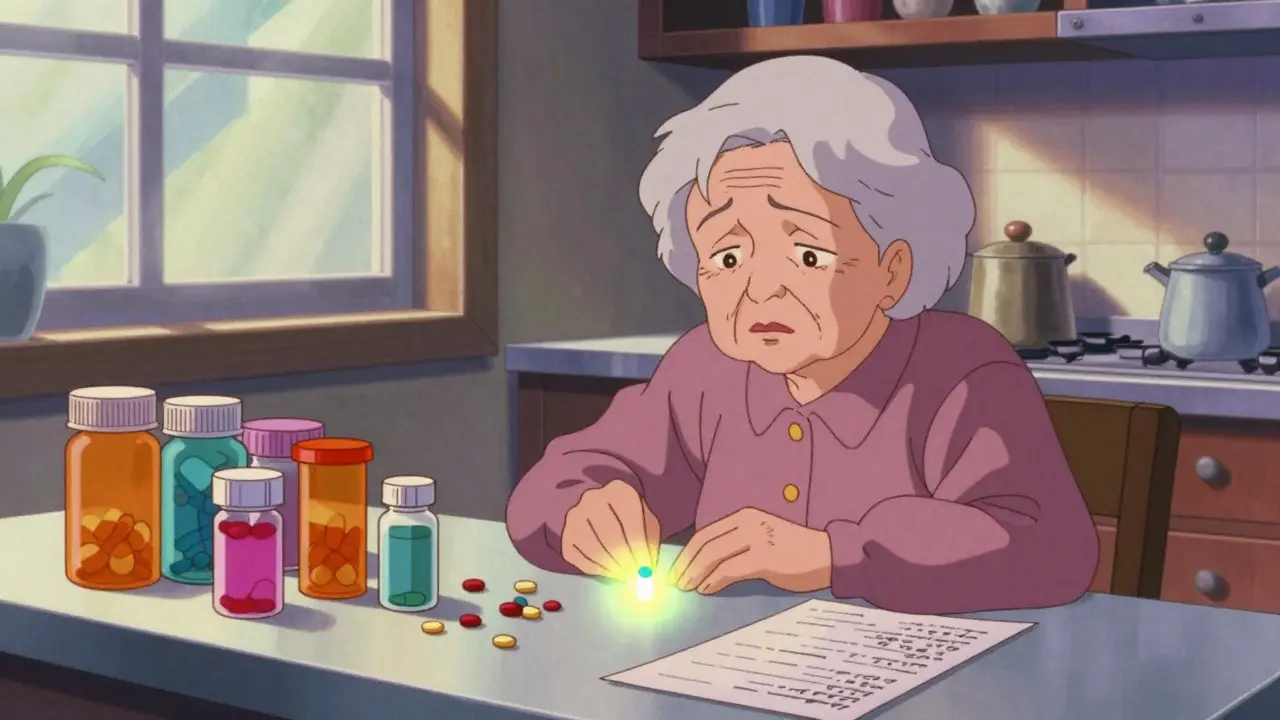
Imagine waking up every morning and counting out 10 pills. Some you take with breakfast, others at lunch, a few before bed. You forget which is which. You skip one because it makes your stomach upset. Or you double up because you’re not sure if you took it already. This isn’t rare-it’s the daily reality for many seniors managing multiple chronic conditions. The pile of pills on the kitchen counter? That’s pill burden. And it’s not just inconvenient-it’s dangerous.
Why Pill Burden Matters More Than You Think
Pill burden isn’t just about how many pills you swallow. It’s about how many chances you have to get it wrong. For seniors, especially those with memory issues, arthritis, or vision problems, each extra pill increases the risk of missed doses, overdoses, or dangerous drug interactions. Studies show that when people take five or more medications daily, their chance of hospitalization jumps by 40%. And the biggest reason? Not side effects-it’s simply forgetting or getting confused. The good news? You don’t have to live with this chaos. Fixed-dose combination (FDC) medications, also called single-pill combinations, are designed to cut that pile in half-or even more. These are pills that combine two or more drugs into one tablet. For example, instead of taking a blood pressure pill and a water pill separately, you take one pill that does both. That’s not science fiction. It’s standard care for millions.How Combination Medications Work
Combination pills aren’t just two tablets squished together. They’re carefully engineered to make sure each drug works the way it should. The active ingredients are balanced so they’re absorbed properly, don’t interfere with each other, and stay stable over time. This isn’t easy. It takes years of testing. The FDA requires proof that the combo works just as well-or better-than taking the drugs separately. You’ll find these combinations most often for:- Hypertension: ACE inhibitors + diuretics, or calcium channel blockers + ARBs
- Diabetes: Metformin + SGLT2 inhibitors or DPP-4 inhibitors
- Heart disease: Statins + blood pressure meds
- HIV: Multiple antivirals in one tablet
The Evidence: Why This Actually Works
Numbers don’t lie. A 2007 meta-analysis in the American Journal of Medicine found that patients taking combination pills were 26% more likely to stick to their regimen than those taking the same drugs separately. That’s not a small gain-it’s life-changing. In a study published in the European Journal of Cardiology Practice, patients on single-pill combinations had lower blood pressure after just 12 weeks. Their systolic pressure dropped by nearly 4 mmHg more than those on separate pills. That might sound tiny, but in real-world terms, it means fewer heart attacks, fewer strokes, fewer ER visits. And it’s not just about health. It’s about cost. When people take their meds correctly, they spend less on hospital care. A 2023 analysis in the Journal of Health Economics and Outcomes Research showed that combination pills saved money across the board-on prescriptions, co-pays, and even caregiver time. One woman in Bristol told her pharmacist she saved £28 a month just by switching from four separate pills to two combos. She didn’t have to make two trips to the pharmacy anymore.
