Cumulative Drug Toxicity Calculator
This tool estimates your cumulative drug exposure based on your daily dose and duration. It compares your exposure to known safety limits for common medications. Note: This is for educational purposes only - always consult your doctor for medical advice.
Your Risk Assessment
Think about this: you’ve been taking the same pill every day for three years. No big deal, right? Your doctor prescribed it, it’s working, and you haven’t felt worse - until one day, out of nowhere, you’re exhausted, your skin turns yellow, or your heart starts skipping beats. That’s not a new problem. It’s an old one that finally caught up. This is cumulative drug toxicity - the quiet, slow build-up of harm from medications you thought were safe because they didn’t hurt you right away.
Why Some Drugs Don’t Hurt You… Until They Do
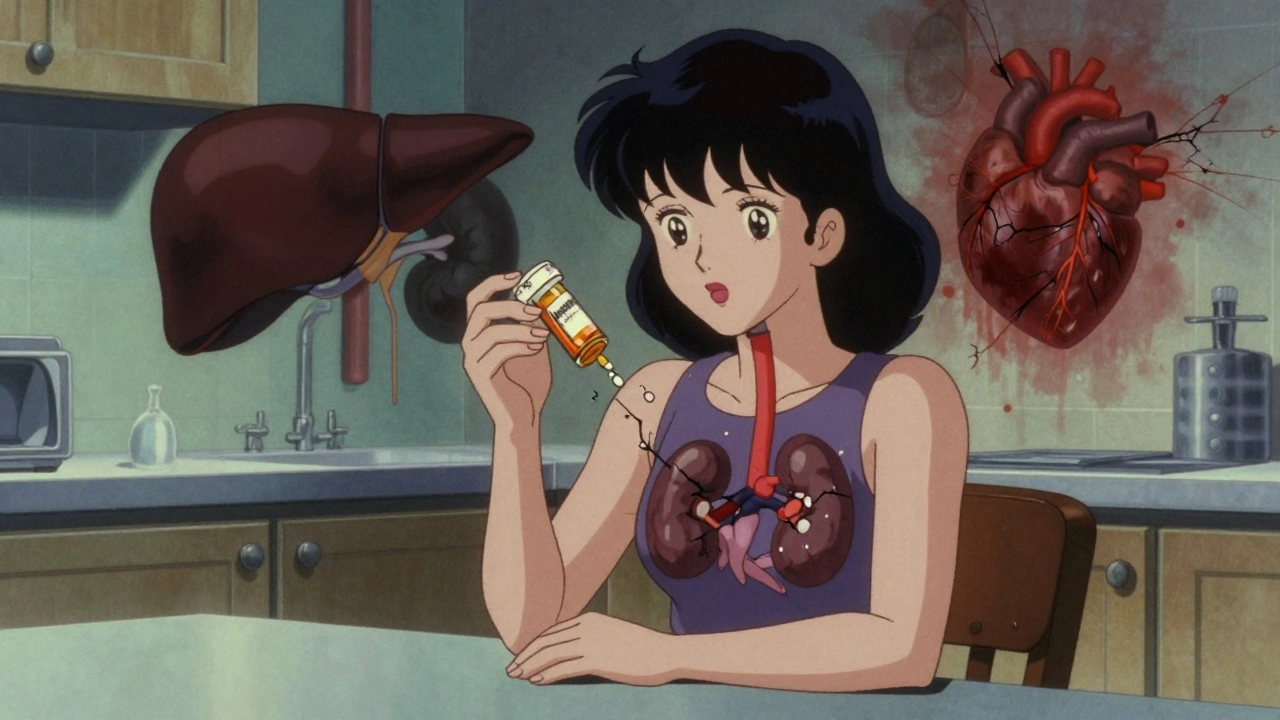
Not all drugs act like a sledgehammer. Some are more like a drip, drip, drip. Your body can handle a little bit - but only if it can get rid of it fast enough. When you take a drug every day, your liver and kidneys work to break it down and flush it out. But if the drug sticks around too long - if it’s fat-soluble, or if your organs are slowing down - it starts piling up. Like water filling a bathtub with the drain half-closed. Drugs with half-lives longer than 24 hours are the biggest culprits. That means it takes a full day or more for your body to clear just half the dose. Take amiodarone for heart rhythm issues? It can stay in your system for months. Digoxin for heart failure? Accumulates in muscle tissue. Even common antibiotics like doxycycline can build up if taken daily for weeks. Over time, those tiny amounts add up to a toxic