When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But what if it doesn’t? Behind many of the quiet failures of generic drugs are deep-rooted problems in manufacturing plants - problems that aren’t always visible to patients, but are tracked closely by regulators, pharmacists, and doctors.
What Goes Wrong in Generic Drug Manufacturing?
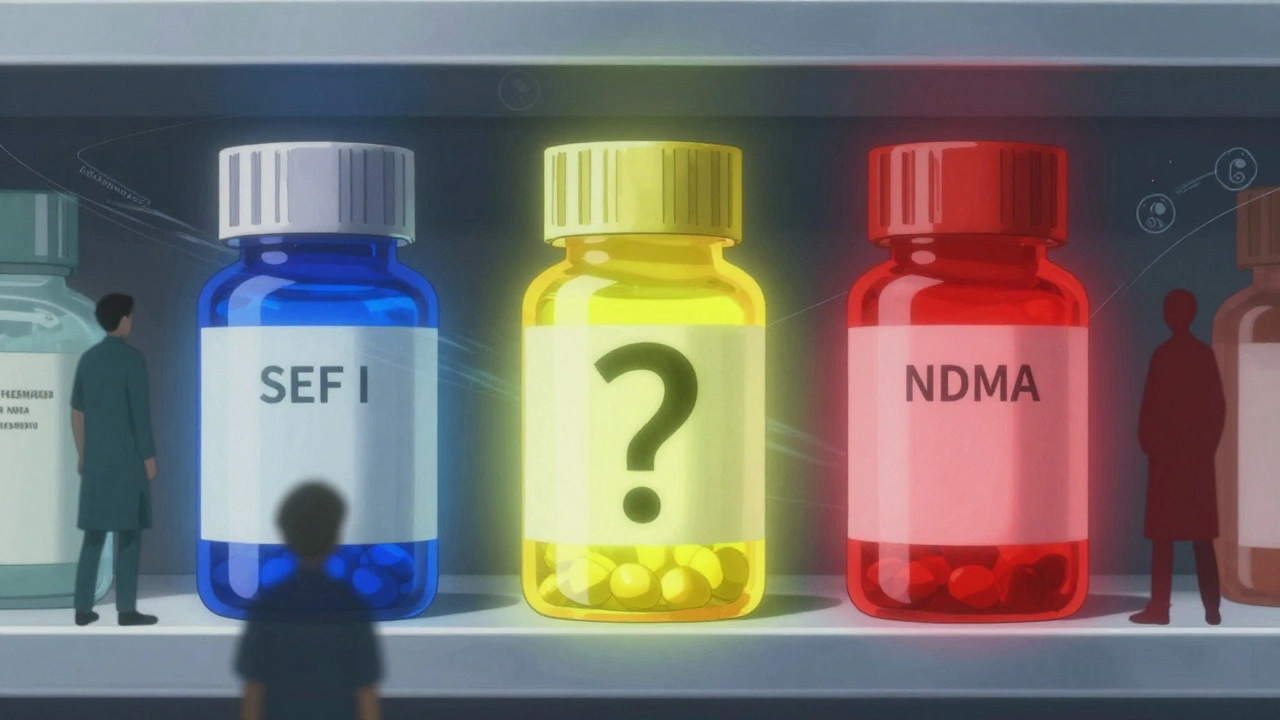
Generic drugs are supposed to be exact copies of brand-name medicines. They contain the same active ingredient, in the same strength, and should deliver the same results. But between the lab and the bottle, things can go wrong. The biggest culprit? Failure to follow Current Good Manufacturing Practices (cGMP). These aren’t suggestions - they’re legal requirements. When manufacturers skip steps, cut corners, or ignore quality checks, the result is pills that don’t dissolve properly, contain toxic impurities, or vary too much in potency from batch to batch.One of the most alarming examples came in 2018, when the FDA found N-nitrosodimethylamine (NDMA) - a probable human carcinogen - in blood pressure medications like valsartan. The contamination traced back to a single plant in China, where a change in the chemical process created the impurity. Over 2.1 million patients were exposed. That wasn’t an accident. It was a failure in process design, testing, and oversight.
Other common problems include:
- Inadequate analytical methods - labs using outdated or inaccurate tests to measure drug strength
- Poor packaging - containers that let in moisture or light, degrading the drug before it’s even taken
- Insufficient stability data - no proof the drug stays effective past a few months
- Unreliable raw materials - sourcing active ingredients from suppliers with no quality controls
These aren’t hypothetical risks. In 2022, 18.7% of FDA inspection findings were tied to flawed testing methods. Another 12.3% were due to packaging failures. And 15.6% of facilities couldn’t prove their drugs stayed stable over time. That’s not a glitch - it’s a pattern.
Why Are Foreign Plants More Likely to Fail?
Over 80% of the active ingredients in U.S. drugs come from abroad - mostly from China and India. But inspections tell a troubling story. In 2022, FDA inspections found 28.6% more violations at Chinese facilities and 19.3% more at Indian facilities compared to U.S. plants.Why? One reason is timing. The FDA can show up unannounced at American factories. But for foreign sites, they have to give advance notice - sometimes months ahead. That gives plants time to clean up, hide documents, or temporarily hire extra staff to pass inspection. A 2023 study from Ohio State University found that generic drugs made in India were linked to 23.7% more severe adverse events than those made in the U.S.
