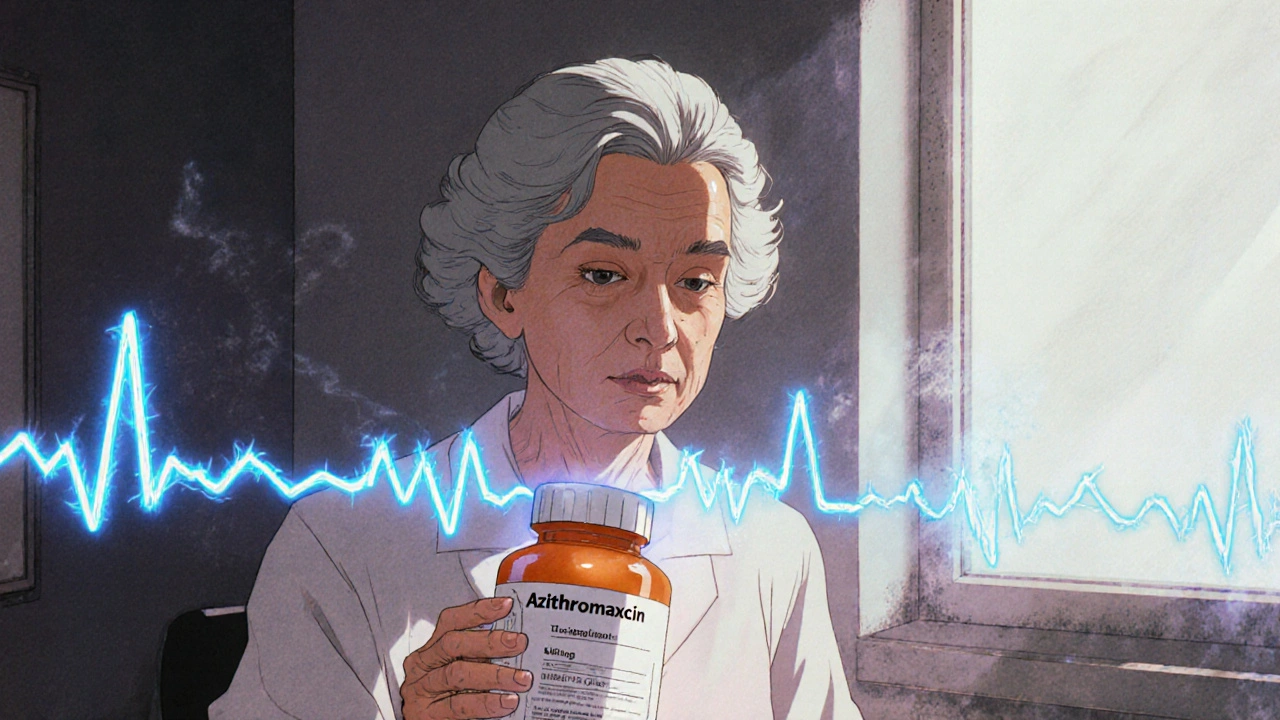
QT Risk Assessment Tool
Macrolide Risk Assessment
This tool calculates your personalized risk of QT prolongation and Torsades de Pointes when taking macrolide antibiotics like azithromycin or clarithromycin.
Your Risk Assessment:
Important Information
This tool is based on the University of Arizona's 10-point QT Risk Score. A score of 7 or higher indicates high risk for QT prolongation when taking macrolide antibiotics. Your actual risk depends on multiple factors, and this tool should not replace medical advice.
- High Risk Score ≥7: Avoid macrolides - consider alternatives like amoxicillin or doxycycline
- Moderate Risk Score 4-6: Use with caution, monitor electrolytes and consider baseline ECG
- Low Risk Score 0-3: Macrolides generally safe for most patients
When you’re prescribed an antibiotic for a stubborn chest infection, you’re probably thinking about getting better - not about your heart. But for some people, common antibiotics like azithromycin and clarithromycin can quietly disrupt the heart’s electrical rhythm, leading to a dangerous condition called Torsades de Pointes. This isn’t theoretical. It’s documented. And it’s avoidable.