load. And it’s not just prescription meds. Fat-soluble vitamins - A, D, E, K - can do the same thing. People popping high-dose vitamin D supplements for years? They’re at risk. Heavy metals like lead or mercury from environmental exposure? They stick in bones and fat for decades. Cumulative toxicity doesn’t care if you’re taking a pill or breathing in pollution - if your body can’t excrete it, it stores it.The Numbers Don’t Lie: It Gets Worse With Time
In cancer treatment, this isn’t theoretical. A 2019 study in the Journal of the National Cancer Institute tracked patients on targeted cancer drugs. In the first treatment cycle, about 25% had serious side effects. By the sixth cycle? That number dropped to just 2%. But here’s the catch: the total number of patients who had experienced serious toxicity by cycle six jumped to over 50%. Why? Because the damage wasn’t showing up in the first week - it was hiding, building, then exploding. It’s the same with chemotherapy. Anthracyclines, used for breast cancer and lymphoma, can wreck your heart. The safe lifetime limit? 450 mg/m². That’s not per year. That’s over your entire life. Go over that, and your risk of heart failure shoots up. And most patients don’t know it. They think, “I’m fine today, so I’m fine overall.” But the heart doesn’t complain until it’s too late. Even non-cancer drugs follow this pattern. A 2023 review found that 68% of adverse drug reactions in people over 65 were due to cumulative effects - not one big mistake, but years of small ones adding up. Lithium for bipolar disorder? Kidney damage creeps in over time. NSAIDs like ibuprofen? Stomach bleeding risk climbs with every month of daily use.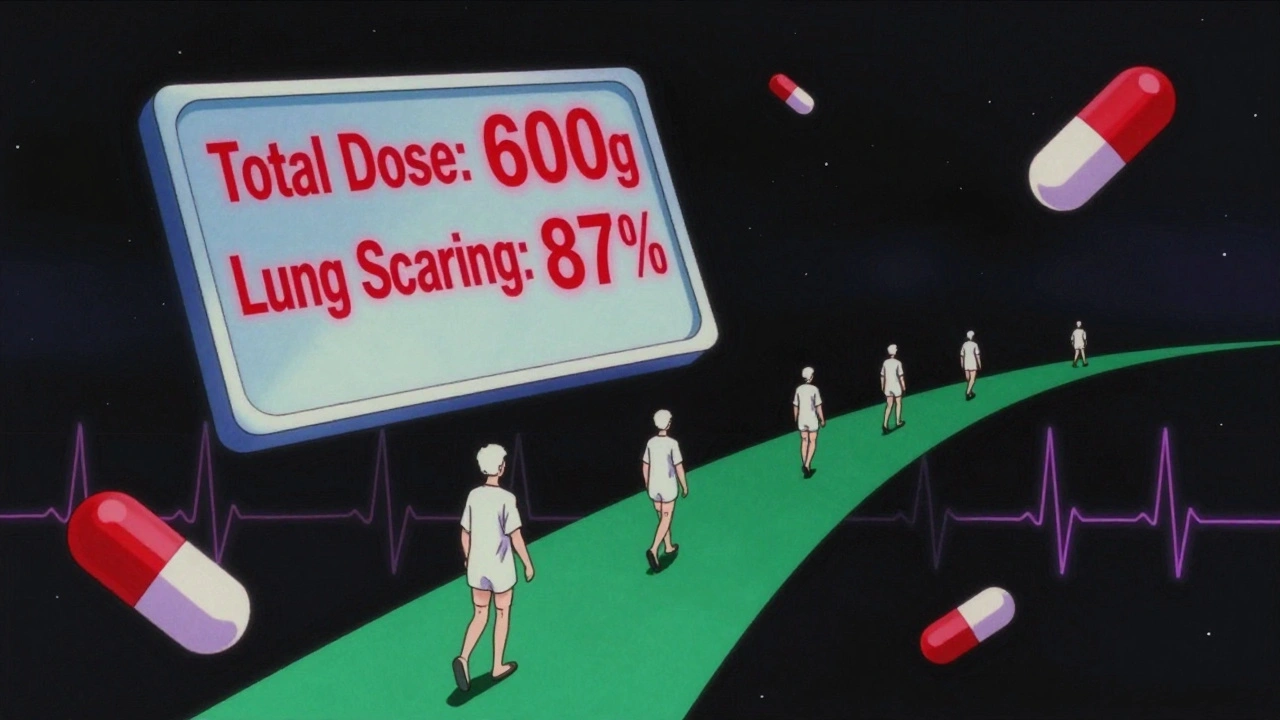
Who’s Most at Risk?