Then there’s the sheer scale of the problem. In 2016, the Government Accountability Office found the FDA had never inspected nearly 1,000 foreign facilities that shipped ingredients to the U.S. Even today, the agency inspects only about 13% of foreign plants each year - despite the fact that 73% of finished drugs are made overseas.
It’s not just about numbers. In one 2022 inspection at an Intas Pharmaceuticals plant in Gujarat, India, an employee was caught pouring acid into a trash can full of quality control documents. That wasn’t a one-off mistake. It was a sign of systemic disregard for accountability.
Who’s Affected - And How?
Patients don’t always know when a generic drug fails. There’s no flashing warning on the bottle. But healthcare providers do. A 2022 survey by the American Society of Health-System Pharmacists found that 67.3% of hospital pharmacists had seen at least one therapeutic failure with a generic drug in the past year. Nearly half of those failures involved products made in India.Some drugs are riskier than others. Narrow Therapeutic Index (NTI) drugs - like warfarin, levothyroxine, and tacrolimus - have a tiny margin between effective and toxic doses. Even small variations in potency can cause serious harm. In 2022, NTI generics accounted for 37% of all Complete Response Letters from the FDA - meaning the agency blocked approval because they couldn’t guarantee safety.
One study published in JAMA Internal Medicine found that generic tacrolimus capsules from certain manufacturers showed 28.4% higher variability in blood concentration than the brand version. For transplant patients, that’s life-or-death.
And it’s not just efficacy. The FDA’s adverse event database recorded 1,842 reports between 2019 and 2022 tied directly to generic drug quality. One batch of nitroglycerin tablets from Impax Laboratories failed to dissolve properly - leading to heart attack patients not getting relief when they needed it most.
The Business Side: Profit vs. Safety
The generic drug market is huge - worth over $420 billion in 2022. But it’s also fiercely competitive. Prices have dropped 18.3% per year since 2018. To stay profitable, many manufacturers have slashed costs - including quality control budgets, which fell by 22.7% on average during that same period.That’s where the real conflict lies. Building a reliable, compliant manufacturing system isn’t cheap. Implementing a full Quality by Design (QbD) program - which builds safety into every step of production - costs an average of $2.7 million per facility and takes 18 to 24 months. Only 23.8% of generic manufacturers have adopted it fully.
Meanwhile, the cost to file a generic drug application with the FDA has jumped from $129,250 in 2018 to $210,500 in 2023 - a 63% increase. Many small manufacturers can’t afford both the fees and the upgrades. So they do the bare minimum to get approval - and hope they don’t get caught.
What’s Being Done - And Is It Enough?
The FDA is trying to catch up. In 2022, it issued 147 warning letters for cGMP violations - up 28.5% from the year before. The 2022 FDA User Fee Reauthorization added $56.7 million to boost foreign inspections, aiming to go from 1,200 to 1,800 per year by 2027.The European Medicines Agency (EMA) went further. Since January 2023, it has conducted unannounced inspections at all foreign facilities supplying the EU. The result? A 41.2% increase in critical findings - meaning they’re finally seeing what’s really happening on the factory floor.
The FDA’s 2023-2027 Strategic Plan says it will prioritize inspections of high-risk facilities - especially those making NTI drugs or complex formulations. It also plans to require 100% more stability data and 75% more bioequivalence studies for complex generics. That’s a big shift. For years, regulators accepted minimal data. Now, they’re demanding proof.
But experts say it’s still not enough. Dr. Ameet Nathwani of Sanofi called the current inspection model “fundamentally broken.” Dr. Helen Winkle, former FDA deputy commissioner, pointed out that the agency tests only 0.02% of imported drug shipments in its labs. That’s like checking one car out of every 5,000 on the highway for safety.

What You Can Do
As a patient, you can’t inspect a factory. But you can stay informed. If you’re on a critical medication - like blood thinners, thyroid pills, or immunosuppressants - ask your pharmacist:- Which company made this generic version?
- Has there been a recall or warning for this batch?
- Is there a brand-name alternative if this one doesn’t seem to work?
Keep track of how you feel. If a generic drug you’ve taken for years suddenly stops working - or causes new side effects - don’t assume it’s all in your head. Report it to your doctor and to the FDA’s MedWatch program.
And if you’re a healthcare provider, push for transparency. Demand batch-level data. Ask for stability reports. Don’t accept “it’s FDA-approved” as enough. Approval is just the start - not the finish line.
The Bigger Picture
This isn’t just about pills. It’s about trust. When patients lose confidence in generics, they pay more for brand-name drugs - or skip doses altogether. When hospitals can’t rely on consistent supply, they face dangerous shortages. In 2022, 58.7% of all drug shortages were caused by quality problems at foreign plants.The system is under strain. Globalization made drugs cheaper, but it also made them harder to control. The solution isn’t to stop making generics - it’s to make them right. That means more inspections, better data, real accountability, and manufacturers who see quality as a competitive advantage, not a cost to cut.
