Every year in the U.S., over 1.3 million medication errors happen in hospitals and pharmacies. Many of these aren’t caused by careless staff-they’re the result of human limits. A pharmacist juggling 20 prescriptions at once, a tired technician reading tiny labels, a patient with a similar name to someone else on the floor. These aren’t rare mistakes. They’re predictable. And that’s why barcode scanning became the most reliable tool in modern pharmacy safety.
How Barcode Scanning Stops Errors Before They Happen
Barcode scanning in pharmacies isn’t just a tech upgrade. It’s a safety checkpoint built into the workflow. The system works by requiring two scans: one on the patient’s wristband and one on the medication’s barcode. If the system doesn’t match the right drug, dose, and patient, it won’t let the prescription go through. That’s called the five rights check: right patient, right medication, right dose, right route, right time. Before barcodes, pharmacists relied on double-checking by hand. Studies show that manual checks catch only about 36% of errors. Barcode systems catch 93.4%. That’s not a small improvement-it’s a game-changer. At one Pennsylvania hospital, accuracy jumped from 86.5% to 97% after they started scanning every medication. That means out of every 100 prescriptions, they went from missing 13 errors to missing just 3. The system doesn’t guess. It doesn’t hope. It verifies. If a nurse grabs the wrong pill bottle-say, levothyroxine instead of lorazepam-the scanner flags it immediately. In one real case, a 10x overdose of levothyroxine was caught because the barcode didn’t match the order. That’s not luck. That’s technology doing exactly what it was built for.The Technology Behind the Scan
Most pharmacy barcodes today are 1D linear codes that store the National Drug Code (NDC). That’s a unique 10- or 11-digit number assigned by the FDA to every medication. Since 2006, all unit-dose packages in the U.S. have been required to carry this barcode. But newer systems are moving to 2D matrix codes-like QR codes-that can hold more data: lot numbers, expiration dates, even manufacturer info. The hardware is simple: a handheld or mobile scanner connected to the pharmacy’s information system. These scanners need to read damaged, smudged, or partially covered barcodes. That’s not always easy. Ampules, insulin pens, and small vials often have tiny or poorly printed labels. Some pharmacies use special trays with built-in lighting to help scanners read these tricky packages. The real power comes from integration. The scanner doesn’t work alone. It talks to the electronic health record (EHR), the pharmacy information system (PIS), and sometimes automated dispensing cabinets. If the system sees that Patient A was prescribed 5mg of warfarin but the bottle says 10mg, it blocks the release. It also logs who scanned what, when, and where-creating a full audit trail for safety reviews.What It Can’t Fix