It’s not just the elderly. Though older adults are hit hardest - their livers and kidneys don’t work as well - anyone with chronic illness is vulnerable. Diabetes? Kidney damage slows drug clearance. Liver cirrhosis? Your body can’t metabolize meds properly. Hypothyroidism? Slows down how fast your liver breaks things down. Even your lifestyle matters. Alcohol? It competes with your liver for processing power. Poor nutrition? Your liver doesn’t have the enzymes it needs. Obesity? Fat-soluble drugs get trapped in fat tissue and slowly leak back into your bloodstream. And don’t forget drug interactions. Taking five meds? Each one can slow down how the others are cleared. A 2022 Medscape survey found that 82% of doctors saw cumulative toxicity cases where patients weren’t following up on blood tests or monitoring schedules. They didn’t realize the danger was creeping in.How Doctors Miss It - And How They Can Stop
Here’s the scary part: many doctors don’t track cumulative doses. They look at your latest blood test. They see “normal.” They think you’re fine. But that’s like checking the weather every morning and assuming the whole year is sunny. A real case from Reddit’s r/medicine: a patient on amiodarone for atrial fibrillation had normal blood levels every checkup. But after taking 600 grams total over five years, he developed severe lung scarring. His doctor never tracked the total dose. He didn’t know it was even a thing. The fix? Therapeutic drug monitoring. That’s not just checking blood levels once. It’s logging every dose, every refill, every change in weight or kidney function - and calculating the total exposure over time. Pharmacist-led programs have cut hospital admissions for drug toxicity by 29% in some health systems. The American Geriatrics Society’s Beers Criteria now lists 34 drugs with high cumulative risk in seniors - including antipsychotics, benzodiazepines, and certain painkillers - with clear lifetime dose limits. The FDA now requires cumulative toxicity warnings on 78% of new oncology drugs approved since 2022. The European Medicines Agency made it mandatory for all chronic-use drugs starting in January 2024. That’s progress. But only 38% of U.S. electronic health records can auto-calculate cumulative doses. Most doctors still do it by hand - if they do it at all.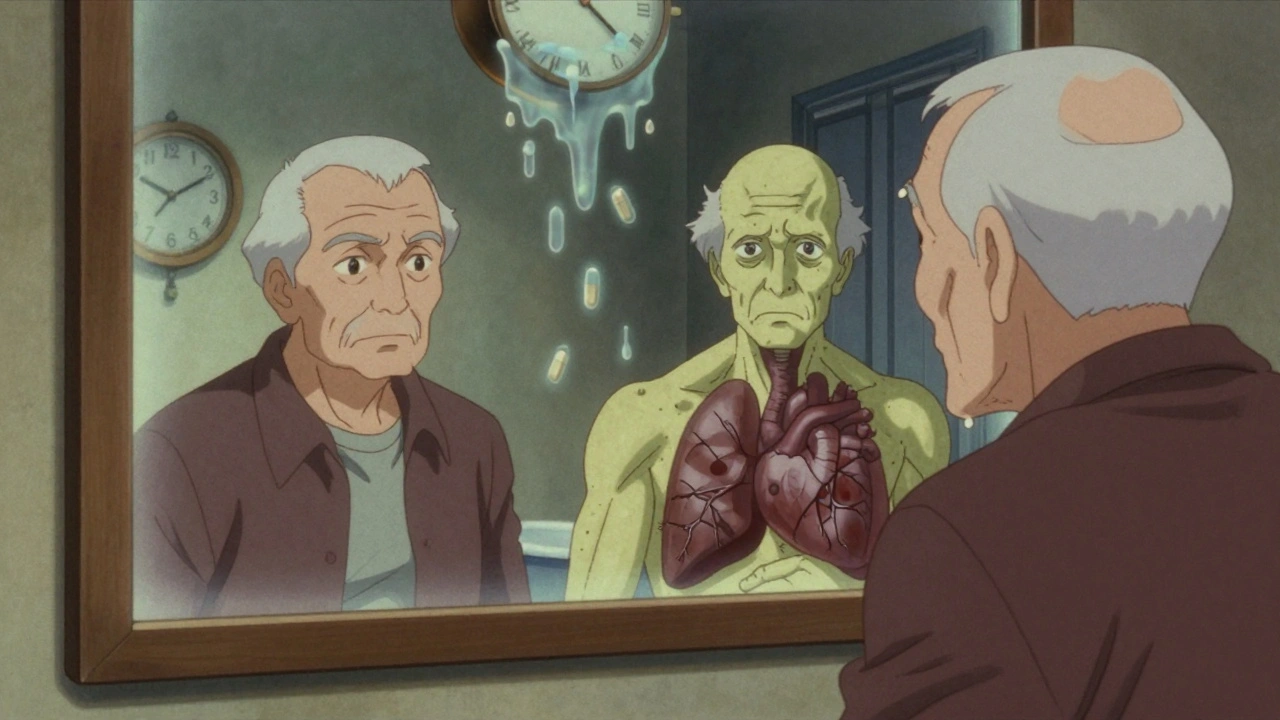
What You Can Do Right Now
If you’re on a medication long-term - especially for heart, mental health, pain, or autoimmune issues - ask these questions:- Is this drug known to build up in the body?
