For years, getting generic medications meant driving to a pharmacy, waiting in line, and paying whatever price the system set-often with hidden fees and confusing insurance math. But starting in 2024 and accelerating through 2025, a quiet revolution is reshaping how Americans buy their everyday prescriptions. Direct-to-consumer generic pharmacies are cutting out the middlemen, offering lower prices, faster delivery, and simpler processes-all through a smartphone app or website. This isn’t just another online pharmacy trend. It’s a structural shift in how drugs reach patients.
What Exactly Is a Direct-to-Consumer Generic Pharmacy?
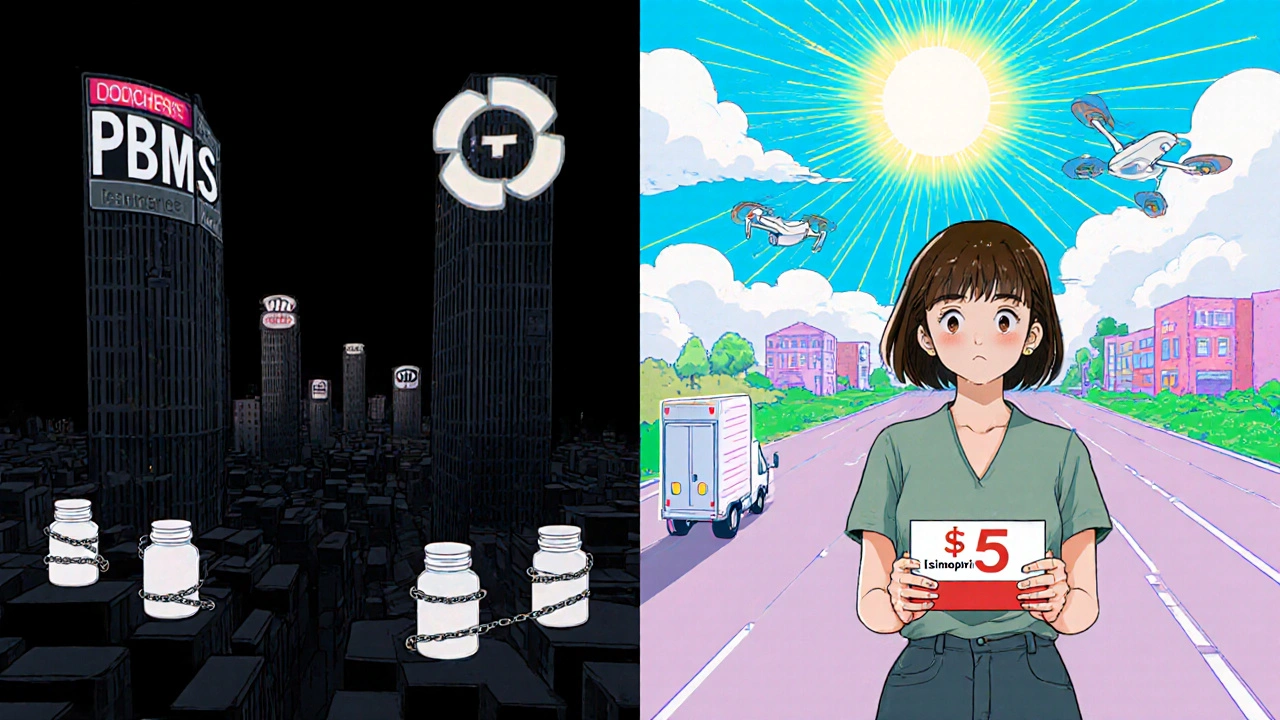
A direct-to-consumer (DTC) generic pharmacy sells FDA-approved generic medications straight to patients, skipping traditional layers like pharmacy benefit managers (PBMs), wholesalers, and brick-and-mortar pharmacies. Think of it like buying a phone directly from Apple instead of through Verizon or Best Buy. You cut out the middlemen, and in most cases, you pay less.
Companies like Ro, Hims & Hers, and Honeybee Health built their businesses around this model. They don’t manufacture drugs-they partner with licensed generic manufacturers and handle everything else: telehealth consultations, e-prescriptions, secure shipping, and refill reminders. By 2025, Ro alone processed over 2.1 million prescription orders in the first quarter, mostly for generics like metformin, lisinopril, and sertraline.
These platforms don’t rely on insurance billing. Instead, they offer transparent cash prices-often 30% to 50% lower than retail pharmacy prices. For example, a 30-day supply of generic lisinopril 10mg costs $15 at a local CVS. On Ro, it’s $5. Same drug. Same manufacturer. Just a different path to your door.
