When someone gets a kidney, liver, heart, or lung transplant, their body doesn’t know the new organ belongs. It sees it as an invader. To stop the immune system from attacking it, patients must take immunosuppressive drugs for life. These aren’t optional. Skip a dose, and rejection can happen - fast. But the cost of brand-name drugs like Prograf or CellCept can hit $2,000 a month. For many, that’s impossible to afford. That’s where generic immunosuppressive combinations come in.
What Are Generic Immunosuppressive Combinations?
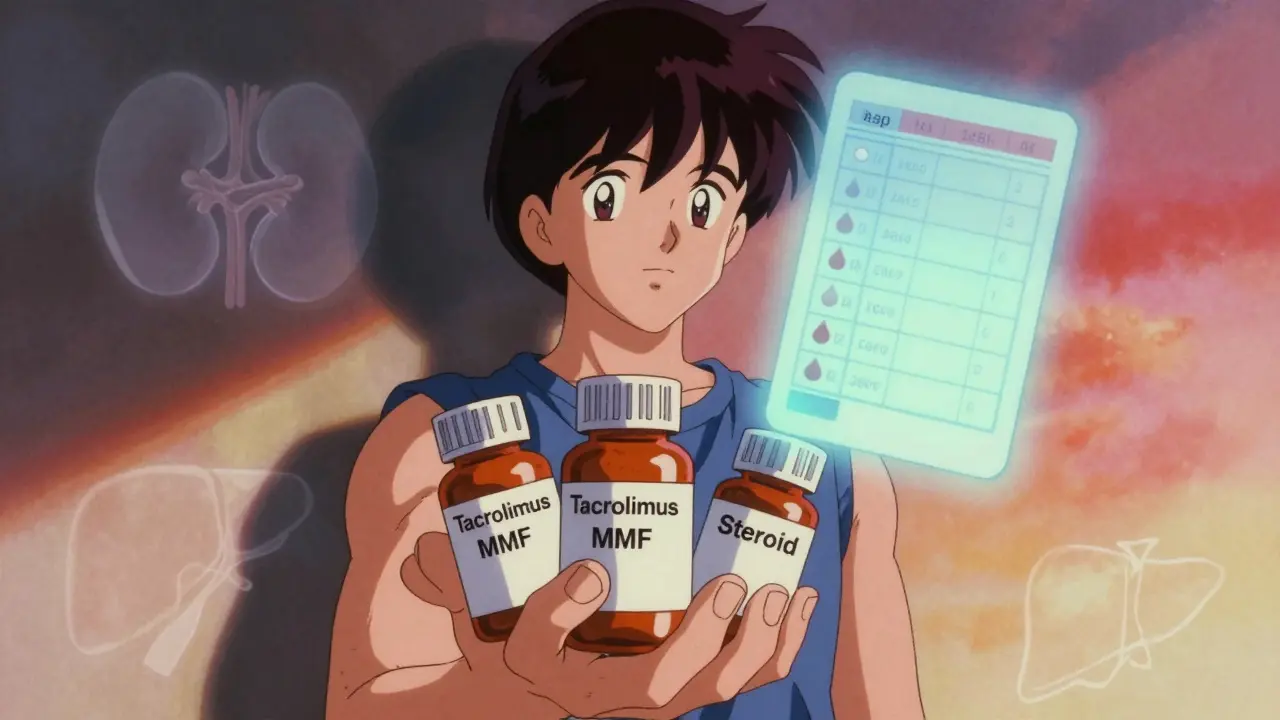
Generic immunosuppressive combinations are multi-drug regimens made up of lower-cost versions of the same medicines transplant patients have taken for decades. They work the same way. They’re not weaker. They’re not experimental. They’re FDA-approved copies of brand-name drugs like tacrolimus, mycophenolate, and sirolimus. The first generic tacrolimus hit the market in 2015 after Prograf’s patent expired. Since then, nearly every key immunosuppressant has a generic version.Most transplant patients take a triple combo: a calcineurin inhibitor (like tacrolimus or cyclosporine), an antimetabolite (like mycophenolate or mycophenolic acid), and sometimes corticosteroids. Today, all three components are available as generics. A typical monthly regimen might include generic tacrolimus, generic mycophenolate mofetil (MMF), and a low-dose steroid - all for under $600, compared to $4,000+ with brands.