Barcode scanning isn’t magic. It can’t fix a label that’s wrong to begin with. If a pharmacy tech accidentally puts a 50mg label on a 5mg tablet-and the barcode matches that label-the system will approve it. That’s why the FDA and the Institute for Safe Medication Practices (ISMP) insist: always verify the medication visually before scanning. There are also workarounds. When scanners fail, staff sometimes bypass them. A 2024 survey found that 41% of pharmacists admitted to skipping scans during busy shifts. In emergency rooms, where seconds count, some nurses just grab the meds and move on. That’s dangerous. ECRI Institute’s 2024 alert says: “It is not safe to send a label by itself.” If the barcode won’t scan, you must look at the drug, check the name, strength, and form-and then decide if it’s correct. Another blind spot: compounded medications. If a pharmacy mixes a custom dose of morphine or a liquid antibiotic, there’s often no barcode. Those rely on manual checks. That’s why BCMA systems are strongest in hospitals with standardized, factory-packaged drugs-not in specialty pharmacies that make a lot of custom formulas.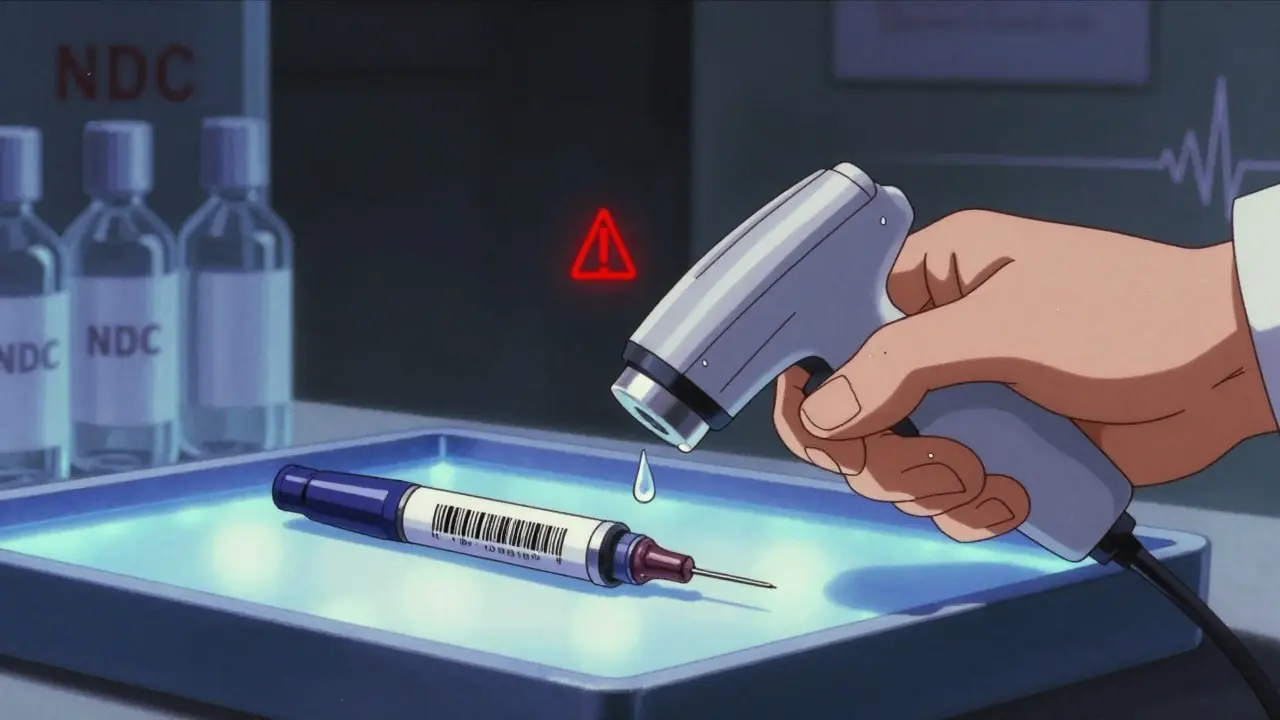
Why It’s Better Than Manual Checks
Think about how many times you’ve seen a pharmacist squint at a tiny label, compare it to a printout, then nod and move on. That’s human judgment under pressure. People get tired. They multitask. They assume. Barcode scanning removes the guesswork. It doesn’t care if you had a bad night’s sleep. It doesn’t get distracted by a ringing phone. It just matches numbers. And the data backs it up:- 89% reduction in wrong drug errors
- 86% reduction in wrong dose errors
- 92% reduction in wrong patient errors
Real Problems, Real Solutions
Barcodes aren’t perfect. Pharmacists complain about them every day. “It adds 15 to 20 minutes to my shift,” one tech wrote on Reddit. “We lose time scanning broken barcodes on insulin pens.” Another said their scanner freezes during rush hour. The solutions aren’t technical-they’re procedural. - Test new products before they hit the floor. If a new medication comes in with a barcode that’s too small or faded, don’t just accept it. Test it with your scanner. Report bad labels to the manufacturer. - Use special trays for small vials. Some pharmacies keep illuminated trays for ampules and insulin. These make scanning 70% faster and reduce errors. - Train staff on what to do when scanning fails. Too many staff just hit “skip.” That’s not a fix. They need a clear protocol: stop, visually verify, document the exception, and escalate if unsure. - Review scan data monthly. Which drugs are most often scanned late or skipped? That’s your red flag. Maybe it’s a high-risk med like insulin or heparin. Target those for extra checks. - Never trust the label alone. Even if the barcode matches, if the pill looks wrong-wrong color, wrong shape-stop. That’s your last line of defense.