How These Models Work: The Tech Behind the Delivery
Behind every smooth DTC pharmacy experience is a complex tech stack built for speed and compliance. It starts with a simple online questionnaire. You answer questions about your condition, current meds, and allergies. Then, a licensed telehealth provider reviews your info and, if appropriate, sends an e-prescription directly to the pharmacy’s internal system.
From there, the medication is picked, packed, and shipped-usually within 24 to 48 hours. Most platforms use HIPAA-compliant cloud systems to store data, AI-powered chatbots to remind you to take your pills, and real-time tracking so you know exactly when your order will arrive. Integration with EHR systems like Epic and Cerner lets providers see your refill history, reducing duplication and errors.
Unlike traditional pharmacies, these platforms don’t just fill orders-they manage care. Subscriptions auto-renew. Refills are triggered based on usage patterns. If you miss a dose, you get a text. If your blood pressure readings are high, the system flags it for a provider follow-up. This isn’t just convenience-it’s adherence engineering.
Why Generic Drugs? Why Now?
Generic drugs make up over 90% of all prescriptions filled in the U.S., but they’ve long been the forgotten stepchild of the pharmaceutical industry. Brand-name companies get headlines and ad budgets. Generics? They’re treated as commodities.
But that’s changing. Generic manufacturers realized they could bypass the PBM rebate system entirely. PBMs claim they negotiate lower prices, but in 2024, they pocketed $28 billion in gross profits from rebates-while patients still paid high out-of-pocket costs. DTC platforms cut that noise. They buy generics in bulk directly from manufacturers and sell at net cost, with no hidden markups.
President Trump’s May 2025 executive order on international drug pricing pushed this further. It required manufacturers to match lower global prices and encouraged DTC sales. While the order focused on brand-name drugs, it created a regulatory green light for all DTC models-including generics. Suddenly, investors saw a path to scale.
Who’s Winning? The Players in the Market
The DTC generic space isn’t dominated by Big Pharma. It’s led by agile digital health startups:
- Ro: The largest player, with 2.1 million Q1 2025 orders. Focuses on chronic condition meds-blood pressure, cholesterol, diabetes, depression.
- Hims & Hers: Built on men’s and women’s health, but now offers over 100 generic prescriptions. Known for sleek app design and fast delivery.
- Honeybee Health: Targets patients on high-deductible plans. Offers price transparency tools and free shipping on orders over $25.
- Blink Health: Works with local pharmacies to fulfill orders, keeping costs low. Popular with Medicare Advantage users.
Big Pharma companies like Eli Lilly and Pfizer are also entering-but not with generics. Their DTC platforms (LillyDirect, PfizerForAll) focus on expensive brand-name drugs like Ozempic and Viagra. They’re using DTC to control pricing and collect patient data, not to compete on price. That’s why the real disruption for everyday patients is happening in the generic space.
Real Savings, Real Problems
Users report real savings. A 2025 Drug Channels survey found 73% of patients using DTC services for chronic conditions improved their adherence. One Reddit user, MedSavvy2025, saved $417.50 a year on generic blood pressure meds. Another saved $120 on antidepressants through Blink Health.
But it’s not perfect. Trustpilot reviews for Honeybee Health show a 3.8/5 rating. Common complaints? Delivery delays (42% of negative reviews), limited medication availability (38%), and slow customer service (29% say responses take over 48 hours). Some users miss having a pharmacist on-site to answer quick questions. A Johns Hopkins study flagged 17 cases where potential drug interactions might have been caught by a retail pharmacist-but went unnoticed in DTC models.
Insurance integration is another headache. Most DTC platforms don’t bill insurance. That’s good if you’re on a high-deductible plan. But if you’re on Medicare or Medicaid, you can’t use these services for covered drugs. You’re stuck paying cash-even if your insurance would’ve paid most of it.
The Regulatory Maze
Running a DTC pharmacy isn’t just about tech and pricing. It’s a legal minefield. To operate legally, a company needs a pharmacy license in all 50 states and Washington, D.C. That process takes 14 to 18 months and costs over $2.3 million in legal and compliance fees.
Plus, every state has different rules about telehealth, prescription validity, and shipping controlled substances. The National Association of Boards of Pharmacy says 47 states require specific DTC licensing as of early 2025. Companies like Ro spent years building compliance teams before launching.
And then there’s the Anti-Kickback Statute and Stark Law. If a company offers discounts or free shipping to patients who use their service, regulators could see it as a bribe to steer business away from traditional pharmacies. The Department of Justice is already investigating a few DTC platforms for potential violations. No charges yet-but the shadow is there.