- Is there a lifetime or total dose limit I should know about?
- Do I need regular blood tests to check for organ damage - and how often?
- Could my kidney or liver function be affecting how this drug is cleared?
The Bigger Picture: Why This Matters
This isn’t just about one person’s heart or liver. Cumulative toxicity costs the U.S. healthcare system $1.2 billion a year in extra treatments, hospital stays, and lost work. It’s why cancer treatments get paused. Why patients switch drugs. Why some stop treatment entirely. New tools are coming. AI models at Memorial Sloan Kettering can now predict your personal risk of toxicity by analyzing 27 different factors - your genetics, age, weight, kidney function, even your diet. These tools aren’t in every clinic yet. But they’re coming. The real win? Prevention. Catching toxicity before it’s irreversible. That’s why tracking matters. That’s why education matters. That’s why you need to know your own body - not just what your doctor tells you. You don’t need to stop your meds. You need to understand them. And you need to be the one watching the clock - because no one else will.What is cumulative drug toxicity?
Cumulative drug toxicity happens when a medication builds up in your body over time because it’s absorbed faster than your body can remove it. This leads to increasing side effects that don’t show up right away - they develop slowly, often after months or years of use. Unlike acute reactions, which happen immediately, cumulative toxicity is silent until it’s serious.
Which drugs are most likely to cause cumulative toxicity?
Drugs with long half-lives, fat-soluble properties, or narrow therapeutic windows are most risky. Examples include amiodarone (heart), digoxin (heart), lithium (mental health), methotrexate (autoimmune), anthracycline chemotherapy (cancer), and fat-soluble vitamins like A and D. Antibiotics like doxycycline and aminoglycosides can also accumulate, especially with long-term use.
Can cumulative toxicity be reversed?
Sometimes, yes - but not always. If caught early, stopping the drug and supporting organ function (like hydration or liver support) can help. But damage to organs like the heart, lungs, or kidneys may be permanent. That’s why early detection through monitoring is critical. Once scarring or cell death occurs, it’s often irreversible.
How do doctors track cumulative drug doses?
In high-risk areas like oncology and cardiology, doctors use cumulative dose calculators built into electronic health records. They track total milligrams taken over months or years. For example, anthracycline chemotherapy has a strict lifetime limit of 450 mg/m². Pharmacists often lead this tracking. But in many clinics, it’s still done manually - if at all.
Are older adults more at risk for cumulative toxicity?
Yes. As we age, liver and kidney function decline, making it harder to clear drugs. Studies show 68% of adverse drug reactions in seniors are due to cumulative effects, not acute overdoses. The American Geriatrics Society Beers Criteria lists 34 medications with high cumulative risk for older adults and recommends strict dose limits.
Can lifestyle factors make cumulative toxicity worse?
Absolutely. Alcohol, poor nutrition, obesity, and other medications can all slow down how your body clears drugs. Alcohol competes with your liver for processing power. Fat tissue stores fat-soluble drugs, releasing them slowly over time. Taking multiple drugs can cause interactions that block metabolism. Even dehydration can reduce kidney clearance.
What should I do if I’ve been on a medication for years?
Ask your doctor: Is this drug known to accumulate? Is there a total lifetime dose limit? Do I need blood tests to check my liver, kidneys, or heart function? Keep a log of every dose you’ve taken. Bring it to appointments. Don’t assume you’re fine just because you feel okay - cumulative damage often has no symptoms until it’s too late.

