Living with celiac disease isn’t just about avoiding bread or pasta. It’s about rebuilding your body from the inside out. For 1 in 100 people worldwide, eating gluten triggers an autoimmune attack that damages the small intestine, blocks nutrient absorption, and leaves you tired, weak, and sick-even if you feel fine on the surface. The good news? Once you cut out gluten completely, 95% of people see their symptoms vanish within days or weeks. The hard part? Making sure your body gets back what it lost-and staying gluten-free for life, even when no one’s watching.
What Gluten-Free Really Means
Gluten isn’t just wheat. It’s wheat, barley, rye, and any cross-contaminated grain. That means your oatmeal might be unsafe if it’s processed in the same facility as wheat. Your soy sauce? Often contains wheat. Even some medications and supplements use gluten as a filler. The FDA requires products labeled “gluten-free” to contain less than 20 parts per million (ppm) of gluten-enough to trigger symptoms in sensitive people. So “wheat-free” doesn’t mean “gluten-free.” Always read the full ingredient list.Safe grains include rice, quinoa, buckwheat, millet, amaranth, teff, corn, and certified gluten-free oats. Yes, oats are tricky. Most aren’t safe unless labeled certified gluten-free. Even then, about 5% of people with celiac disease react to avenin, the protein in oats. Start slow: try 50 grams per day, and monitor for bloating, fatigue, or diarrhea. If symptoms return, stop. No exceptions.
The Hidden Nutrient Crisis
When your small intestine is damaged by gluten, it can’t absorb nutrients properly. By the time most people are diagnosed, they’re already deficient in key vitamins and minerals. Here’s what’s missing in most newly diagnosed patients:- Iron: Found in 12-63% of patients at diagnosis. Causes fatigue, pale skin, and shortness of breath.
- Vitamin D: Deficient in 37-75% of people. Weakens bones and lowers immunity.
- Calcium: Low in 25-40%. Leads to bone loss and osteoporosis over time.
- Folate (B9) and Vitamin B12: Critical for red blood cell production and nerve function. Deficiencies cause brain fog and tingling in hands and feet.
- Magnesium: Often overlooked. Needed for muscle function, sleep, and energy. Many people still feel tired even after going gluten-free because their magnesium levels are still low.
Supplementing isn’t optional-it’s essential. Most doctors recommend:
- Iron: 18 mg daily for women, 8 mg for men (take with vitamin C to boost absorption)
