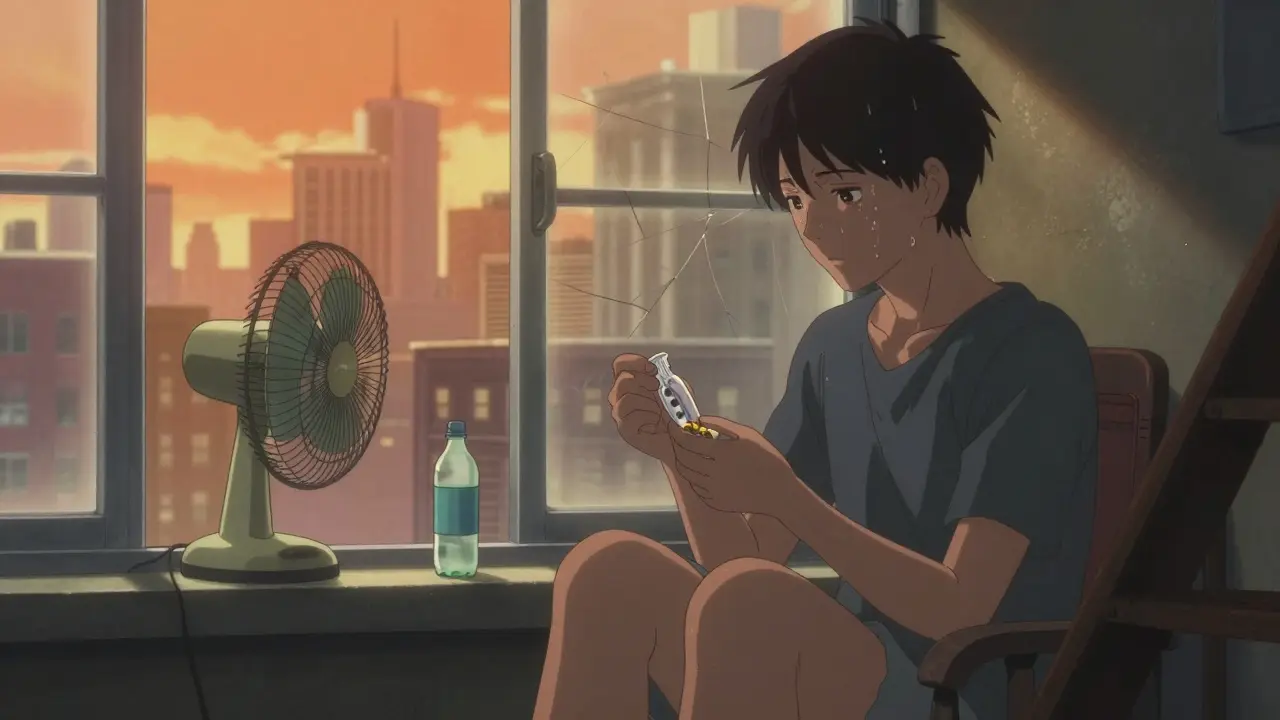
When the temperature climbs above 24°C (75.2°F), the risk of overdose doesn’t just stay the same-it goes up. Not because people use more drugs, but because heat changes how the body handles them. For someone using opioids, stimulants, or even prescription medications, a heatwave isn’t just uncomfortable-it’s deadly. And it’s not just about being outside. Indoor spaces without air conditioning, shelters that turn people away, or even a cramped apartment with no fan can become death traps during extreme heat.
Why Heat Makes Overdose More Likely
Your body works hard to stay cool. When it’s hot, your heart pumps faster, your blood vessels widen, and you sweat. But if you’re using drugs like cocaine, methamphetamine, or even opioids, your body is already under strain. Cocaine raises your heart rate by 30-50%. Heat adds another 10-25 beats per minute. Together, that’s a dangerous combo. Your heart can’t keep up. That’s when cardiac arrest happens. Dehydration makes it worse. Lose just 2% of your body weight in fluids-something easy to do in the heat-and drugs become more concentrated in your bloodstream. That means a dose you normally take might now be too strong. It’s like pouring the same amount of alcohol into half the water. You get drunk faster. Same with drugs. Opioids already slow your breathing. Heat makes that worse. Studies show heat reduces your body’s ability to compensate for respiratory depression by 12-18%. That tiny margin between safety and stopping breathing? Gone. And if you’re taking medications for mental health-antidepressants, antipsychotics-heat can make them less effective or more toxic. About 70% of antipsychotics and 45% of antidepressants behave differently in high temperatures, according to research in JAMA Internal Medicine. That’s not just a side effect. It’s a risk multiplier.Who’s Most at Risk
People experiencing homelessness are especially vulnerable. In the U.S., about 580,000 people are homeless on any given night. Nearly 4 in 10 of them have a substance use disorder. They don’t have access to cool spaces. They can’t refill water bottles easily. They’re often turned away from shelters if they’re actively using drugs. Even people who aren’t homeless but live in older buildings without AC are at risk. Cities are hotter than surrounding areas-up to 5°C warmer because of concrete, asphalt, and lack of trees. That’s the urban heat island effect. In places like Philadelphia or Seattle, where summers used to be mild, the spike in overdose deaths during heat domes has been shocking. The CDC found that regions with historically cooler climates-like the Pacific Northwest-see overdose risk spike 3.7 times higher during heat events than in places like Arizona, where people are more used to the heat. Why? Lack of acclimatization. Your body needs time to adjust. When heat hits fast, your systems don’t have a chance.What You Can Do: Practical Harm Reduction Steps
You don’t need to stop using drugs to stay alive in the heat. But you do need to change how you use them.- Reduce your dose by 25-30% when it’s above 24°C. This isn’t guesswork. It’s based on how your body metabolizes drugs in heat. Less is safer.