For now, the message is clear: not all generics are equal. And knowing that could save your life.
Are all generic drugs unsafe?
No, not all generic drugs are unsafe. Many are manufactured to high standards and work just as well as brand-name versions. The problem isn’t generics themselves - it’s specific manufacturers, especially those with poor oversight, weak quality systems, or a history of violations. Most FDA-approved generics are safe and effective. But the risk is higher with drugs made in facilities that have been flagged for cGMP violations.
How can I tell if my generic drug is from a problematic manufacturer?
You can check the FDA’s website for warning letters and recalls. Look up the manufacturer name on your prescription label and search for it in the FDA’s Enforcement Reports. If you’re on a critical medication like warfarin or levothyroxine, ask your pharmacist if the maker has had recent inspections or recalls. Some pharmacies also track manufacturer reliability internally - don’t be afraid to ask.
Why do some generic drugs work differently than others?
Even though generics are required to be bioequivalent, small differences in inactive ingredients, manufacturing processes, or dissolution rates can affect how the drug is absorbed. This is especially true for Narrow Therapeutic Index (NTI) drugs, where even a 5% variation can cause side effects or treatment failure. If you switch between two generics and notice a change in how you feel, talk to your doctor - it’s not just in your head.
What’s being done to fix these problems?
The FDA is increasing inspections of foreign plants and requiring more data for complex generics. The EMA now conducts unannounced inspections, which has exposed more violations. Industry experts are pushing for mandatory Quality by Design (QbD) systems and better data integrity controls. But progress is slow. Funding, staffing, and diplomatic barriers still limit how much oversight is possible.
Should I avoid generic drugs altogether?
No. Generic drugs save billions of dollars each year and make essential medications accessible. The key is to be smart. For routine medications like statins or antibiotics, generics are usually fine. For critical drugs like those for heart conditions, epilepsy, or transplants, ask your doctor if a brand-name version or a more reliable generic is available. Don’t assume all generics are the same - ask questions, monitor your response, and report any changes.


James Kerr
December 3, 2025 AT 05:27Man, I just found out my blood pressure med was made in China. 😳 I’ve been taking it for two years and never felt a thing… until last week. Now I’m dizzy all day. Guess I’m switching back to brand-name, even if it costs me half my paycheck.
Albert Essel
December 4, 2025 AT 10:17The systemic failure in foreign drug manufacturing is not a surprise to anyone who has followed FDA inspection reports over the past decade. The issue is not globalization per se, but the lack of enforceable international regulatory alignment. Without mandatory unannounced inspections globally, we are essentially trusting profit motives over public health.
Charles Moore
December 6, 2025 AT 06:31I get that generics save money, and I’m all for affordability. But when your life depends on a pill dissolving just right, cutting corners shouldn’t be an option. My uncle had a transplant and switched generics-ended up in the ER with rejection symptoms. Turns out, the new batch had 30% higher variability. That’s not a glitch. That’s negligence.
Gavin Boyne
December 8, 2025 AT 02:12So let me get this straight: we outsource the most critical part of our healthcare-life-saving meds-to factories that get a heads-up before inspectors show up? And we wonder why people die? 😏 The FDA is basically playing whack-a-mole with a blindfold on. Meanwhile, the CEOs of these companies are sipping margaritas on beaches while patients choke on under-dosed pills. Capitalism: it’s a feature, not a bug.
Rashi Taliyan
December 9, 2025 AT 13:21As someone from India, I am heartbroken. Our pharmaceutical industry has done so much good-giving the world affordable medicine, saving millions. But yes, there are bad apples. Not all factories are like this. Please don’t judge an entire nation because of a few corrupt plants. We are proud of our science, but we need global accountability-not blame.
Kara Bysterbusch
December 11, 2025 AT 07:10It’s staggering to consider that the FDA inspects less than 13% of foreign facilities annually, despite 73% of finished drugs being manufactured overseas. This isn’t regulatory oversight-it’s a statistical fantasy. When you consider that a single batch of nitroglycerin can fail to dissolve, and patients die because of it, we are not just failing in policy-we are failing in moral responsibility.
Rashmin Patel
December 11, 2025 AT 10:25Look, I work in pharma logistics in Mumbai, and I’ve seen the pressure firsthand. Companies are told to cut costs, so they cut testing, they cut documentation, they cut safety. And guess what? The FDA doesn’t even know half of what’s happening because they rely on self-reported data. We need blockchain traceability from raw material to pill bottle-no more paper trails. And if the FDA can’t do it, let’s make the EU lead the way and force global compliance. This isn’t about nationalism-it’s about survival.
sagar bhute
December 13, 2025 AT 07:36Stop pretending this is a surprise. India and China are dumping garbage pills into the US market because they know you’re too lazy to care. You want cheap meds? Fine. But don’t cry when your thyroid meds stop working or your blood thinners turn you into a walking bruise. This is what happens when you outsource your health to the lowest bidder. Wake up. It’s not a conspiracy-it’s capitalism.
Cindy Lopez
December 15, 2025 AT 02:55Wow. So much text. Can we just say: some generics are bad, the FDA is slow, and you should ask your pharmacist? Done.