDA now requires OTC products with NSAIDs to say "Do not use if taking blood thinners" in bold on the front. But that’s not enough. Many people still miss it.Here’s how to read a label correctly:
- Look at the "Active Ingredients" section-ignore the brand name and marketing claims.
- Check every ingredient. If you see acetylsalicylic acid, ibuprofen, naproxen, or magnesium salicylate-put it back.
- Don’t assume "non-drowsy" or "alcohol-free" means safe. Those labels tell you nothing about warfarin interactions.
- Check for acetaminophen in multiple products. If you’re taking a cold tablet and a separate pain reliever, you could hit 3,000 mg without realizing it.
One user on r/bloodthinners shared that after taking two doses of Theraflu-containing acetaminophen and phenylephrine-his INR jumped from 2.4 to 6.1 in 72 hours. He ended up in the hospital. He thought he was being careful. He wasn’t.
What to Do Before You Take Anything
The American College of Chest Physicians and the Anticoagulation Forum both agree: Always check with your anticoagulation clinic before taking any new medication-even if it’s sold over the counter.Here’s what works in real life:
- Get a personalized "Medication Safety Card" from your clinic. It lists safe and unsafe OTC options for you.
- Use a pharmacy app like Mayo Clinic’s "Warfarin Watch"-scan the barcode of any OTC product before buying. It flags dangerous combinations in seconds.
- Ask your pharmacist: "Is this safe with warfarin?" Don’t assume they’ll know unless you ask.
- Keep a log. Write down every OTC product you take, the date, and your INR reading after. Patterns show up fast.
Patients who complete a 90-minute "OTC Medication Safety" workshop reduce bad choices by 78%. That’s not luck. That’s education.

The Bigger Picture
You might think this is just about cold season. But it’s not. Warfarin users are at risk year-round. Every new supplement, every change in diet, every OTC purchase adds up. In 2023, 28% of warfarin-related hospitalizations came from OTC meds alone. That’s preventable.And it’s getting worse. With more multi-symptom products on the market, and fewer people reading labels, the risk is rising. Even new FDA rules-like requiring warning labels on NSAIDs-aren’t enough if patients don’t understand what they mean.
There’s hope, though. Pharmacogenetic testing can now tell you if you’re genetically more likely to have bad reactions to warfarin. People with certain CYP2C9 or VKORC1 gene variants break down the drug slower. That means even small doses of OTC meds can be dangerous. But only 18% of patients get tested-mostly because insurance won’t cover it.
Your Action Plan
If you’re on warfarin, here’s what to do right now:- Go through your medicine cabinet. Toss anything with NSAIDs, high-dose acetaminophen, or cimetidine.
- Call your anticoagulation clinic. Ask for a list of safe OTC cold meds. Get a Medication Safety Card.
- Download a barcode scanner app like Warfarin Watch. Use it every time you buy something.
- When you feel sick, don’t guess. Call your pharmacist or clinic first.
- Teach someone in your household how to read labels. You might not be thinking clearly when you’re sick.
There’s no magic pill. But there’s a simple rule: Never take anything new without checking. Your life depends on it.
Can I take Tylenol while on warfarin?
Yes, but only if you stay under 2,000 mg per day. Taking more than that for three or more days in a row can increase bleeding risk by affecting platelet function. Always check the total amount from all sources-cold medicines, pain relievers, and sleep aids often contain acetaminophen.
Is Sudafed safe with warfarin?
Yes, both pseudoephedrine (Sudafed) and phenylephrine (Sudafed PE) are considered safe at standard doses. They don’t interfere with warfarin’s blood-thinning effect. But avoid multi-symptom products that combine them with NSAIDs or high-dose acetaminophen.
What cold medicine is safest for someone on warfarin?
The safest approach is to pick single-ingredient products: guaifenesin for mucus, cetirizine or loratadine for runny nose, and pseudoephedrine for congestion. Avoid anything labeled "multi-symptom," "cold & flu," or "maximum strength." Always read the active ingredients list.
Can I take ibuprofen if I’m on warfarin?
No. Ibuprofen (Advil, Motrin) and other NSAIDs like naproxen (Aleve) significantly increase your risk of serious bleeding, especially in the stomach. Studies show this combination raises bleeding risk by 4.5 times. Even occasional use is dangerous. Use acetaminophen instead, and only within the safe daily limit.
Do OTC cold meds affect INR levels?
Yes. NSAIDs, high-dose acetaminophen, cimetidine, quinidine, and certain supplements can all raise or lower your INR. A rise in INR means your blood takes longer to clot-increasing bleeding risk. A drop means clots form more easily. Always monitor your INR closely after starting any new OTC product, even if it’s "safe."
Why do some cold meds say "not for people on blood thinners"?
Because they contain NSAIDs like ibuprofen or naproxen, which thin the blood on their own and also damage the stomach lining. When combined with warfarin, the risk of internal bleeding skyrockets. The FDA now requires this warning on the front of the package. If you see it, don’t ignore it.
Should I get genetic testing for warfarin sensitivity?
It’s not required, but it can help. If you have certain gene variants (CYP2C9 or VKORC1), your body processes warfarin differently. That means you might be more sensitive to OTC interactions. Testing isn’t widely available yet-only 18% of patients get it-but if you’ve had unexplained INR swings, talk to your doctor about it.