- Use less frequently. Give your body time to recover. Space out use by at least 24-48 hours during heatwaves.
- Hydrate constantly. Drink one cup (8 oz) of cool water every 20 minutes-even if you don’t feel thirsty. Electrolyte packets help too. Many harm reduction groups now hand out free hydration packs with water, salt, and sugar.
- Never use alone. If you’re alone and something goes wrong, no one calls for help. Use in a group. If that’s not possible, tell someone where you are and when you’ll check in.
- Keep naloxone handy. Naloxone works for opioid overdoses. It’s free in many places. Carry it. Know how to use it. Teach your friends.
- Avoid mixing drugs. Alcohol, benzodiazepines, and stimulants all interact unpredictably with heat. The more you mix, the less your body can cope.

What Services Are Available
Some cities have figured this out. Vancouver set up seven air-conditioned respite centers next to supervised consumption sites during the 2021 heat dome. They offered water, showers, medical checks, and naloxone training. Overdose deaths dropped by 34% that summer. Philadelphia started handing out cooling kits-misting towels, electrolyte sachets, hats, and info sheets-after their 1995 heatwave killed 700 people. In 1999, after they implemented their plan, deaths dropped to 100. They’ve kept it going. Now they give out over 2,500 kits every summer. In Maricopa County, Arizona, volunteers trained in naloxone use do daily wellness checks on people who use drugs. In 2022, they made over 12,000 visits. They found 287 overdoses and reversed them all. But here’s the problem: only 12 out of 50 U.S. states have official heat emergency plans that include people who use drugs. Most don’t. That means you can’t rely on the system. You have to plan for yourself.What to Avoid
- Don’t wait until you feel sick. Heat exhaustion hits fast. Symptoms: dizziness, nausea, confusion, rapid pulse. If you have them, get cool immediately. Don’t wait to see if it gets better.
- Don’t use in direct sun or hot rooms. Even a car parked in the sun can hit 60°C inside. That’s not a place to rest.
- Don’t assume shelters will help. Many still turn away people who are actively using. Know your local options ahead of time. Call ahead. Ask: “Do you allow people who use drugs during heat advisories?”
- Don’t ignore medication side effects. If you’re on antidepressants or antipsychotics, talk to your provider about heat. Your dose might need adjusting.

How to Help Others
If you care about someone who uses drugs, you can make a difference.- Carry extra water and electrolytes. Offer them.
- Know where the nearest cooling center is. Share the info.
- Learn how to use naloxone. It’s simple. Takes 2 minutes.
- Don’t judge. If someone is using drugs in the heat, they’re not being reckless-they’re surviving. Your support could save their life.
- If you’re part of a community group, push your local health department to include substance use in their heat emergency plan. The Biden administration has allocated $50 million for this exact purpose. Demand it be used.
The Bigger Picture
This isn’t just about individual choices. It’s about systems failing people. Climate change is making heatwaves longer, stronger, and more frequent. By 2050, we could see 20-30 extra days each year above the 24°C overdose risk threshold. New research suggests heat might even change your gut bacteria-which affects how drugs are broken down. We’re only starting to understand the full picture. But right now, we know enough to act. Hydration. Lower doses. Naloxone. Cooling spaces. These aren’t luxury ideas. They’re life-saving tools. The CDC says people who use drugs make up 18-22% of heat-related emergency visits. That’s not a small number. That’s a crisis. And it’s one we can fix-if we choose to.Can heat make a drug overdose worse even if I don’t feel hot?
Yes. Your body’s internal temperature can rise even if you’re indoors or in the shade. Heat affects your metabolism, heart rate, and hydration levels-all of which change how drugs act in your system. You don’t need to feel sweaty or dizzy for an overdose to happen. The risk increases as soon as temperatures go above 24°C (75.2°F), regardless of how you feel.