How Effective Are They?
The big question: do they work as well?Yes - if managed right.
A 2022 study in the American Journal of Transplantation looked at over 12,000 kidney transplant patients. Those on generic tacrolimus had a 94.7% one-year graft survival rate. Those on the brand? 95.1%. The difference wasn’t statistically meaningful. Another study from the University of Maryland tracked lung transplant patients over eight years. Those on generic tacrolimus plus sirolimus lived longer on average than those on tacrolimus plus mycophenolate.
But here’s the catch: these drugs have a narrow therapeutic window. That means the difference between a safe, effective dose and a toxic one is small. Tacrolimus levels need to stay between 5 and 10 ng/mL. Sirolimus between 4 and 12 ng/mL. If levels dip too low, rejection kicks in. Too high, and you risk kidney damage, tremors, or even seizures.
Generic versions must meet FDA bioequivalence standards: their blood concentration must be within 80-125% of the brand. That’s a wide range. For a drug like tacrolimus, even a 15% drop in absorption can trigger rejection. That’s why switching from brand to generic isn’t just a pharmacy change - it’s a medical event.
Cost Savings Are Real - and Massive
Let’s break down the numbers.
Brand-name tacrolimus (Prograf) costs $1,800-$2,200 a month. Generic? $300-$400. That’s an 80% drop. Mycophenolate (CellCept) runs $1,200-$1,500 monthly. Generic MMF? $150-$250. Same with sirolimus (Zortress) - brand is $1,600, generic is $350.
For a patient on a full triple combo, switching to generics can save $1,500-$1,800 a month. That’s over $20,000 a year. For someone on Medicare or without insurance, that’s the difference between taking meds or skipping them.
According to IQVIA, 78% of new kidney transplant prescriptions in 2023 were for generic immunosuppressants. In 2016, it was 15%. That shift didn’t happen by accident. Medicare Part D now covers all transplant drugs, and hospitals are pushing generics to cut costs. Teva, Sandoz, and Mylan now control 75% of the generic market.

Not All Generics Are the Same
Here’s where things get tricky. Two generics of the same drug - say, tacrolimus - made by different companies aren’t always identical in how your body absorbs them. One might dissolve slower. Another might have different fillers that affect absorption.
Transplant centers have learned this the hard way. A 2022 FDA inspection found 12% of generic tacrolimus batches failed USP dissolution tests. That means the pill didn’t break down properly in the gut. The result? Unpredictable blood levels.
That’s why most transplant centers now require patients to stick with the same generic manufacturer once they switch. No switching back and forth between brands. No random substitutions at the pharmacy. Consistency matters more than cost savings here.
One transplant pharmacist in Ohio told me: “We see 30% more clinic visits in the first six months after a patient switches to generic. Their levels are all over the place. We have to adjust doses every two weeks.”
Who Should Use Generics?
Not every patient is a good candidate for a switch.
Patients who’ve been stable on brand-name drugs for years - especially those who’ve had rejection episodes in the past - are often advised to stay put. Why risk a change when the system is working?
But for new transplant recipients? Generics are now the standard of care. The American Society of Transplantation updated its guidelines in 2021 to recommend generic combinations as first-line therapy - as long as therapeutic drug monitoring (TDM) is tight.
Some combinations are better for specific cases. Sirolimus + tacrolimus is gaining traction for high-risk kidney transplant patients because it avoids steroids and cuts diabetes risk by 31%. A 2024 meta-analysis showed mTOR inhibitors like sirolimus lower post-transplant diabetes risk by 50% compared to calcineurin inhibitors.
