MAOI Cold Medicine Safety Checker
Check if your cold medicine is safe to use with MAO inhibitors. Even a single dose of decongestants like ephedrine can trigger a life-threatening hypertensive crisis when combined with MAOIs.
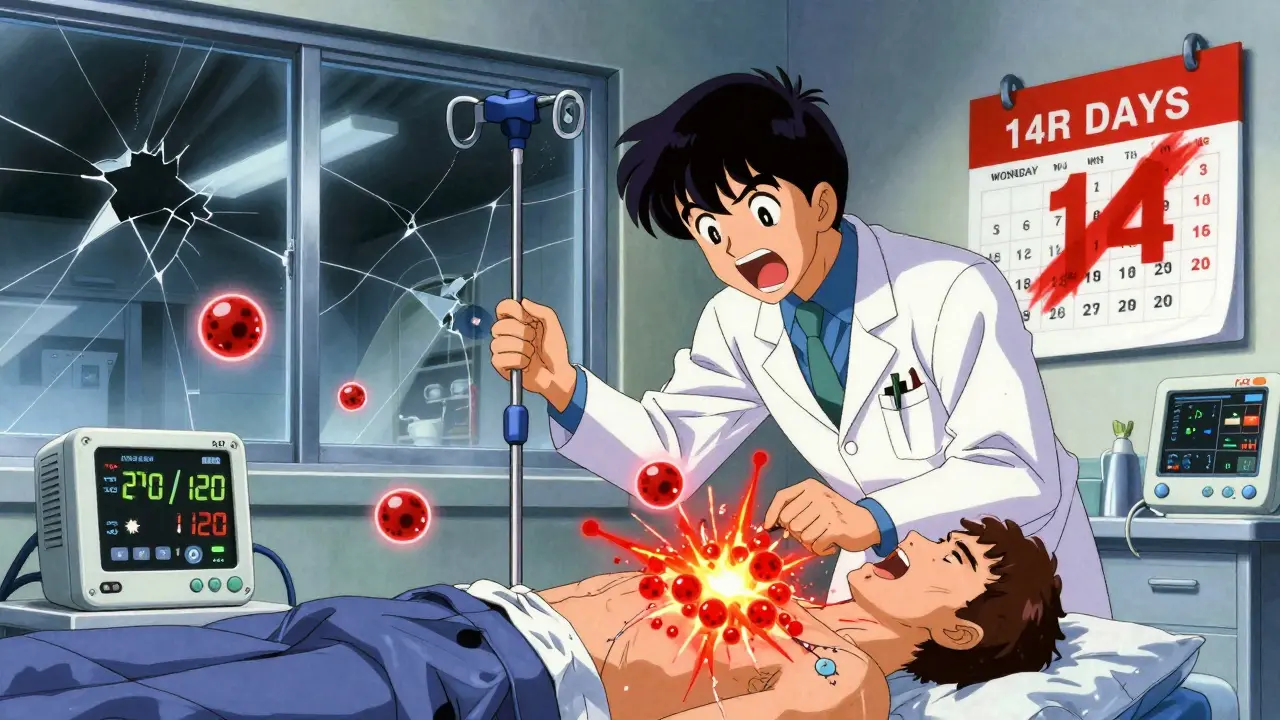
One pill. One dose of an over-the-counter cold medicine. One moment of ignorance. And suddenly, your blood pressure spikes to dangerous levels-240 mmHg-in under an hour. Your head feels like it’s going to explode. Your vision blurs. You can’t breathe. This isn’t a horror movie. It’s a real, documented, and preventable medical emergency that happens every year when people mix ephedrine with MAO inhibitors.
What Exactly Happens When Ephedrine Meets MAOIs?
Ephedrine is a stimulant. It’s in some cold and asthma meds. It makes your heart race, your blood vessels tighten, and your blood pressure rise. That’s why it works for congestion. But when you’re taking an MAO inhibitor-a type of antidepressant like phenelzine (Nardil), tranylcypromine (Parnate), or isocarboxazid (Marplan)-your body loses its ability to break down excess norepinephrine. That’s the chemical your brain uses to signal your blood vessels to constrict.Normally, your body keeps norepinephrine in check. But MAOIs shut down the enzyme that does that job. Then ephedrine comes in and dumps even more norepinephrine into your system. No brakes. No safety valve. The result? A runaway surge of pressure in your arteries. This isn’t a mild spike. It’s a hypertensive crisis. Systolic pressure can hit 200 mmHg or higher in minutes. That’s like driving your car at 120 mph with worn-out brakes.