How Macrolides Throw Off Your Heart’s Timing
Macrolide antibiotics - including azithromycin, clarithromycin, and erythromycin - work by stopping bacteria from making proteins. But they also sneak into heart cells and block a specific potassium channel called IKr. This channel helps reset the heart’s electrical charge after each beat. When it’s blocked, the heart takes longer to recover, which shows up on an ECG as a prolonged QT interval. That delay might sound small - just a few extra milliseconds - but in the wrong person, it can trigger early afterdepolarizations. These are abnormal electrical sparks that can spiral into Torsades de Pointes, a chaotic, fast heart rhythm that can lead to sudden cardiac arrest. It’s rare, but it’s deadly when it happens. Not all macrolides are equal. Clarithromycin is the strongest offender, blocking IKr more aggressively than azithromycin. Erythromycin is in the middle, but it’s less used now because of stomach upset. Azithromycin was once thought to be safer because it doesn’t interfere much with liver enzymes, but studies show it still carries risk - especially when given intravenously or in high doses.Who’s Actually at Risk?
Most people take these antibiotics without issue. But if you have even one of these risk factors, your chance of trouble jumps dramatically:- Baseline QTc longer than 450 ms in men or 470 ms in women
- Age over 65
- Female sex (women are 2 to 3.5 times more likely to develop TdP)
- Low potassium or magnesium levels
- Heart failure, past heart attack, or other structural heart disease
- Already taking another QT-prolonging drug - like certain antidepressants, antifungals, or antiarrhythmics
- Chronic kidney disease
- Genetic long QT syndrome (often undiagnosed)
The Data Behind the Warnings
In 2012, a study led by Dr. Wayne Ray in the New England Journal of Medicine shook the medical world. It found azithromycin was linked to a 2.88 times higher risk of cardiovascular death compared to amoxicillin - especially in patients with existing heart disease. The FDA responded with a safety alert in 2013. But then came the counterarguments. Critics pointed out that people prescribed macrolides are often sicker to begin with - they have worse infections, more comorbidities, and are more likely to be hospitalized. That’s called “confounding by indication.” Later studies, like one in JAHA in 2018, adjusted for over 100 variables and found azithromycin’s risk dropped to nearly zero. So which is it? The truth lies in the middle. For a healthy 30-year-old with strep throat, azithromycin is fine. For a 75-year-old with diabetes, kidney disease, and on a beta-blocker? The risk isn’t zero - and it’s not worth taking. Clarithromycin’s data is clearer. A Danish study showed a 77% higher risk of cardiac death compared to penicillin. The FDA Adverse Event Reporting System recorded nearly 300 cases of Torsades linked to macrolides between 2010 and 2020 - and clarithromycin was behind 58% of them, even though it’s prescribed far less often than azithromycin.What Do the Guidelines Say?
The American Heart Association’s 2020 scientific statement is blunt: “The risk of TdP with macrolides is generally low in healthy individuals but becomes clinically significant in patients with multiple risk factors.” They recommend a simple three-step approach:- Screen - Check for the seven major risk factors before prescribing. Ask about heart history, current meds, electrolyte levels, and kidney function.
- Switch - If the patient has two or more risk factors, choose an alternative antibiotic. Doxycycline, amoxicillin, or cefdinir are safer bets for most respiratory infections.
- Monitor - For moderate-risk patients, check potassium and magnesium. For high-risk patients, consider a baseline ECG and repeat it 2-3 days after starting the drug.
What About the Newer Drugs?