But sirolimus isn’t for everyone. If you’ve had recent surgery or poor wound healing, it can delay recovery. Corticosteroids, though cheaper and effective, increase the risk of weight gain, bone loss, and cataracts. Many centers now use steroid-sparing regimens with generic tacrolimus and sirolimus to avoid those side effects.

The Monitoring Challenge
Switching to generics isn’t a one-time event. It’s a process.
Patients need blood tests every two weeks for the first month after switching. Then monthly for three to six months. Trough levels for tacrolimus, MMF, and sirolimus must be tracked like a clock. One patient in Texas switched to generic tacrolimus and saved $1,500 a month - but had three rejection episodes in the first year because her levels dropped below 5 ng/mL. She had to go back to the brand.
On the other hand, a Reddit user named “KidneyWarrior2020” wrote: “Generic MMF has worked perfectly for me for three years. No issues. Saved over $18,000.”
That’s the split. 68% of patients on the National Kidney Foundation forum reported success. But 22% had rejection or side effects that forced them back to brand-name drugs.
It’s not about the drug. It’s about the monitoring.
What’s Next?
The future of transplant care is moving toward even more cost-effective combinations. In May 2023, the FDA approved the first interchangeable biosimilar for belatacept (Nulojix), a newer immunosuppressant that could cut costs by 40%. KDIGO guidelines now recommend generic sirolimus as first-line for high-risk kidney patients.
Some centers are even testing protocols that could eventually let patients stop taking immunosuppressants altogether. One clinical trial (NCT00078559) used alemtuzumab induction followed by generic tacrolimus and sirolimus. A small group of patients were able to stop all drugs after two years - without rejection.
For now, though, most transplant patients will keep taking these drugs for life. And for them, generic combinations aren’t just a cost-saving trick. They’re a lifeline.
95% of transplant centers plan to increase generic use in the next five years. The data shows it’s safe. The math shows it’s necessary. The only question is: are we doing enough to support patients through the transition?
Are generic immunosuppressants as safe as brand-name drugs?
Yes - when used correctly. Generic versions of tacrolimus, mycophenolate, and sirolimus are FDA-approved and must meet strict bioequivalence standards. Studies show they maintain the same graft survival rates as brand-name drugs. However, because these drugs have a narrow therapeutic window, switching requires close monitoring. Blood levels must be checked frequently, especially in the first three months. Without proper tracking, there’s a higher risk of rejection or toxicity.
Can I switch from brand to generic on my own?
No. Never switch without consulting your transplant team. Your doctor and pharmacist must coordinate the switch. They’ll check your current blood levels, choose a specific generic manufacturer, and schedule frequent lab tests after the change. Random substitutions at the pharmacy can cause dangerous fluctuations in drug levels. Most transplant centers require a formal transition plan - not a pharmacy refill change.
Why do some patients have rejection after switching to generics?
Rejection after switching usually happens because drug levels dropped too low. Generic drugs must be within 80-125% of the brand’s absorption, which is a wide range. One generic might be absorbed slightly slower than another. If your body absorbs less of the drug, your blood levels fall below the safe threshold. That’s why consistent sourcing - sticking with the same generic manufacturer - is critical. Also, some patients need dose adjustments after switching. Skipping follow-up blood tests increases rejection risk.
Which generic immunosuppressant combination is most common?
The most common combination is generic tacrolimus plus generic mycophenolate mofetil (MMF), with or without low-dose steroids. This regimen is used in about 64% of kidney transplant patients. It’s proven, effective, and now mostly generic. For high-risk patients, tacrolimus plus generic sirolimus is becoming more popular because it avoids steroids and reduces diabetes risk. The choice depends on the organ, patient history, and risk of rejection.
Do generic immunosuppressants have more side effects?
The side effects themselves - like tremors, high blood pressure, or stomach upset - are the same as the brand-name versions because they contain the same active ingredient. However, some patients report more side effects after switching. That’s usually because their blood levels changed. Too high = more toxicity. Too low = rejection symptoms that feel like side effects. It’s not that generics are more toxic - it’s that they require more careful dosing. Frequent monitoring helps prevent this.
