Checkpoint inhibitors and CAR-T cell therapy aren’t just new cancer treatments-they’re rewriting the rules of how we fight the disease. For decades, chemotherapy and radiation were the go-to tools, attacking fast-growing cells without much regard for whether they were cancerous or healthy. But these two immunotherapies work differently. Instead of poisoning the body, they empower the body’s own immune system to find and destroy cancer cells. And for some patients, the results have been life-changing.
How Checkpoint Inhibitors Unleash the Immune System
Your immune system has built-in brakes. That’s a good thing. It stops your body from attacking itself. But cancer cells are sneaky. They learn how to flip those brakes on, tricking your T cells-the immune system’s frontline soldiers-into ignoring them. Checkpoint inhibitors are drugs designed to smash those brakes. The most common targets are PD-1, PD-L1, and CTLA-4. These are proteins that act like stop signs between T cells and cancer cells. Drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) block PD-1. Atezolizumab (Tecentriq) blocks PD-L1. Ipilimumab (Yervoy) blocks CTLA-4. When these drugs are given, the stop signs disappear. T cells wake up, recognize the cancer, and start attacking. These drugs work best in cancers that already have some immune activity-like melanoma, lung cancer, and kidney cancer. Response rates vary. In some patients, tumors shrink dramatically and stay gone for years. In others, nothing happens. Why? Because not all tumors are visible to the immune system. Some don’t have enough mutations to stand out. Others create a shield of suppressive cells around themselves. Side effects happen because once you remove the brakes, the immune system can turn on healthy tissues. That’s called an immune-related adverse event (irAE). Common ones include rash, colitis, thyroid problems, and lung inflammation. About 30-40% of patients get a rash. Up to 15% develop colitis. These are manageable with steroids, but they require careful monitoring.CAR-T Therapy: Engineering Your Own Cancer Fighters
CAR-T therapy is like giving your immune system a GPS and a weapon upgrade. It starts with a simple blood draw. Doctors collect your T cells. Then, in a lab, those cells are genetically modified to carry a synthetic receptor called a chimeric antigen receptor, or CAR. This receptor is designed to latch onto a specific protein on cancer cells-like CD19 on B-cell leukemias and lymphomas. After the cells are engineered, they’re multiplied in bioreactors until there are hundreds of millions. Then, after a round of chemotherapy to clear space in the body, they’re infused back into you. These supercharged T cells go hunting. They find cancer cells with the target protein, stick to them, and kill them. The results in certain blood cancers are stunning. In children with relapsed acute lymphoblastic leukemia, complete response rates hit 80-90%. For adults with aggressive lymphoma, about 40-50% see long-term remission. These aren’t just temporary improvements-many patients remain cancer-free for years. But CAR-T isn’t simple. The process takes 3 to 5 weeks. It’s expensive-between $373,000 and $475,000 per treatment. And the side effects can be severe. Cytokine release syndrome (CRS) happens in 50-70% of patients. Your immune system goes into overdrive, causing high fever, low blood pressure, and breathing trouble. Immune effector cell-associated neurotoxicity syndrome (ICANS) affects 20-40% of patients, leading to confusion, seizures, or trouble speaking. Both require ICU-level care.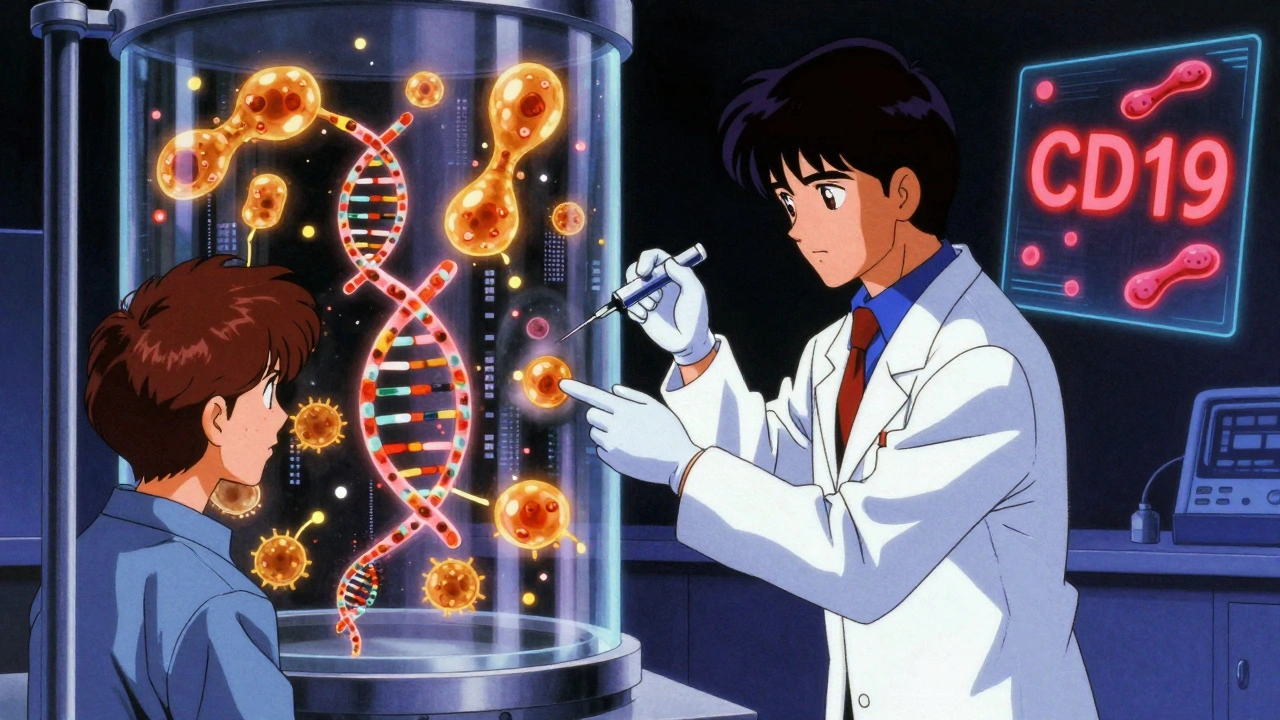