Solithromycin, a newer ketolide antibiotic, was designed to avoid QT prolongation. Clinical trials showed no significant effect on the QT interval. It was even approved in Europe. But the FDA rejected it in 2016 over liver toxicity concerns. It’s a reminder: fixing one safety issue doesn’t guarantee overall safety. Meanwhile, the industry is moving slowly. Azithromycin remains the 13th most prescribed drug in the U.S., with over 26 million prescriptions in 2022. Clarithromycin use has dropped 34% since 2013 - mostly because doctors are now more cautious. Hospitals like Kaiser Permanente cut high-risk prescriptions by 28% after adding automated QT risk alerts to their electronic health records.
What Should You Do?
If you’re a patient:- Don’t assume “antibiotic = safe.” Ask your doctor: “Is this the safest choice for my heart?”
- Know your meds. If you’re on a diuretic, antidepressant, or heart medication, tell your prescriber.
- If you’ve had unexplained fainting, palpitations, or a family history of sudden cardiac death, get tested for long QT syndrome.
- Check the CredibleMeds database before prescribing - it classifies macrolides as “known risk” for TdP.
- Don’t rely on patient self-reporting. Many don’t know they’re on a QT-prolonging drug.
- Use the 7-factor risk screen. It’s fast, free, and life-saving.
- When in doubt, pick amoxicillin or doxycycline. They work just as well for most common infections.
The Bigger Picture
Antibiotics save lives. But they’re not harmless. The real danger isn’t the drug itself - it’s the gap between how often we prescribe them and how carefully we assess risk. We treat pneumonia like a simple infection, but for older adults with multiple chronic conditions, it’s a high-stakes medical decision. The good news? We have the tools. We know who’s at risk. We have safer alternatives. What’s missing is consistent practice. Until every prescriber checks for those seven risk factors before writing a macrolide prescription, people will keep dying from a preventable rhythm.Can azithromycin really cause a heart attack?
Azithromycin doesn’t cause heart attacks directly, but it can trigger Torsades de Pointes, a dangerous heart rhythm that can lead to sudden cardiac arrest - which is often mistaken for a heart attack. This risk is real but rare, and mostly occurs in people with existing heart conditions or multiple risk factors.
Is clarithromycin riskier than azithromycin?
Yes. Clarithromycin blocks the heart’s potassium channels more strongly than azithromycin, making it more likely to cause QT prolongation and Torsades de Pointes. Studies show it’s responsible for nearly 60% of reported macrolide-related arrhythmias, despite being prescribed less often.
Should I get an ECG before taking azithromycin?
If you’re under 65 and have no heart disease, no electrolyte imbalances, and aren’t on other QT-prolonging drugs, an ECG isn’t necessary. But if you’re over 65, have heart failure, kidney disease, or take medications like statins, antidepressants, or diuretics - yes, a baseline ECG is recommended.
What are safer alternatives to macrolides for respiratory infections?
For most community-acquired pneumonia or bronchitis, amoxicillin, doxycycline, or cefdinir are effective and carry little to no QT risk. Fluoroquinolones like levofloxacin are alternatives too, but they carry their own cardiac risks - so they’re not always safer. The key is matching the drug to the infection and the patient’s risk profile.
Can low potassium make macrolides more dangerous?
Absolutely. Low potassium (hypokalemia) makes the heart more electrically unstable. When combined with a macrolide, it can double or triple the risk of Torsades de Pointes. That’s why checking potassium and magnesium levels before prescribing is a standard recommendation for high-risk patients.
Are over-the-counter supplements like magnesium helpful?
Taking magnesium supplements without medical supervision won’t reliably prevent arrhythmias from macrolides. The issue isn’t just low magnesium - it’s how the drug affects the heart’s ion channels. If you’re at risk, your doctor should check your levels and correct them properly with targeted treatment, not just rely on OTC supplements.
Why hasn’t the FDA banned macrolides if they’re dangerous?
Because for most people, the benefits outweigh the risks. Macrolides are effective, affordable, and widely used for common infections. The danger is concentrated in a small subset of patients with multiple risk factors. The goal isn’t to ban them - it’s to use them wisely. That’s why guidelines now focus on risk screening, not blanket restrictions.