Adoption and the Future
In U.S. hospitals, 78% now use barcode scanning. That’s up from 42% in 2015. But in community pharmacies? Only 35%. Why? Cost. Smaller pharmacies can’t afford the scanners, software, and training. But the risk is higher there too. One wrong pill can kill someone at home, not just in a hospital. The future is 2D barcodes. By 2026, 65% of medications will use them. That means more data, better traceability, and fewer scanning failures. Some companies are even testing AI that predicts when a barcode will fail before the scan even happens-suggesting a better angle or lighting. The technology won’t replace pharmacists. It will make them safer. The goal isn’t to automate the job-it’s to automate the mistakes. And right now, barcode scanning is the most proven way to do it.What You Should Know as a Patient
If you see a pharmacist scan your wristband and then scan your medication, don’t think it’s just bureaucracy. That’s the system protecting you. If you’re given a new pill and it looks different from your last refill, say something. Even if the barcode scanned fine, your eyes are still the final safety check. You’re not just a patient. You’re part of the safety team.How effective is barcode scanning at preventing medication errors?
Barcode scanning systems prevent 93.4% of potential dispensing errors when used correctly, according to a 2021 BMJ Quality & Safety study. This means out of every 100 mistakes that could happen, the system stops 93 of them. In real-world settings, hospitals have seen overall medication error rates drop by 65% to 86% after implementation.
Do all medications have barcodes?
Since 2006, the FDA has required all unit-dose packaged medications sold in the U.S. to carry a barcode with the National Drug Code (NDC). However, compounded medications, emergency medications, and some specialty drugs (like insulin pens or ampules) may not have barcodes or may have poorly printed ones. In these cases, visual verification by a pharmacist is required.
Can barcode scanning cause errors?
Yes-if used incorrectly. The biggest risk is automation bias: staff trusting the scanner over their own judgment. For example, if a label is printed wrong but the barcode matches it, the system will approve the error. That’s why pharmacists are trained to visually verify the medication even after a successful scan. Workarounds, like skipping scans during busy times, also reduce safety.
Why do some pharmacists dislike barcode systems?
Many report that scanning adds time to their shift, especially with damaged barcodes, small vials, or system glitches. Some scanners don’t read ampules well without special trays. Others say frequent false alerts cause "alert fatigue," making staff more likely to ignore warnings. Training gaps also play a role-staff who don’t know how to handle scan failures are more likely to bypass the system.
Is barcode scanning used in community pharmacies?
Less than 35% of community pharmacies in the U.S. use barcode scanning, mainly due to cost and lack of regulation. Most systems are installed in hospitals and large health systems. But as the technology becomes cheaper and more compact, adoption in retail settings is slowly increasing. The American Society of Health-System Pharmacists recommends it for all pharmacies, regardless of size.

Iona Jane
January 15, 2026 AT 17:31Barcodes are just the beginning. They’re tracking us. Every pill you take, every scan-it’s feeding a database that knows when you’re sick, what you’re taking, and who you are. This isn’t safety. It’s surveillance dressed in white coats.
Jami Reynolds
January 17, 2026 AT 14:16While the data presented is statistically compelling, it remains fundamentally flawed in its epistemological framing. The assumption that technological determinism can override human fallibility is a dangerous myth perpetuated by institutional orthodoxy. The five rights are not algorithmically enforceable-they are ethical imperatives requiring moral agency, which cannot be outsourced to a scanner.
Furthermore, the reliance on NDC codes ignores the structural corruption within pharmaceutical supply chains. Many barcodes are generated by third-party repackagers who mislabel medications. The system doesn’t prevent error-it automates misrepresentation.
The FDA’s mandate of 2006 was not a public health triumph but a corporate compromise. Manufacturers lobbied for the least intrusive standard possible. The barcode is a compliance theater, not a safety net.
And yet, the narrative persists: technology fixes everything. But when a nurse skips a scan during a shift change, is that negligence-or a rational response to a system designed to fail?
Consider this: if the system catches 93.4% of errors, what happens to the remaining 6.6%? Are they the most lethal ones? The ones that slip through because they involve off-label use, pediatric dosing, or polypharmacy? The data doesn’t say.
The real issue isn’t the scanner. It’s the institutional refusal to reduce workload, increase staffing, or invest in pharmacist education. We’ve outsourced responsibility to silicon, then punished humans when the silicon fails.