What’s Next? Hybrid Models and Bigger Changes
Experts agree: DTC won’t replace traditional pharmacies. Instead, it’s forcing them to adapt. CVS and Walgreens are now testing their own cash-price generic programs. Some insurers are partnering with DTC platforms to offer subsidized pricing for members with high-deductible plans.
By 2026, we’ll likely see hybrid models: you order your generic metformin online, but pick it up at your local CVS if you need it faster. Or your doctor sends a prescription to both your retail pharmacy and a DTC platform-you choose the cheaper option.
Pharmaceutical companies are also rethinking their supply chains. Techspert’s June 2025 report found some manufacturers are creating “ring-fenced” production lines just for DTC orders. That means even if wholesalers run out of stock, your DTC order still ships on time.
Should You Use a DTC Generic Pharmacy?
If you’re paying cash for generics, especially for chronic conditions, it’s worth trying. You’ll likely save 30-50%. The process is simple: sign up, answer a few questions, get your prescription, wait a couple days, and refill automatically.
But avoid it if:
- You rely on insurance coverage for your meds
- You take multiple complex drugs and need frequent pharmacist consultations
- You need your medication within 24 hours
- You’re uncomfortable with digital-only care
For everyone else-especially those on high-deductible plans, without insurance, or tired of surprise pharmacy bills-DTC generic pharmacies offer a rare win: lower prices, no hassle, and real control over your healthcare.
Are DTC generic pharmacies safe?
Yes-if you use a licensed platform. Reputable DTC pharmacies like Ro, Hims & Hers, and Honeybee Health are accredited by the National Association of Boards of Pharmacy (NABP) and use FDA-approved generics. All prescriptions require a telehealth consultation. The biggest risk isn’t drug safety-it’s missing pharmacist advice on drug interactions, especially if you take multiple medications.
Can I use insurance with DTC pharmacies?
Most cannot bill insurance directly. They operate on cash-pay pricing, which is often cheaper than your insurance copay-especially if you have a high-deductible plan. Some platforms like Blink Health let you submit receipts for reimbursement, but you’ll need to handle it manually. Medicare and Medicaid patients generally can’t use these services for covered drugs.
How fast do DTC generic pharmacies deliver?
Most deliver within 2 to 5 business days. Ro and Hims & Hers often ship within 24-48 hours after your telehealth visit. This is slower than walking into a local pharmacy, but faster than waiting for a PBM to approve a claim. If you need medication urgently, keep a small supply on hand or use a traditional pharmacy for emergencies.
Do DTC pharmacies offer all generic drugs?
No. Most focus on high-volume, chronic-condition generics like blood pressure, cholesterol, diabetes, and antidepressants. You won’t find rare or specialty generics (like certain autoimmune drugs) on these platforms. If your medication isn’t listed, you’ll need to go through a traditional pharmacy or specialty distributor.
Why are DTC generic prices so much lower?
Because they cut out the middlemen. Traditional pharmacies get drugs through PBMs, wholesalers, and distributors-each adding fees and markups. DTC platforms buy directly from generic manufacturers, avoid insurance billing costs, and pass the savings to you. You’re paying the net price, not the inflated list price.
Final Thoughts: A Shift, Not a Fad
This isn’t just another app that delivers pills. It’s a fundamental challenge to a broken system. For too long, the cost of generic drugs was hidden behind layers of corporate deals and rebate games. DTC pharmacies are exposing that. They’re giving patients real choices, real savings, and real control.
Regulators will keep watching. Insurance companies will keep resisting. But patients? They’re already voting with their wallets. In Q3 2025, 27% of commercially insured Americans used a DTC pharmacy at least once. Among those with chronic conditions, that number jumped to 41%.
If you’re paying out of pocket for generics, it’s time to look beyond your local pharmacy. The old system isn’t broken-it’s been designed to profit from your confusion. The new model? It’s simple, transparent, and working.


Scott Macfadyen
November 17, 2025 AT 21:41Finally, someone’s cutting through the bullshit. I’ve been paying $47 for lisinopril at Walmart while my buddy on Ro pays $5. Same pill. Same factory. Just no middlemen sucking the air out of the room. This isn’t innovation-it’s basic math.