Why CAR-T Struggles with Solid Tumors
CAR-T therapy has revolutionized blood cancer treatment. But for lung, breast, or colon cancer? Progress has been slow. Why? Solid tumors are hostile environments. They’re surrounded by fibrous tissue that blocks T cells from getting in. They pump out chemicals that shut down immune activity. And they often don’t have a single, clear target protein like CD19. If the target exists on healthy cells too, CAR-T cells can attack them-leading to dangerous side effects. In trials for pancreatic or ovarian cancer, response rates have been under 10%. Even when CAR-T cells get inside, they often become exhausted-just like the natural T cells that checkpoint inhibitors try to revive. That’s why researchers are trying to engineer smarter CAR-T cells. Some are being built to secrete their own checkpoint-blocking antibodies right at the tumor site. This avoids the full-body toxicity of drugs like Keytruda. In mouse studies, this approach cut immune lung damage by 42% while keeping tumor-killing power strong. Others are being armored with cytokines like IL-12 to help them survive longer inside the tumor. New targets are being explored-like B7-H3 and GPC3-that show promise in early trials.Combining the Two: The Next Frontier
The real breakthrough might not be choosing between checkpoint inhibitors and CAR-T-it’s using them together. Think of it this way: CAR-T cells bring the soldiers to the battlefield. But if the battlefield is filled with poison gas (the tumor’s immunosuppressive environment), those soldiers won’t last long. Checkpoint inhibitors remove the gas. Clinical trials are now testing this combo in melanoma, lung cancer, and even glioblastoma. As of March 2024, there were 47 active trials combining the two, and 68% of them focus on solid tumors. One clever approach from 2018 involved engineering CAR-T cells to produce their own PD-1-blocking fragment. This meant the drug was delivered exactly where it was needed-inside the tumor-reducing side effects by 37% in animal models. It’s like having a soldier carry their own antidote. But it’s not perfect. Even together, these therapies struggle to overcome the toughest tumors. Researchers are now looking at blocking other checkpoints like LAG-3 and TIM-3, or targeting intracellular brakes like PTP1B. Early studies show blocking PTP1B alongside CAR-T can triple the number of T cells that infiltrate breast tumors in mice.
Access and Equity: Who Gets These Treatments?
These therapies are miracles-but they’re not equally available. Checkpoint inhibitors are available in most hospitals. They’re shipped like regular drugs. CAR-T therapy? It’s a bespoke, one-patient-at-a-time manufacturing process. Only specialized centers can handle it. In the U.S., 87% of CAR-T treatments are given at academic medical centers, even though those make up only 15% of cancer clinics. Access disparities are stark. A 2020 review found Medicaid patients were 23% less likely to get CAR-T than those with private insurance. Black patients were 31% less likely to receive it than white patients. Cost isn’t the only barrier. It’s logistics, referrals, awareness, and systemic gaps in care. The European Medicines Agency approved its first CAR-T therapy in August 2018-10 months after the FDA. That delay isn’t just bureaucratic. It affects lives.What’s Next?