The First Known Case: A Warning Ignored
Back in 1965, a 49-year-old woman took a single 25 mg dose of ephedrine for a cold. She was already on nialamide, an MAOI. Within 30 minutes, she collapsed. She had a subarachnoid hemorrhage-bleeding in her brain. She died. The doctor who wrote the case report, Dr. M.S. Hirsch, called it a direct result of the drug interaction. That report was published in JAMA. It was clear. It was urgent. And yet, 60 years later, people are still dying from this.Why? Because ephedrine is still in OTC products. Because doctors forget to warn patients. Because patients don’t read labels. Because “it’s just a cold medicine” feels harmless.
How Much Ephedrine Is Dangerous?
You don’t need a lot. As little as 12.5 mg of ephedrine can trigger a crisis if you’re on an MAOI. That’s half the dose in many cold pills. Common brands like Bronkaid, Primatene, and some generic decongestants contain 25 mg to 120 mg per tablet. One pill. That’s enough. And it’s not just ephedrine. Pseudoephedrine, phenylephrine, and phenylpropanolamine-the other decongestants-do the same thing. They’re all off-limits.And it’s not just pills. Some weight-loss supplements, energy drinks, and herbal products still contain ephedra or ephedrine alkaloids. Even if the label says “natural,” it’s still dangerous with MAOIs.
What Does a Hypertensive Crisis Feel Like?
It doesn’t sneak up. It hits like a truck.- Severe, sudden headache-often starting at the back of your head and radiating forward
- Blurred or lost vision, seeing spots or “white out”
- Heart pounding like it’s trying to escape your chest
- Chest pain that feels like a vise tightening
- Profuse sweating, even if you’re cold
- Nausea, vomiting, dizziness
- Neck stiffness, confusion, seizures
One Reddit user from 2022 described it: “Felt like my head was going to burst. I screamed. I couldn’t move. My vision went white for 10 seconds.” That’s not exaggeration. That’s a real patient’s account. In 2018, a 32-year-old man on phenelzine took a 25 mg ephedrine tablet and suffered an intracranial hemorrhage. He survived-but barely.
This Risk Doesn’t Go Away When You Stop the MAOI
Here’s what most people don’t know: the danger doesn’t vanish when you stop taking the MAOI. Because these drugs bind to the enzyme permanently. Your body has to grow new enzymes to replace them. That takes two to three weeks.So if you stop your MAOI on Monday, you still can’t take ephedrine until late next month. Many patients think, “I haven’t taken it in a week-I’m fine.” They’re wrong. And they end up in the ER.
Even newer MAOIs like selegiline (Emsam) patch aren’t completely safe. At higher doses, they still block MAO-A, the enzyme that breaks down norepinephrine. Only the lowest patch dose (6 mg/24hr) reduces the risk-but it’s not zero. And if you’re on a higher dose? Don’t risk it.
What About Reversible MAOIs Like Moclobemide?
Moclobemide is different. It’s reversible. It only blocks the enzyme for 24 to 48 hours. That means the risk is lower. But it’s not gone. You still need to avoid ephedrine. And you still need to wait at least 48 hours after your last dose before taking any decongestant. The threshold for triggering a crisis is higher-around 100 mg of tyramine-but ephedrine doesn’t need tyramine to cause trouble. It directly releases norepinephrine. So even with moclobemide, the combo is unsafe.Emergency Treatment: What Doctors Do
If someone’s in a hypertensive crisis from this interaction, time is everything. Standard high blood pressure meds like nifedipine are dangerous here. They can cause your pressure to crash too fast, leading to stroke.Doctors use intravenous phentolamine. It’s a fast-acting alpha-blocker that opens up blood vessels. It’s the only safe option. But it requires hospital care. You can’t treat this at home.
And even with treatment, outcomes aren’t always good. Between 2015 and 2020, the FDA recorded 37 cases of this interaction. Nine ended in death. Most of those people were taking OTC meds they thought were harmless.

Why This Keeps Happening
MAOIs are prescribed to fewer than 1% of depressed patients today. But they’re still vital for people who don’t respond to SSRIs. About half a million Americans are on them. The problem? Most prescribers aren’t psychiatrists. A primary care doctor might write an MAOI prescription without knowing the full risks. A pharmacist might not flag the interaction. A patient might pick up a cold medicine without telling anyone they’re on an antidepressant.Studies show 22% of MAOI patients still get a contraindicated drug within 30 days of starting treatment. That’s not just a mistake. It’s a system failure.