- Calcium: 1,000-1,200 mg daily (split into two doses for better absorption)
- Vitamin D: 600-800 IU daily, but many need 2,000-5,000 IU to correct deficiency
- Folate: 400 mcg daily
- Vitamin B12: 250-500 mcg daily, or 1,000 mcg sublingual if absorption is poor
- Magnesium: 400 mg daily (glycinate or citrate form works best)
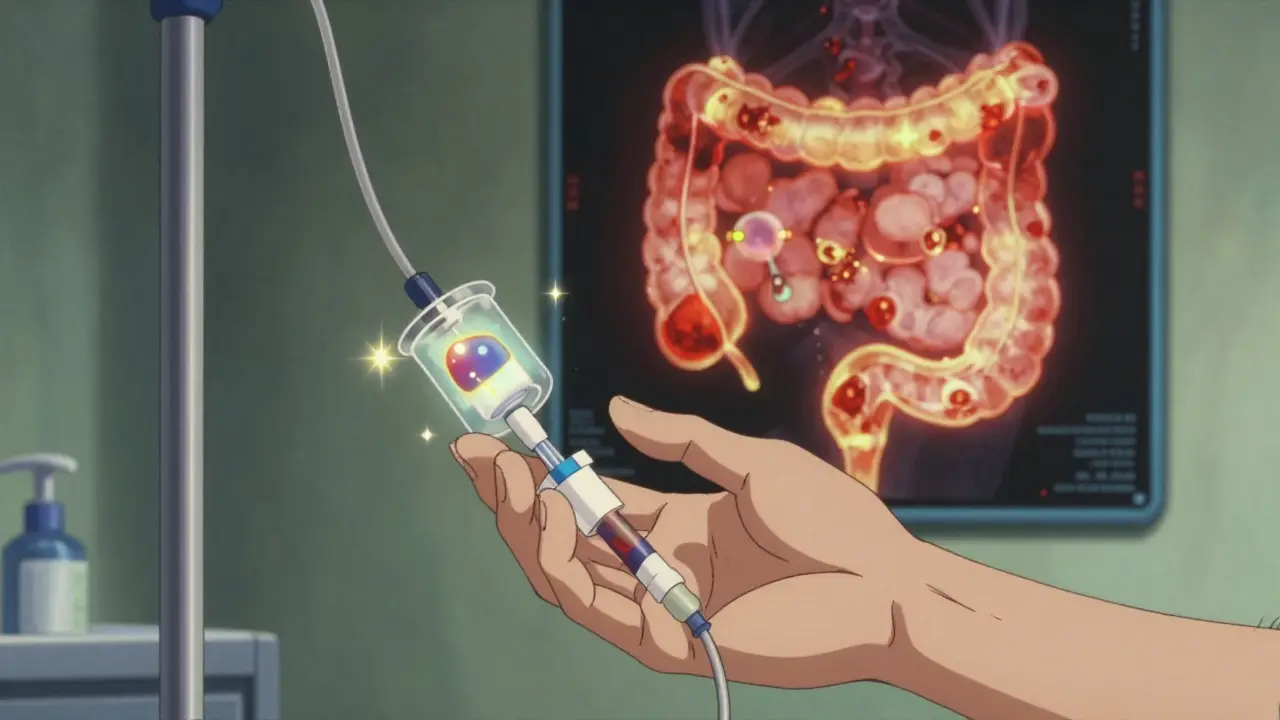
Don’t guess your levels. Get blood tests before and after starting supplements. Some people need IV iron or high-dose vitamin D injections if oral supplements aren’t working. One patient on Celiac.com reported chronic fatigue for over a year-even after going gluten-free-until an IV iron infusion fixed it.
Why You’re Still Sick After Going Gluten-Free
If you’ve been gluten-free for months and still feel awful, you’re not alone. About 30% of people with celiac disease continue to have symptoms despite following the diet. Why?- Hidden gluten: Cross-contamination in restaurants, shared toasters, or gluten in sauces and seasonings. One study found 85% of patients with ongoing symptoms had unintentional exposure.
- Leaky gut: The intestinal lining takes time to heal. Until then, inflammation and poor absorption continue.
- Other food intolerances: Many people develop lactose intolerance or SIBO (small intestinal bacterial overgrowth) after celiac damage.
- Supplements aren’t working: Poor-quality supplements, wrong forms (like oxide instead of citrate), or not taking them with food.
Dr. Alessio Fasano from Harvard says even 50 milligrams of gluten a day-about the size of a crumb-can stop your gut from healing in half of patients. That’s why you need a certified gluten-free dietitian. They’ll help you spot hidden sources: soy sauce, malt vinegar, communion wafers, spice blends, and even some cosmetics.
Testing, Tracking, and Follow-Up
Diagnosis starts with a blood test: tTG-IgA. It’s 98% accurate-if you’re still eating gluten. If you’ve already gone gluten-free, the test can be wrong. That’s why testing must happen before dietary changes. If the blood test is positive, an endoscopy with biopsy is usually needed to confirm damage (though new 2025 guidelines allow biopsy-free diagnosis in children with very high antibody levels).After diagnosis, track your progress:
- Month 1: Meet with a dietitian. Get baseline blood work (iron, B12, vitamin D, calcium, TSH).
- Month 3: Repeat CBC and metabolic panel. Check for improvement in anemia and nutrient levels.