When Combination Pills Don’t Work
This isn’t a magic fix. Combination pills have limits. You can’t adjust the dose of one drug without changing the whole pill. That’s a problem if you’re still figuring out the right strength. For example, if your blood pressure drops too low on a combo with 10 mg of one drug and 160 mg of another, you can’t just cut the dose of one. You have to switch to a different combo-or go back to separate pills. Some seniors also have allergies or side effects to one component. Say you’re on a combo with hydrochlorothiazide and you develop a rash. You can’t just stop that one drug-you have to stop the whole pill and find another option. That’s why doctors don’t jump straight to combos for everyone. They start with single drugs, fine-tune the dose, then switch to a combo once things are stable. Also, not all combos are available in every strength. If you need 5 mg of one drug and 25 mg of another, but the only combo comes in 10 mg and 50 mg, you’re stuck. That’s why it’s important to talk to your pharmacist. They know what’s available and can help you find the closest match.How to Talk to Your Doctor About Switching
Don’t wait for your doctor to bring it up. Ask. Say: “I’m having trouble keeping track of all my pills. Is there a combination medicine that could simplify this?” Bring your pill bottle list to the appointment. Write down which pills you forget, which make you feel sick, and which you skip. Your doctor can use that to decide if a combo makes sense. Ask these questions:- Can any of my meds be combined into one pill?
- Are there generic versions of these combos? They’re often much cheaper.
- What happens if I need to change one dose later?
- Is there a version with a lower dose if I’m sensitive to side effects?
What Pharmacists Can Do for You
Your pharmacist is your secret weapon. They see your full prescription history. They know which combos are covered by your insurance. They can flag interactions you didn’t know about. Ask your pharmacist for a medication review. Many pharmacies offer this for free. They’ll go through every pill, check for duplicates, spot unnecessary drugs, and suggest combos. Some even give you a printed chart showing which pills to take when. One Bristol pharmacy started a “Pill Burden Clinic” last year. Patients who went saw their pill count drop by an average of 40% in six weeks. They can also help with:- Switching to blister packs or pill organizers
- Setting up refill reminders
- Connecting you with programs that help pay for meds
What’s Coming Next
The future of combination meds is getting smarter. Researchers are testing “polypills” with three or four drugs for heart disease risk reduction. Some include aspirin, a statin, and two blood pressure pills-all in one tablet. Early trials show patients on these polypills are 30% more likely to stick to their treatment. There’s also work on extended-release combos that last 24 hours with just one dose. And new tech is making it easier to track adherence. Some pills now have tiny sensors that send a signal to your phone when you swallow them. It sounds high-tech, but it’s already being used in clinical settings. The goal isn’t just fewer pills. It’s fewer hospital beds, fewer falls, fewer missed birthdays. It’s about giving seniors back control over their own health.Real Talk: What You Can Do Today
You don’t need to wait for a breakthrough. Start now:- Write down every medication you take, including vitamins and supplements.
- Count how many pills you take each day. Be honest.
- Ask your doctor: “Can any of these be combined?”
- Ask your pharmacist: “Are there cheaper or simpler versions?”
- If you’re on a combo, don’t stop it unless your doctor says so-even if you feel fine.
Are combination medications safe for seniors?
Yes, when prescribed correctly. Combination medications are rigorously tested for safety and effectiveness in older adults. The key is matching the combo to your specific health needs. Your doctor will check for kidney function, liver health, and other factors before prescribing. Many seniors benefit from lower doses in combos because they reduce side effects like dizziness or dehydration that can happen with higher doses of single drugs.
Can I switch from separate pills to a combination pill on my own?
No. Never switch medications without talking to your doctor. Even if the ingredients are the same, the dosage or timing might be different. Stopping or changing pills suddenly can cause dangerous spikes in blood pressure, blood sugar, or heart rate. Always get professional advice before making any changes.
Are combination pills more expensive than buying separate medications?
Usually, they’re cheaper. Generic combination pills often cost less than buying each drug separately, especially when you factor in co-pays and pharmacy fees. Some insurance plans cover combos at a lower tier than multiple individual prescriptions. Ask your pharmacist to compare the total monthly cost of your current regimen versus a combo option.
What if I need to adjust the dose of one drug in the combo?
If your condition changes and you need a different dose, your doctor may switch you to a different combination pill or temporarily go back to separate medications. Some combos come in multiple strengths-for example, 5 mg/100 mg or 10 mg/200 mg. If no suitable combo exists, your doctor will find the next best option. Flexibility is built into the process.
Do combination pills work for all chronic conditions?
Not yet-but they’re expanding fast. They’re most common for hypertension, diabetes, HIV, and heart disease. Research is ongoing for combos in conditions like COPD, depression, and Parkinson’s. If you’re on multiple meds for a chronic illness, ask if a combo exists or is in development. Even if one isn’t available now, it might be soon.

Hayley Ash
December 30, 2025 AT 12:30kelly tracy
January 1, 2026 AT 02:34Shae Chapman
January 2, 2026 AT 13:22henry mateo
January 2, 2026 AT 20:21Aayush Khandelwal
January 4, 2026 AT 06:15Nadia Spira
January 5, 2026 AT 18:18Kunal Karakoti
January 7, 2026 AT 14:31Glendon Cone
January 7, 2026 AT 16:38Kelly Gerrard
January 7, 2026 AT 23:14srishti Jain
January 9, 2026 AT 17:47Sandeep Mishra
January 11, 2026 AT 02:06Colin L
January 12, 2026 AT 09:50Henry Ward
January 13, 2026 AT 00:27Joseph Corry
January 14, 2026 AT 03:27Cheyenne Sims
January 15, 2026 AT 08:23