What to Do Next
If you’re on warfarin and haven’t talked to your anticoagulation clinic about OTC meds, do it today. Bring your medicine cabinet with you-or at least a list of everything you’ve taken in the last month. Ask for a Medication Safety Card. Set a reminder to check your INR after any cold or flu episode.Don’t wait for a bleeding event to learn the hard way. Thousands have already. You don’t have to be one of them.

Philip Rindom
November 16, 2025 AT 12:22Man, I just grabbed a bottle of Theraflu last week thinking it was fine since it said 'acetaminophen and phenylephrine' - didn't even look at the fine print. Now I'm paranoid every time I walk past the cold aisle. Thanks for the wake-up call.
Jess Redfearn
November 17, 2025 AT 04:46so like… can i just take tylenol? like a little bit? i dont wanna die but my head hurts
Scott Walker
November 18, 2025 AT 05:05Just scanned my last cold med with Warfarin Watch and it flagged the ibuprofen hidden in the 'Nighttime Cold Relief' bottle. 😳 I had no idea. This app is now on my home screen. 🙏
Sharon Campbell
November 19, 2025 AT 13:07why do we even have otc meds if we cant trust em? like wtf is the point of any of this. just stay home and cry i guess.
Brendan Peterson
November 20, 2025 AT 23:09The 2,000 mg acetaminophen limit is widely misunderstood. Studies show even 3,000 mg/day for 5+ days can elevate INR in sensitive patients. The real danger is cumulative exposure across multiple products - which is why pharmacists need to be actively consulted, not just asked in passing.
sara styles
November 21, 2025 AT 05:58Let’s be real - this whole system is rigged. The FDA only started requiring those warning labels after 17 lawsuits in 2022. Big Pharma knew for decades that warfarin + NSAIDs = death trap, but they kept pushing multi-symptom combos because they sell better. And now they want us to trust a barcode scanner app like it’s some kind of miracle? Wake up. The system doesn’t care if you bleed out - as long as you keep buying meds.
They even let St. John’s Wort sit on shelves like it’s harmless. It’s not. It’s a blood thinner disguised as a ‘natural mood booster.’ And guess who pays the price? The people too poor to get genetic testing. The ones who can’t afford a 90-minute workshop. The ones who just want to feel better without becoming a statistic.
They want you to think this is about ‘reading labels.’ No. It’s about corporate greed, underfunded healthcare, and a population too exhausted to read fine print after working two jobs. I’ve seen three people bleed internally because they took ‘just one’ of those pills. None of them knew. And now they’re gone.
So yes, scan the barcode. Get the card. Call your pharmacist. But don’t fool yourself - none of that changes the fact that we’re being sold poison wrapped in rainbow labels. And they’re still making money off your fear.
Segun Kareem
November 22, 2025 AT 06:12There’s a deeper truth here: medicine isn’t just about chemistry - it’s about culture. We’ve been taught to self-medicate like it’s a right, not a risk. We swipe, we buy, we pop - no thought, no consultation. But warfarin doesn’t care about your hustle. It doesn’t care that you’re tired, sick, or in a hurry. It just reacts. And if you don’t respect that, it will break you.
This isn’t about being careful. It’s about humility. It’s about admitting you don’t know everything - even when it’s just a cold. The real cure isn’t in the bottle. It’s in the conversation. With your pharmacist. Your doctor. Your family. The people who love you enough to say, ‘Wait - let me check that first.’
Next time you reach for something OTC, pause. Breathe. Ask yourself: ‘Is this helping me… or just letting me pretend I’m in control?’ Because sometimes, the bravest thing you can do is not take anything at all - until you’re sure.
Ashley B
November 23, 2025 AT 20:12Oh please. You think this is about cold meds? Wake up. The real danger is the government letting Big Pharma push these combos while quietly funding studies that downplay the risks. I’ve got friends on warfarin who’ve been told by their ‘clinic’ to ‘just avoid Advil’ - but no one told them about the sneaky magnesium salicylate in Doan’s Pills. That’s not negligence - it’s cover-up. And don’t even get me started on how they ignore genetic testing because it’s ‘too expensive.’ They don’t want you to know you’re genetically doomed. They want you to keep buying.
Rodney Keats
November 23, 2025 AT 22:20Wow. So the solution to a cold is… call your clinic, download an app, get a card, scan barcodes, and log everything? Sounds like a full-time job. Meanwhile, my doctor won’t even return my texts. Thanks for making me feel like a burden just for wanting to feel better.
Laura-Jade Vaughan
November 25, 2025 AT 19:54As someone who’s been on warfarin for 12 years and has a PhD in pharmacology, I must say: this post is *adorable*. 🌸 You’ve summarized the basics beautifully - but you completely omitted the role of gut microbiota in warfarin metabolism. Recent studies (2023, JAMA Cardiology) show that antibiotics or probiotics can alter INR by up to 2.1 points. And no, your ‘Medication Safety Card’ won’t mention that. 😘
Also, did you know that vitamin K-rich greens (kale, spinach) can destabilize INR? But you didn’t even mention diet. How… quaint.
Still, kudos for not saying ‘just avoid NSAIDs’ - that’s a 2010 mindset. 🥂
Jennifer Stephenson
November 27, 2025 AT 13:58Read labels. Ask your pharmacist. Avoid NSAIDs and high-dose acetaminophen. Use single-ingredient products. That’s it.