- Month 6: Repeat tTG-IgA. Levels should drop by at least 50%. If not, you’re still being exposed to gluten.
- Year 1: Get a DXA scan to check bone density. Many people lose bone mass before diagnosis.
- Every 2-3 years: Repeat bone scan and nutrient panels.
Some patients need advanced testing like capsule endoscopy or stool tests for gut permeability if symptoms persist. The European Society for the Study of Coeliac Disease now recommends this for anyone still symptomatic after 2 years on a gluten-free diet.
Dining Out, Traveling, and Daily Life
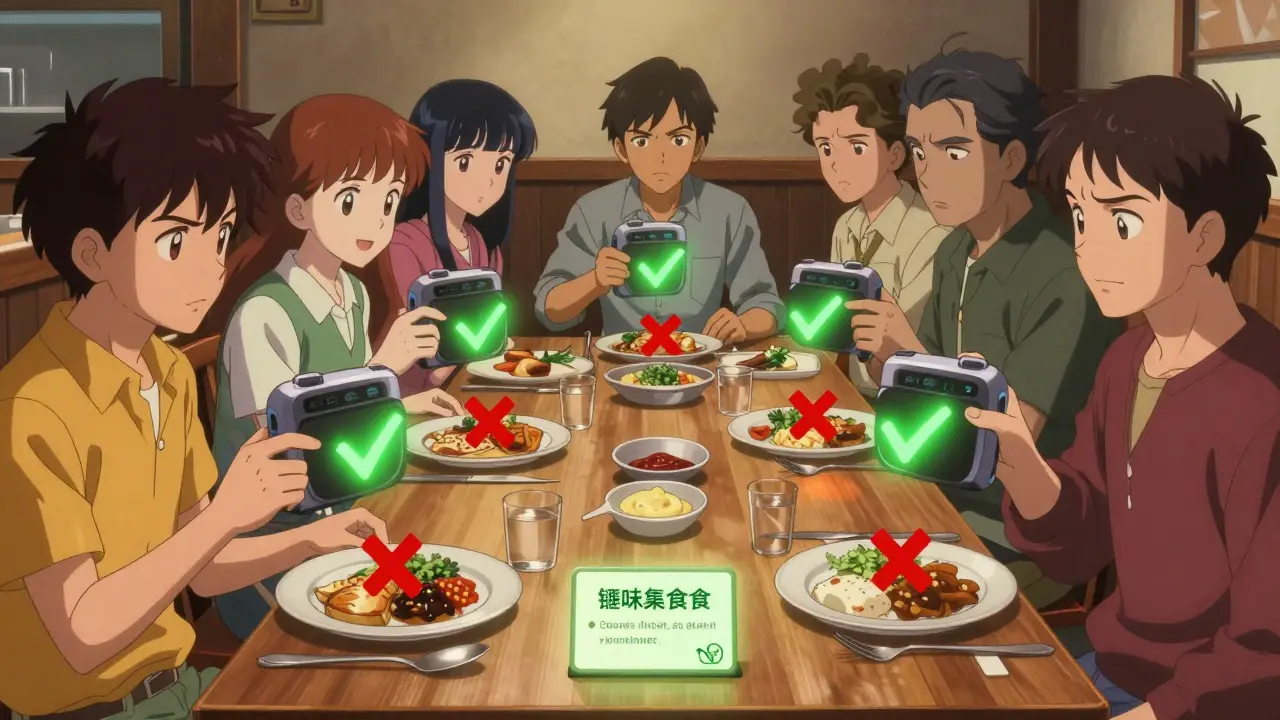
Only 28% of U.S. restaurants have verified gluten-free protocols, according to the National Restaurant Association. That means you can’t assume a “gluten-free menu” is safe. Ask these questions:- Do you have a separate grill, fryer, and prep area for gluten-free food?
- Are your utensils and cutting boards cleaned before preparing my meal?
- What brand of soy sauce do you use?
- Is the salad dressing gluten-free?