Is it safe to use drugs in air-conditioned places during a heatwave?
Air conditioning reduces the physical risk from heat, but it doesn’t eliminate overdose risk. Dehydration, drug potency, and mixing substances still matter. Even in a cool room, using alone or skipping hydration can lead to overdose. The safest approach is to reduce your dose, stay hydrated, and never use alone-even in AC.
Does naloxone work for overdoses caused by heat and drugs?
Naloxone only reverses opioid overdoses. If heat causes an overdose from cocaine, meth, or alcohol, naloxone won’t help. But if opioids are involved-even mixed with other drugs-naloxone can still save a life. Always carry it if opioids are part of your use. It’s free in many places and easy to use.
Why do some shelters turn away people who use drugs during heatwaves?
Many shelters have policies against active drug use due to liability concerns, staff training gaps, or lack of resources. Some fear violence, theft, or medical emergencies they’re not equipped to handle. This leaves people with nowhere to go during extreme heat. Advocacy groups are pushing for policy changes, but until then, it’s critical to know which shelters are safe and which aren’t-call ahead before showing up.
Can I get help for hydration and cooling supplies without being judged?
Yes. Many harm reduction organizations give out water, electrolytes, cooling towels, and hats without asking questions. In cities like New York, Philadelphia, and Vancouver, these services are offered through mobile outreach teams, community centers, and supervised consumption sites. You don’t need to be in recovery or clean to get help. These services exist because they save lives.
What should I do if I see someone collapsing from heat and possible overdose?
Call emergency services immediately. Move the person to a cooler place if possible. If they’re unresponsive and you suspect opioid overdose, give naloxone if you have it. Cool them down with wet cloths, fans, or ice packs on the neck, armpits, and groin. Don’t wait. Even if you’re unsure, acting fast can make the difference between life and death.

Meghan O'Shaughnessy
December 17, 2025 AT 08:00Been using in my apartment without AC for weeks now. Didn’t realize how much the heat was stacking the deck against me. Just cut my dose by 30% this week and felt like a whole new person. No more dizzy spells after using. Simple fix, massive difference.
Also started carrying those free electrolyte packs from the harm reduction van. They’re like magic in a pouch. Water + salt + sugar. No judgment. Just life-saving stuff.
People act like you have to be clean to deserve cool air. But the truth? You deserve to survive even if you’re not okay yet.
Kaylee Esdale
December 17, 2025 AT 19:24heat kills quietly. no sirens. no headlines. just a body cooling off in a room with no fan and a spoon still warm.
you don’t need to be a saint to deserve water. you just need to be breathing.
Jody Patrick
December 18, 2025 AT 02:04Stop coddling addicts. If you can’t handle the heat, don’t use. Simple. No handouts. No special treatment. Personal responsibility.
Radhika M
December 19, 2025 AT 11:31From India, we know heat. We sweat, we drink nimbu pani, we rest in shade. Same rules apply here. Drink water. Don’t use alone. Lower dose. No magic. Just basics.
And naloxone? Free in Delhi too. Why not here? Simple things save lives.
Philippa Skiadopoulou
December 20, 2025 AT 13:21The data presented is compelling and aligns with clinical observations in urban health settings. The physiological mechanisms linking hyperthermia to pharmacokinetic alterations are well documented in toxicology literature.
That said, the absence of coordinated public health infrastructure remains a critical gap. Municipalities must integrate substance use populations into heat response protocols as a matter of public safety, not moral preference.
Pawan Chaudhary
December 21, 2025 AT 12:19Hey, I’ve been down that road. Heat got me too. But I started carrying a little bottle of water everywhere. Told my buddy where I’d be. Got naloxone from the clinic next to the laundromat.
It’s not about being perfect. It’s about being alive tomorrow. You got this. One sip, one step, one day at a time.
CAROL MUTISO
December 21, 2025 AT 16:26Oh wow, so the government would rather let people die in their apartments than spend $50 million on something that actually works? How very American.
We’ll fund drones for surveillance but not cooling centers for people who use drugs. We’ll give tax breaks to billionaires but not electrolytes to the overheated.
It’s not a crisis of willpower. It’s a crisis of character. And we’re failing. Spectacularly.
Meanwhile, Vancouver’s doing it right. They’re saving lives. And we’re arguing about whether they deserve it.
Let me guess - next we’ll debate whether people should be allowed to breathe during a heatwave. Because why not make it a moral issue? It’s so much easier than fixing the system.
Erik J
December 22, 2025 AT 01:55Interesting. The part about gut bacteria changing drug metabolism under heat stress - is there any peer-reviewed data on that beyond the 2023 preprint from Stanford? I’ve been looking for longitudinal studies but haven’t found much.
Also, the 12-18% reduction in respiratory compensation - was that measured in controlled lab settings or field conditions? Just curious how applicable it is to real-world use.