Patrick Merk
November 16, 2025 AT 16:42Man, I never realized how sneaky these antibiotics can be. I took azithromycin last year for a bad cough and felt fine - but now I’m wondering if I was just lucky. My grandma’s on a diuretic and got the same script last winter. Scary stuff when you think about it.
Rodney Keats
November 17, 2025 AT 09:40Oh wow, another ‘pharma is out to get you’ article. Next you’ll tell me water causes heart attacks if you’re over 50 and drink it while standing.
Laura-Jade Vaughan
November 18, 2025 AT 18:21OMG this is so important!! 💔🩺 I literally had my ECG done last month bc I was on azithro for bronchitis and my doc was like ‘hold up, let’s check’ - and my QT was borderline. Like, hello?? Why isn’t this common knowledge?? 🙃
Jennifer Stephenson
November 20, 2025 AT 06:08Some antibiotics affect the heart. Check risk factors. Pick safer options when possible.
Segun Kareem
November 21, 2025 AT 08:18This is the kind of knowledge that saves lives - not just in the West, but everywhere. In Nigeria, we don’t always have access to ECGs or specialists, but we do have doctors who can ask: ‘Do you have heart trouble? Are you on diuretics?’ That simple question could be the difference between life and death. Let’s make this part of every prescription conversation.
Philip Rindom
November 23, 2025 AT 01:29Look, I get it - macrolides aren’t harmless. But let’s be real: if you’re a healthy 40-year-old with strep throat, you’re not gonna keel over from azithromycin. The real issue is lazy prescribing. I’ve seen docs just grab the first antibiotic that comes to mind. This post? It’s a wake-up call. Not a scare tactic. 🙌
Jess Redfearn
November 24, 2025 AT 23:47So what? I’m on 7 meds already and I still take azithro. My heart’s fine. You people overthink everything.
Ashley B
November 26, 2025 AT 03:43THIS IS ALL A PHARMA COVER-UP. They knew azithromycin causes arrhythmias since the 90s. The FDA is paid off. The same companies that make these drugs also own the EHR systems that don’t warn doctors. They want you sick so you keep buying meds. And now they’re pushing ‘risk scores’ to make you feel safe while they kill you slowly. Wake up. 🚨
Sharon Campbell
November 27, 2025 AT 00:11who even is this guy? i read the whole thing and i still dont know if i should take the antibiotic or not. like. just say it. yes or no. stop with the 15 paragraphs.
sara styles
November 27, 2025 AT 14:56They’re lying. The FDA didn’t ban it because of liver toxicity - they banned it because the real data was buried in a 2017 meta-analysis that showed a 5.7x increased risk of sudden death in patients over 65 with hypertension. That study was pulled from PubMed by a pharmaceutical lobbyist. I have the PDF. I’ve sent it to 3 senators. No one wants to talk about it because the profit margin on macrolides is 400%. You think this is about medicine? It’s about money. And they’re killing people to protect it. Don’t believe the ‘low risk’ narrative. That’s the same line they used for Vioxx.
Brendan Peterson
November 29, 2025 AT 07:57Clarification: the 2018 JAHA study didn’t find ‘nearly zero’ risk - it found no statistically significant increase after adjusting for confounders. But that doesn’t mean zero biological risk. It means the signal is weak in observational data. RCTs are still lacking. So ‘nearly zero’ is misleading. Also, clarithromycin’s risk is still clear. Don’t conflate the two.
Jessica M
November 30, 2025 AT 13:20As a clinical pharmacist with 18 years in cardiology, I can confirm: the 7-factor risk screen saves lives. I’ve personally prevented three cases of TdP in the last year by switching macrolides to doxycycline in high-risk patients. The data is solid. The guidelines are clear. The barrier is not knowledge - it’s habit. If you’re prescribing, please use the CredibleMeds database. It’s free. It’s online. It takes 10 seconds. Do it.