The future of immunotherapy is moving fast. “Off-the-shelf” CAR-T cells-made from healthy donors instead of the patient-are in trials. These could cut wait times from weeks to days and lower costs. Companies are also testing CAR-T for earlier stages of cancer, not just when everything else has failed. New targets are being discovered. Better ways to deliver the therapy are being built. And researchers are learning how to predict who will respond-before treatment even starts. But the biggest shift isn’t technological. It’s philosophical. We’re no longer just trying to kill cancer cells. We’re trying to retrain the immune system to see them as enemies-and keep fighting, long after the last dose. These therapies aren’t cures for everyone. But for the people who respond, they offer something rare: time. Time with family. Time without chemo. Time to hope again.How do checkpoint inhibitors differ from CAR-T cell therapy?
Checkpoint inhibitors are drugs-usually intravenous antibodies-that block signals cancer cells use to hide from the immune system. They work systemically, meaning they circulate throughout the body. CAR-T therapy is a personalized treatment: your own T cells are removed, genetically altered in a lab to target cancer, multiplied, and infused back into you. It’s a living drug, designed to hunt specific cancer cells.
Which cancers respond best to checkpoint inhibitors?
Melanoma, non-small cell lung cancer, kidney cancer, and Hodgkin lymphoma respond best. These cancers often have high mutation loads, making them more visible to the immune system. Response rates range from 20% to 40%, and some patients experience long-lasting remissions.
Why is CAR-T therapy so expensive?
Each CAR-T treatment is custom-made for one patient. The process involves collecting blood, shipping it to a specialized lab, genetically modifying the cells, growing them over 3-5 weeks, and then reinfusing them. This personalized manufacturing, along with the need for intensive care during side effects, drives costs to $373,000-$475,000 per treatment.
Can CAR-T therapy treat solid tumors like breast or lung cancer?
So far, success has been limited. Solid tumors create physical and chemical barriers that block T cells from entering. They also lack clear, unique targets. Early trials show response rates below 10%. But new engineered CAR-T cells-like those that secrete checkpoint blockers or carry cytokines-are showing promise in ongoing clinical trials.
What are the biggest side effects of CAR-T therapy?
The two most serious are cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). CRS causes high fever, low blood pressure, and breathing issues. ICANS can lead to confusion, seizures, or trouble speaking. Both require immediate medical care. About 50-70% of patients experience CRS, and 20-40% get ICANS.
Are there alternatives to using a patient’s own cells for CAR-T therapy?
Yes. Researchers are developing "off-the-shelf" CAR-T cells from healthy donors. These are made in bulk and stored for immediate use, cutting the wait time from weeks to days. Early trials show promise, but challenges remain-like the body rejecting the donor cells or the therapy not lasting as long. Still, this could make CAR-T more accessible and affordable.
How do doctors decide between checkpoint inhibitors and CAR-T therapy?
It depends on the cancer type, stage, and patient health. CAR-T is mostly used for certain blood cancers after other treatments fail. Checkpoint inhibitors are used earlier, often as first-line treatment for melanoma, lung, or kidney cancer. Biomarker tests-like PD-L1 levels or tumor mutation burden-help guide the choice. For some patients, combining both may be the best option.


Vivian Amadi
December 10, 2025 AT 21:49Katherine Liu-Bevan
December 12, 2025 AT 11:28matthew dendle
December 13, 2025 AT 02:47Kristi Pope
December 14, 2025 AT 03:18we need to celebrate them too
Jim Irish
December 15, 2025 AT 09:13Jimmy Kärnfeldt
December 16, 2025 AT 02:12even if it doesn't work for everyone, the fact that it works for some at all? that's hope made tangible
Mia Kingsley
December 17, 2025 AT 23:27Sylvia Frenzel
December 18, 2025 AT 21:45Lisa Stringfellow
December 19, 2025 AT 22:32Paul Dixon
December 20, 2025 AT 07:52Eddie Bennett
December 20, 2025 AT 12:59Ariel Nichole
December 22, 2025 AT 00:52Vivian Amadi
December 23, 2025 AT 08:39