Is there financial help for generic immunosuppressants?
Yes. While brand-name manufacturers used to offer the best patient assistance programs, 65% of generic manufacturers now offer copay cards and discounts. Medicare Part D covers all transplant medications, and many states have transplant-specific programs. Some nonprofit organizations, like the National Kidney Foundation, also help with medication costs. Always ask your transplant pharmacist - they know which programs are available for your specific drugs.
What Patients Need to Do
If you’re on immunosuppressants, here’s what you need to know:
- Never switch manufacturers without telling your transplant team.
- Keep all follow-up blood tests - even if you feel fine.
- Know your target drug levels. Ask your pharmacist for them.
- Keep a log of side effects, missed doses, or changes in how you feel.
- Ask about copay assistance - you might qualify for help.
Transplant care isn’t just about the surgery. It’s about the daily grind of taking pills, getting blood drawn, and staying on top of your health. Generics make that grind more manageable - financially and emotionally. But they demand more attention, not less.

Rosalee Vanness
January 13, 2026 AT 23:55Let me tell you, I’ve been on generic tacrolimus for five years now - and I swear, it’s like my body finally stopped screaming at me. I used to cry in the pharmacy aisle every month, staring at that $2,100 bill like it was a ransom note. Now? I pay less than my Netflix subscription. But here’s the thing nobody talks about: consistency. I switched from one generic to another because my insurance changed, and boom - tremors, nausea, sleepless nights. My doc had to re-tweak everything. Now I’m locked in with the same manufacturer, same batch, same pharmacy. It’s not glamorous, but it’s survival. I keep a little notebook: date, dose, blood level, how my hands shook that day. It’s my quiet rebellion against a system that treats life-saving meds like commodities. And yeah, I’m not the loudest voice on this thread - but I’m still here. Breathing. Alive. Thanks to generics that didn’t break me.
And if you’re thinking of switching? Don’t just nod and walk out of the clinic. Ask for the manufacturer name. Write it down. Treat it like your favorite coffee brand - because it is. Your life depends on it.
I used to think I was just a transplant patient. Now I know I’m a pharmacokinetic detective. And I’m kinda proud of that.
Also - I’ve never once missed a blood test. Not even when I was sick. Not even when I was broke. Because I learned the hard way: your body doesn’t care about your budget. It only cares about your trough levels.
So yeah. Generics saved me. But only because I showed up for them.
And if you’re reading this and you’re scared? You’re not alone. I was too. But I’m still here. And I’m not going anywhere.
Keep going. You’ve got this.
- Rosalee, still alive, still testing, still grateful.
mike swinchoski
January 14, 2026 AT 03:38People don’t realize generics are just cheap knockoffs. You think your body can’t tell the difference? Bullshit. I’ve seen patients crash after switching. It’s not science - it’s gambling with organs. If you can afford brand, take brand. No excuses.
Angel Tiestos lopez
January 14, 2026 AT 11:48bro. i just wanna say 🙏🏽 i switched to generic tacrolimus last year and my bank account cried tears of joy 😭💸
but also my body? kinda mad at first. tremors, weird dreams, felt like my insides were rearranging themselves 🤯
then my doc said ‘stick with the same brand’ and boom - peace. like my liver finally said ‘ok cool, we good.’
also i found out my pharmacy was swapping generics like trading cards. they got slapped with a warning. so now i bring my own pills in a little ziplock. yes, i’m that guy. no regrets.
generics aren’t magic. they’re medicine. and medicine needs discipline. not just money.