Chloe Sevigny
November 17, 2025 AT 22:18One must interrogate the epistemological underpinnings of this ‘disruption.’ The commodification of pharmacological care under the banner of ‘transparency’ merely reconfigures the neoliberal apparatus-replacing institutional gatekeeping with algorithmic arbitrage. The patient becomes a consumer, the medication a SKU. Where is the dignity in that? And who audits the telehealth ‘providers’ who rubber-stamp prescriptions in under 90 seconds?
Denise Cauchon
November 18, 2025 AT 23:38Canada’s got the same drugs, same prices, same pharmacies-yet we don’t need some Silicon Valley app to tell us how to live. This is American chaos dressed up as convenience. You think your ‘$5 metformin’ is a win? Wait till your insurance refuses to cover your next prescription because you ‘opted out’ of the system. You’re not saving money-you’re surrendering your safety net.
Andrea Johnston
November 19, 2025 AT 12:14Let’s be real-these apps are great until you need something that isn’t on their 100-item list. I’ve been on 7 different meds for 15 years. None of them are on Ro. And when I tried Honeybee for my thyroid med? ‘Out of stock.’ For 3 weeks. Meanwhile, my local pharmacist had it in 10 minutes. You think convenience is worth risking your stability? Don’t be naive.
Victoria Malloy
November 20, 2025 AT 03:58This is actually really encouraging. I’m on a high-deductible plan and the savings are life-changing. I used to skip doses because I couldn’t afford it. Now I take them every day. No drama. No stress. Just a notification saying ‘Your meds are on the way.’ It’s not perfect, but it’s better than what we had.
Alex Czartoryski
November 21, 2025 AT 21:07Oh wow, so now we’re supposed to trust some app that sends pills in a box with no human interaction? What happens when you have a reaction? Who do you call? The chatbot? ‘Hi, I’m experiencing dizziness and blurred vision-can you please recommend a different SSRI?’ No thanks. I’ll take my $15 copay and my actual pharmacist who remembers my dog’s name.
Gizela Cardoso
November 21, 2025 AT 22:11I’ve been using Blink for my statins since last year. Delivery’s usually on time, prices are insane, and I appreciate the refill reminders. I do miss being able to ask the pharmacist about grapefruit, though. Maybe they could add a live chat with a pharmacist? Just a thought.
Jonathan Gabriel
November 23, 2025 AT 14:59Wait-so you’re telling me these companies aren’t just cutting out PBMs but also avoiding state licensing requirements? That’s not innovation-that’s regulatory arbitrage. And the DOJ investigation? That’s not a rumor. I’ve seen the subpoenas. These guys are skating on thin ice. Don’t be fooled by the $5 lisinopril-it’s a Trojan horse.
Don Angel
November 25, 2025 AT 00:17I’ve used Ro for my blood pressure meds for 11 months now. No complaints. Delivery always comes in 2 days. No surprise bills. No insurance paperwork. I used to spend 45 minutes on the phone with my PBM just to get them to approve a refill. Now? I tap a button. And yes-I know the pharmacist isn’t there. But I also don’t need someone to tell me to take my pill. I’m an adult.
benedict nwokedi
November 25, 2025 AT 05:39This is all a CIA-backed operation to depopulate the elderly through controlled medication distribution. They’re not lowering prices-they’re consolidating data. Every time you sign up, they log your health, your habits, your triggers. Then they sell it to insurers who raise your premiums. And the ‘FDA-approved’ pills? Probably sourced from a warehouse in Mumbai. Look up the 2023 Senate hearing on foreign generic supply chains. They buried it.
deepak kumar
November 26, 2025 AT 09:02In India, we’ve had this for years-online pharmacies like 1mg and Pharmeasy. You order, they deliver, and prices are 70% lower than local stores. But we also have a strong culture of consulting doctors before switching. Don’t just jump because it’s cheap. Talk to your physician. Even if the app says ‘you’re good to go,’ your body might say otherwise.
Dave Pritchard
November 27, 2025 AT 00:58For anyone nervous about trying this: start with one med. Pick something simple, like metformin or lisinopril. Try it for a month. Compare the cost. See how the delivery works. If it’s smooth, expand. If not, go back. No pressure. This isn’t about abandoning traditional care-it’s about adding a better option. You’re not choosing between two worlds-you’re choosing what works for you.
kim pu
November 27, 2025 AT 10:39LOL they call this ‘transparency’? Bro, the ‘net cost’ is still a lie. Manufacturers sell to DTCs at a discount, but only if they agree to not sell to anyone else. That’s not competition-that’s a cartel with a mobile app. And don’t get me started on the ‘telehealth providers’ who are just temp nurses paid $15/hr to click ‘approve.’ This isn’t healthcare. It’s a pyramid scheme with pills.