Elizabeth Grace
December 3, 2025 AT 06:57I took amiodarone for 4 years. Didn't know it could wreck your lungs until I started coughing up dust like I smoked 2 packs a day. Turned out my CT scan looked like a tornado hit my chest. Docs never told me to track the total dose. Just said 'you're fine.' Well, I'm not. Now I'm on oxygen. Don't be me.
Steve Enck
December 5, 2025 AT 02:33The epistemological failure of modern pharmacovigilance lies in its reliance on cross-sectional biomarkers to assess longitudinal pharmacokinetic risk. The reductionist paradigm of 'normal lab values' obscures the emergent pathology of bioaccumulation-a phenomenon wherein homeostatic thresholds are incrementally breached across temporal scales imperceptible to clinical surveillance protocols. In essence, we mistake absence of acute distress for absence of damage.
Jay Everett
December 6, 2025 AT 02:09Bro, this is wild 😳 I’ve been popping vitamin D like candy since 2020. 5000 IU daily. Thought I was a health god. Now I’m reading this and my heart just dropped. My last bloodwork showed calcium levels creeping up. I’m scheduling a doc appt tomorrow. Thanks for the wake-up call 🙏 I’ll start logging every pill now. No more guessing!
मनोज कुमार
December 6, 2025 AT 13:02Joel Deang
December 7, 2025 AT 00:06yo i just realized i’ve been on ibuprofen every day for 7 years for my back. like… every single day. no breaks. i thought it was just ‘normal’ to pop 2 like a vitamin. now i’m scared to pee. my stomach’s been acting weird. i’m gonna stop. and yes i spelled that wrong. i’m typing on my phone with one hand while holding coffee.
Roger Leiton
December 8, 2025 AT 15:56This is one of those posts that makes you pause and just stare at your medicine cabinet. I’ve got 6 bottles on my nightstand. I never thought about how they’re stacking up over time. I’m printing out that checklist and bringing it to my next appointment. We need more awareness like this. Seriously. 👏
Laura Baur
December 9, 2025 AT 18:14It’s profoundly disturbing that we’ve normalized chronic polypharmacy as a lifestyle rather than a medical intervention. The medical-industrial complex profits from perpetual usage, not cure. Patients are conditioned to believe that ‘if it’s prescribed, it’s safe’-a dangerous myth that ignores the physiology of accumulation. We’ve outsourced responsibility to algorithms and EHRs that can’t even calculate cumulative doses. The blame isn’t on the patient. It’s on a system that commodifies compliance.
Jack Dao
December 10, 2025 AT 16:32Wow. Just wow. I’m sure you all think you’re so enlightened now that you’ve read this. But let’s be real-you’re just another person who Googled ‘drug toxicity’ after a weird symptom. Meanwhile, real doctors are trying to save lives. You’re not a patient. You’re a symptom-chaser. Go take a breath. And maybe stop reading Reddit for medical advice.
dave nevogt
December 11, 2025 AT 12:19I’ve been on lithium for 12 years. My kidneys are down to 45% function now. I didn’t know it was slow damage. I thought the blood tests were just routine. No one ever said ‘this is building up.’ I feel guilty. Not because I took my meds-but because I trusted the system too much. I wish someone had told me to track the total milligrams. I’d have asked harder questions. I’m not mad. Just… sad.
Arun kumar
December 11, 2025 AT 18:45Shannara Jenkins
December 13, 2025 AT 09:26Hey, if you’re reading this and you’re on long-term meds-take a deep breath. You’re not alone. This isn’t about panic. It’s about awareness. Start small: write down one pill you take daily. Look up its half-life. Then ask your doctor one question at your next visit. You don’t need to fix everything today. Just start paying attention. You’ve got this 💪
Zed theMartian
December 13, 2025 AT 10:51Oh great. Another ‘doomscrolling medical horror story’ designed to make people stop taking their prescriptions. Next you’ll tell me oxygen is toxic if you breathe it for 10 years. Newsflash: everything is toxic at high enough doses. The fact that you’re alive reading this means your body is doing its job. Stop being paranoid and start trusting your doctor.
Ella van Rij
December 15, 2025 AT 02:42Wow. So… you’re telling me that if I take a pill for 5 years, I might… die? Shocking. I guess I should’ve known that. I mean, who doesn’t know that drugs are poison? 😘 I’ll just stop my antidepressants. Totally fine. My therapist will be thrilled. Thanks for the life-saving insight, Captain Obvious.
ATUL BHARDWAJ
December 16, 2025 AT 15:13