peace out, transplant fam. you’re all warriors. 🫡
Acacia Hendrix
January 15, 2026 AT 20:50It’s fundamentally irresponsible to equate bioequivalence with therapeutic equivalence in narrow-therapeutic-index agents. The 80–125% FDA bioequivalence window is not a clinical safety buffer - it’s a regulatory loophole that commodifies life-sustaining pharmacotherapy. The pharmacokinetic variance between generic manufacturers introduces unacceptable heterogeneity in Cmax and AUC, which directly correlates with rejection risk in immunocompromised populations. Furthermore, the lack of post-marketing pharmacovigilance for generic immunosuppressants is a systemic failure of the FDA’s risk mitigation framework. Until mandatory therapeutic drug monitoring is standardized across all transplant centers - and until manufacturers are held to the same batch-to-batch consistency standards as innovator products - this practice remains ethically dubious. Cost savings should not be prioritized over biological fidelity.
James Castner
January 16, 2026 AT 00:20I’ve spent over two decades working in transplant care - from the ICU to the outpatient clinic - and I’ve seen the raw truth of this issue. What we’re talking about here isn’t just about cost. It’s about dignity. It’s about a single mother in Ohio who can now afford to take her daughter to school instead of choosing between meds and groceries. It’s about a veteran in Texas who didn’t have to sell his truck to stay alive. Yes, the science is nuanced. Yes, monitoring is critical. But the data doesn’t lie - when managed properly, generics save lives at a fraction of the cost. And let me be clear: those who claim they’re ‘unsafe’ haven’t sat with the families who’ve lost loved ones because they couldn’t afford the brand. We don’t have the luxury of elitist hesitation. We have a moral imperative to scale access. The American Society of Transplantation got it right. The FDA got it right. Now it’s time for every hospital, every pharmacist, every insurer to get it right too. This isn’t a compromise. It’s justice.
Adam Rivera
January 17, 2026 AT 03:11Hey, I’m just a guy who got a liver transplant five years ago. I’m on generics now. I save like $1,700 a month. I used to work part-time at a gas station just to pay for meds. Now I can actually go out with my wife on weekends. I don’t care if it’s generic or brand - I care that I’m still here. And I’m not gonna let someone tell me I’m less of a survivor because I didn’t pay $2,000 for my pills. We’re all just trying to live, you know? Thanks for the info. Keep it real.
Damario Brown
January 19, 2026 AT 00:56lol. 78% of prescriptions are generic now? that's because insurance companies forced it. nobody cares about patient outcomes anymore. just profit. i saw a guy get rejected because his generic was from a different batch. his levels dropped. he died. no one even blinked. the system is broken. and you people are just happy you got a discount. sad.
Priyanka Kumari
January 20, 2026 AT 23:37I’m from India, and my brother got a kidney transplant last year. He’s on generic tacrolimus and MMF. The cost was less than $50/month. We didn’t have insurance, but we found a nonprofit that helped with shipping. His levels are stable. No rejection. He’s back to teaching math. I just want to say - this isn’t just an American issue. People all over the world are surviving because generics exist. Don’t let fear silence the truth: access to medicine is a human right. Thank you for writing this. It helps so many of us feel less alone.
Avneet Singh
January 21, 2026 AT 14:56Generic immunosuppressants are a regulatory failure masked as cost-saving innovation. The bioequivalence standards are archaic and clinically inadequate for drugs with a therapeutic index narrower than lithium. Any clinician who endorses this without mandatory pharmacogenomic screening is practicing negligent medicine. The data cherry-picked in this post ignores the 22% rejection cohort - a statistically significant failure rate. This isn’t progress. It’s pharmaceutical austerity dressed in virtue signaling.
James Castner
January 23, 2026 AT 00:22Thanks for the perspective, Priyanka. Your brother’s story is exactly why we need to amplify voices beyond the U.S. - this isn’t a luxury. It’s a global health equity issue. And Damario, I hear your anger. I’ve lost patients too. But the answer isn’t to retreat into brand-name privilege. It’s to demand better monitoring, better tracking, better support systems - not to deny people the chance to live. We don’t fix broken systems by denying access. We fix them by making them better for everyone. That’s the work we’re doing now. And it’s working.