Carry a gluten-free dining card in 30+ languages from the Celiac Disease Foundation. It explains your needs clearly to kitchen staff. Use the Nima Sensor-a portable device that tests food for gluten in minutes. It detects levels as low as 20 ppm with 90% accuracy. It’s not perfect, but it’s better than guessing.
Medications are another blind spot. About 30% of prescriptions contain gluten as a filler. Check the Gluten-Free Drug Database from the University of Chicago. Always ask your pharmacist to verify.
The Cost and the Future
Gluten-free food costs 159% more than regular food. A loaf of gluten-free bread runs $5.99 per pound-nearly three times the price of regular bread. This isn’t just inconvenient-it’s a barrier to health. Many people skip supplements or eat lower-quality gluten-free products because they can’t afford the good ones.But things are changing. The global gluten-free market hit $8.37 billion in 2024 and is expected to grow to $12.34 billion by 2029. More grocery stores have dedicated gluten-free sections. Manufacturers are improving taste and texture. Still, insurance rarely covers the cost of supplements or dietitian visits. Only 15-20% of functional medicine testing is reimbursed.
Looking ahead, new tools are emerging: enzyme therapies like Latiglutenase (in Phase 3 trials) that break down gluten in the stomach, and gluten-detection sensors that fit in your phone. A vaccine called Nexvax2 is being tested, but early results were disappointing. For now, the only proven cure is still a strict, lifelong gluten-free diet.
Studies show that people who stick to the diet have a near-normal life expectancy. Those who don’t have 2.5 times the risk of early death from complications like intestinal lymphoma or osteoporosis fractures. It’s not about perfection-it’s about consistency. Every meal matters.
Can I eat oats if I have celiac disease?
Yes-but only certified gluten-free oats, and only after your gut has healed. Start with 50 grams per day and watch for symptoms. About 5% of people react to oats, even if they’re certified. If you get bloated, tired, or have diarrhea, stop eating them. Never eat regular oats-they’re almost always cross-contaminated.
Why am I still anemic after going gluten-free?
Your gut may still be healing, or your iron supplement isn’t being absorbed. Many people need higher doses or IV iron. Check your ferritin levels-not just hemoglobin. Low ferritin means your body’s iron stores are empty, even if your blood looks okay. Take iron with vitamin C and avoid calcium or tea around the same time, as they block absorption.
Do I need to take supplements forever?
Not forever-but until your blood tests show normal levels. Most people need supplements for 6-18 months. After that, you may be able to get nutrients from food. But many continue taking vitamin D and magnesium long-term because it’s hard to get enough from diet alone, even on a gluten-free plan.
Can celiac disease be cured?
No, not yet. The only proven treatment is lifelong gluten avoidance. Researchers are testing enzyme therapies and vaccines, but nothing is approved yet. Even if a cure comes, it won’t replace the need for a gluten-free diet until it’s proven safe and effective for everyone.
How do I know if my gluten-free diet is working?
Symptoms should improve within weeks. Blood tests (tTG-IgA) should drop by at least half within 6 months. Bone density should start improving in 1-2 years. If you’re still tired, bloated, or getting sick after 6 months, you’re likely still getting gluten. Talk to a dietitian and get retested.
What to Do Next
If you’ve just been diagnosed:- Book a consultation with a certified gluten-free dietitian (find one through the Academy of Nutrition and Dietetics).
- Get blood tests for iron, vitamin D, calcium, B12, folate, and thyroid function.
- Start supplements based on your results-not what you read online.
- Buy a dedicated toaster and separate cutting boards for gluten-free food.
- Download the Nima Sensor or carry a dining card when eating out.
- Check all medications with the Gluten-Free Drug Database.
If you’ve been gluten-free for a while but still feel off:
- Re-test your tTG-IgA and nutrient levels.
- Review every meal for hidden gluten-spices, sauces, supplements, lip balm.
- Ask your doctor about SIBO or lactose intolerance testing.