How to Stay Safe
If you’re on an MAOI:- Absolutely avoid all ephedrine, pseudoephedrine, phenylephrine, and phenylpropanolamine. Check every cold, flu, allergy, and weight-loss product.
- Use saline nasal sprays, humidifiers, or antihistamines like loratadine instead of decongestants.
- Wait at least 14 days after stopping an irreversible MAOI before using any stimulant or decongestant.
- Carry an MAOI alert card. The Mayo Clinic recommends it. 87% of patients who used one avoided dangerous interactions.
- Tell every doctor, dentist, and pharmacist you’re on an MAOI-even for a tooth extraction or minor surgery.
If you’re not on an MAOI but think you might be: don’t guess. If you’ve been prescribed an antidepressant and aren’t sure what kind, check the label or call your pharmacy. Don’t risk it.
Is There Any Hope for Safer Options?
Yes. In March 2023, the FDA approved a new reversible MAOI called befloxatone. Early data shows it has a 90% lower risk of hypertensive crisis because it’s short-acting and selective. It’s not on the market yet, but it’s a sign that science is trying to fix this.Researchers are also testing wearable BP monitors that alert patients to sudden spikes-early warning systems for people on MAOIs. These aren’t magic. But they could save lives.
Still, the bottom line hasn’t changed: ephedrine and MAOIs don’t mix. Ever. No exceptions. No “just this once.” No “I’ve been fine before.” This isn’t a gamble. It’s a guaranteed risk.
What If You Accidentally Take Them Together?
If you’ve taken ephedrine while on an MAOI-even one pill-call 911 or go to the nearest ER immediately. Don’t wait. Don’t call your doctor first. Don’t hope it passes. This isn’t a stomachache. This is a ticking time bomb.And if you’re a caregiver, family member, or friend of someone on an MAOI: learn the signs. Keep their meds list updated. Check their OTC purchases. You might be the one who saves their life.
Can I take Sudafed if I’m on an MAOI?
No. Sudafed contains pseudoephedrine, which acts just like ephedrine. It forces norepinephrine release and can trigger a hypertensive crisis when combined with MAOIs. Avoid all decongestants unless your doctor specifically says it’s safe-and even then, proceed with extreme caution.
How long after stopping an MAOI is it safe to use ephedrine?
For irreversible MAOIs like Nardil or Parnate, wait at least 14 days. For reversible MAOIs like moclobemide, wait 48 hours. But many experts recommend waiting 21 days to be absolutely safe, since enzyme regeneration can vary by person. Never assume you’re safe after just a week.
Are there any safe cold medicines for people on MAOIs?
Yes-but only non-decongestant options. Antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) are generally safe. Saline nasal sprays, humidifiers, and honey for coughs are also good choices. Avoid anything with “decongestant,” “sinus,” “cold,” or “multi-symptom” in the name unless you’ve confirmed the ingredients with a pharmacist.
Can I drink alcohol while on an MAOI?
It’s risky. Alcohol can raise blood pressure and interact with MAOIs, especially red wine and aged cheeses. But the bigger danger is combining it with decongestants or stimulants. If you’re on an MAOI, avoid alcohol unless your doctor says it’s okay. Even then, limit it.
Why aren’t MAOIs banned if they’re so dangerous?
Because they work when nothing else does. For people with treatment-resistant depression, atypical depression, or severe anxiety, MAOIs can be life-changing. The risk is real-but so is the benefit. That’s why they’re still prescribed, but only under strict supervision. The goal isn’t to eliminate them, but to use them safely.


Gray Dedoiko
December 22, 2025 AT 17:22I had no idea one little cold pill could do this. My uncle was on an MAOI and took Sudafed thinking it was 'just a decongestant.' He ended up in the ICU for three days. Never thought to connect the dots until now. Thanks for laying this out so clearly.
Aurora Daisy
December 24, 2025 AT 11:31Of course Americans die from this. You people take pills like candy and then blame the medicine. In the UK, we have actual regulations. You can't just walk into a pharmacy and grab a bottle of ephedrine like it's gummy bears. This is what happens when you treat your body like a video game with infinite lives.
Katie Taylor
December 24, 2025 AT 22:10This is why I’m telling everyone I know about this. If you’re on an MAOI, I’m sending you this post. No jokes. No 'I’ve been fine before.' This isn’t a suggestion-it’s a lifeline. I’ve seen people lose their minds over this. Don’t be one of them. You’re worth more than a quick fix for a stuffy nose.