And let’s not forget: barcodes don’t prevent drug interactions. They don’t detect allergies. They don’t know if the patient is pregnant, fasting, or allergic to the dye in the pill.
The reduction in wrong-drug errors? Fine. But the rise in alert fatigue? Ignored. The erosion of clinical judgment? Celebrated as efficiency.
This isn’t progress. It’s the quiet surrender of professional autonomy to corporate efficiency metrics.
And yes-I’ve seen a barcode scan approve a 10x overdose because the label was printed wrong. The system didn’t catch it. The nurse did. Because she looked.
Technology is a tool. Not a guardian. Not a savior. Not a replacement for vigilance.
Sohan Jindal
January 19, 2026 AT 08:38This whole barcode thing is just another way for the feds to control us. They don’t care if you live or die-they care if they can track you. And now they’re forcing pharmacies to scan every pill like you’re some kind of criminal. Next thing you know, they’ll scan your coffee cup to see if you’re diabetic.
Ayush Pareek
January 20, 2026 AT 05:57I’ve seen this work in my hospital back in Mumbai. The system isn’t perfect, but it’s the best tool we’ve got. The real win? When a new tech learns to stop and look-instead of just scanning. That’s the culture shift. Not the machine.
Frank Geurts
January 20, 2026 AT 20:17It is with profound respect for the meticulous advancements in pharmaceutical safety infrastructure that I submit the following observation: the implementation of barcode-mediated clinical verification protocols constitutes not merely a procedural enhancement, but a paradigmatic evolution in the epistemology of pharmacological accountability. The integration of NDC-encoded data streams into EHR-PIS ecosystems represents a triumph of interdisciplinary systems engineering, wherein the confluence of regulatory compliance, human factors design, and data integrity yields an unprecedented reduction in iatrogenic harm. One must, however, acknowledge the persistent epistemic vulnerabilities inherent in automation bias-wherein the human operator, lulled by the illusion of algorithmic infallibility, relinquishes the sacred duty of visual corroboration. This is not a failure of technology, but a failure of training. And it is here that the moral imperative of professional stewardship must be reasserted, not revoked.
Nat Young
January 22, 2026 AT 04:4893.4%? That’s not impressive. That’s just better than guessing. You’re still missing 7% of errors. And those are the ones that kill people. So congrats-you turned a 64% failure rate into a 6.6% one. Still not good enough.
Also, why are we still using 1D barcodes in 2025? That’s like using a rotary phone because ‘it’s reliable.’
And don’t get me started on the 41% who skip scans. That’s not a glitch. That’s a revolt.
ellen adamina
January 22, 2026 AT 19:07I’ve been on both sides-patient and nurse. I saw a man almost get the wrong heart med because the barcode scanned fine but the pill was the wrong color. He didn’t say anything. I did. That’s the real safety net: someone who cares enough to look.
Niki Van den Bossche
January 24, 2026 AT 02:25Barcodes are the new religion. We’ve replaced prayer with scanning. We’ve replaced intuition with algorithms. We’ve replaced the pharmacist as a healer with a data-entry clerk who stares at a screen like a zombie. The soul of pharmacy is being digitized into oblivion-and we call it progress. How poetic. How tragic. How utterly, beautifully American.
Mike Berrange
January 24, 2026 AT 11:26So let me get this straight. You’re proud that a machine catches 93% of errors, but you ignore that the machine is only as good as the label it reads? And you think that’s a win? That’s like being proud your GPS works as long as the street signs aren’t painted over.
Also, why are we still using NDC? It’s a 10-digit mess. Why not use a universal product code? Or a blockchain? Or at least a QR code that doesn’t vanish when the pill bottle gets wet?
You’re not solving the problem. You’re just making it look like you are.
Diane Hendriks
January 24, 2026 AT 13:15The United States of America leads the world in pharmaceutical innovation-not because of government mandates, but because of private-sector ingenuity. The adoption of barcode scanning is a testament to American efficiency, discipline, and commitment to life. Other nations cling to outdated manual systems. We do not. We scan. We verify. We protect. And we do not apologize for it. The 6.6% of errors that remain? They are the cost of freedom. And we pay it with vigilance, not with surrender to bureaucracy.