- Consider a capsule endoscopy if symptoms persist after 2 years.
Celiac disease isn’t a phase. It’s a lifelong condition that demands attention-but with the right plan, you can thrive. Your body has already shown it can heal. Now, give it the nutrients it needs to stay strong.


Catherine Scutt
January 10, 2026 AT 15:12Okay but have you tried gluten-free oats? I ate them for two weeks straight and felt like a zombie. Turned out I’m one of the 5%. No one talks about that. Just sayin’.
Darren McGuff
January 11, 2026 AT 05:36Oh my god, I cried reading this. I was diagnosed 3 years ago and spent 14 months feeling like my bones were made of wet cardboard. Then I found out my vitamin D was at 12 ng/mL. Took 5,000 IU daily + sunlight like it was my job. Now I hike in winter. Your body remembers how to heal-you just gotta give it the right tools. 💪
Alicia Hasö
January 12, 2026 AT 13:22To everyone new to this journey: you are not broken. You are not failing. You are a warrior rebuilding your biology one gluten-free meal at a time. The fatigue? The brain fog? The anxiety? They’re not in your head-they’re in your gut. And guess what? Science says it heals. You don’t need to be perfect. You just need to be consistent. Start with the blood tests. Get the right supplements. Find your dietitian. You’ve already taken the hardest step-you’re here. Now let’s build your strength, one nutrient at a time. 🌱
Aron Veldhuizen
January 14, 2026 AT 06:55Let’s be intellectually honest here: the entire gluten-free industry is a $12 billion scam built on placebo effects and corporate greed. You’re told you need expensive supplements, special toasters, and $8 loaves of bread-when the real solution is just eating whole foods. Potatoes. Chicken. Lettuce. No one needs a Nima Sensor to survive. This isn’t medicine-it’s marketing dressed up as science. And yes, I’ve read the studies. The mortality risk is overstated. You’re being manipulated.
Ian Long
January 14, 2026 AT 21:56I get where Aron’s coming from-but I also spent 8 months in the ER with unexplained anemia and nerve damage because I believed him. I cut out everything ‘gluten-adjacent’ and still felt awful. Then I got my ferritin checked-it was 4. IV iron changed my life. The science is real. The supplements? Necessary. The cost? Brutal. But if you’re still alive to read this, you owe it to yourself to do the testing. Don’t let ideology override your health.
Elisha Muwanga
January 14, 2026 AT 22:39Why are we letting corporations profit off a medical condition? In my country, we just eat rice and meat. No fancy supplements. No $200 sensors. No dietitians. You want to live? Stop eating wheat. That’s it. This whole ‘gluten-free lifestyle’ is just American over-medicalization. We’re turning a simple intolerance into a cult. Get over it.
Maggie Noe
January 16, 2026 AT 11:42Just got my tTG-IgA back-down 80% in 6 months. Still taking magnesium glycinate. Still avoiding soy sauce like it’s poison. Still using my Nima. Still terrified of restaurant kitchens. But I’m sleeping. I’m smiling. I’m alive. 🙏✨
Heather Wilson
January 18, 2026 AT 07:22Let’s address the elephant in the room: the 30% of people who remain symptomatic despite strict adherence. The article implies this is due to hidden gluten-but what if it’s not? What if the autoimmune response persists independently? What if the gut never fully heals? What if this is a chronic immune dysregulation, not a dietary failure? The data is messy. We’re treating a symptom, not a root cause. And yet, no one wants to say that out loud.
Jeffrey Hu
January 18, 2026 AT 13:55Wait-you’re telling me I need to take 400mg of magnesium glycinate daily? I thought magnesium was just for leg cramps. And why not just eat spinach and almonds? Also, are you sure the FDA’s 20ppm standard is safe? I read a paper that said 5ppm is the real threshold for neural sensitivity. And what about the microbiome? Did you factor in that gluten-free diets reduce fiber intake? This whole thing feels like a checklist, not a science.