Payson Mattes
December 26, 2025 AT 12:04Wait… did you know the FDA knew about this since the 70s but let it slide because Big Pharma makes more money selling MAOIs and decongestants together? They don’t want you to know that the real danger is in the labels being too small. I’ve got a friend who works at a compounding pharmacy-he says they print warnings in 4pt font on purpose. And don’t even get me started on how the WHO is suppressing data on reversible MAOIs…
Isaac Bonillo Alcaina
December 26, 2025 AT 13:35You misused 'hypertensive crisis' as a synonym for 'emergency.' It's a clinical syndrome, not a synonym for 'bad.' Also, you said '240 mmHg'-that's not systolic, that's diastolic. Systolic can't be 240 and be survivable. And you misspelled 'phenylephrine' twice. This post is dangerously inaccurate despite its good intent. Fix your facts before you scare people.
Bhargav Patel
December 26, 2025 AT 18:18There is a profound irony in our modern pharmacological age: we have developed molecules capable of altering the very architecture of human consciousness, yet we still rely on the crudest of behavioral cues-reading labels-to prevent catastrophe. The tragedy is not in the chemical interaction, but in the systemic failure to embed safety into the culture of consumption. We treat medicine as a commodity, not a covenant. And in doing so, we reduce the sacred act of healing to a transactional gamble.
Sidra Khan
December 26, 2025 AT 20:00Okay but have you tried just… not taking the MAOI? 😏
siddharth tiwari
December 27, 2025 AT 02:07my cousin took ephedrine and died and no one said nothin. the government is coverin it up. they dont want us to know how bad these drugs are. i read it on a forum. its not just ephedrine its the chemicals in the water too. you gotta drink spring water and avoid wifi if you on MAOI. they put it in the air to control us.
Jeffrey Frye
December 27, 2025 AT 04:38So let me get this straight-you’re telling me that a 25mg pill of ephedrine can kill someone on an MAOI, but the same person can safely take 100mg of tyramine from blue cheese? That’s not a medical risk, that’s a statistical inconsistency. Also, why is phentolamine the gold standard? It’s not even FDA-approved for this indication. Sounds like anecdotal medicine dressed up as protocol.
Andrea Di Candia
December 27, 2025 AT 16:04This is the kind of post that makes me believe in the power of community. I’ve been on selegiline for 3 years and I never knew I had to wait 21 days after stopping. I thought 14 was enough. Thank you for not just listing the facts, but for making me feel like I’m not alone in this. If you’re reading this and you’re on an MAOI-breathe. You’re not broken. You’re just navigating a system that wasn’t built for you. We’re figuring it out together.
Joseph Manuel
December 27, 2025 AT 17:00The data presented lacks statistical context. Of the 500,000 individuals on irreversible MAOIs in the United States, how many experience this interaction annually? The FDA's 37-case dataset over five years implies an incidence rate of less than 0.0015% per year. While the outcome is severe, the probability is statistically negligible. Risk communication must be calibrated to prevent undue alarm.
Andy Grace
December 27, 2025 AT 21:47My mum’s on phenelzine. She reads labels like a forensic accountant now. I printed out a list of banned ingredients and taped it to the fridge. We also keep a bottle of saline spray right next to the cough medicine. Small steps, but they matter. Thanks for the reminder-this stuff sticks with you.
Delilah Rose
December 29, 2025 AT 12:54I just want to say that I used to think people who took MAOIs were just ‘dramatic’ or ‘overly cautious’-until my best friend had a near-fatal reaction after taking a cold tablet she thought was ‘safe’ because it said ‘non-drowsy.’ She spent two weeks in the hospital. Her vision didn’t come back for months. Now I check every single ingredient in every single product, even the ones from the gas station. It’s exhausting, but it’s worth it. If you’re on an MAOI, you’re not being paranoid-you’re being smart. And if you’re not on one but know someone who is? Please, be their second pair of eyes. We need more people like that.
Spencer Garcia
December 29, 2025 AT 14:40Saline spray + humidifier + honey = your new best friends. No decongestants. Ever. Save this post. Share it. Print it. Your life depends on it.
Abby Polhill
December 30, 2025 AT 23:06Just had a 45-minute convo with my pharmacist about this. She said the real issue is that OTC meds aren’t required to have MAOI interaction warnings on the front-only in the ‘Drug Facts’ section, which 90% of people don’t read. It’s a regulatory blind spot. They’re not hiding it-they’re just assuming you’ll read the tiny print. We need a universal red flag symbol for MAOI contraindications. Like the skull and crossbones, but for blood pressure.