When a brand-name drug’s patent runs out, the market doesn’t just open up to generic competitors-it gets messy. That’s when you see the rise of authorized generics: the same pill, same capsule, same inactive ingredients, but without the brand name on the label. These aren’t knockoffs. They’re made by the original company, often on the same production line, and sold at a lower price. And they’re one of the most strategic moves big pharma makes when their monopoly ends.
What Exactly Is an Authorized Generic?
An authorized generic is the exact same drug as the brand-name version-same active ingredient, same fillers, same coating, same everything. The only difference? It’s sold under a different label, usually by a subsidiary or partner of the original manufacturer. Think of it like a car company making the same model but selling it under a budget brand name. No changes. No shortcuts. Just a new box.
Unlike traditional generics, which must prove they’re bioequivalent through an Abbreviated New Drug Application (ANDA), authorized generics skip that step entirely. They’re marketed under the original New Drug Application (NDA) the brand company already got FDA approval for. That means no extra testing, no delays, and no uncertainty about whether they work the same way. The FDA confirms they’re therapeutically equivalent because they literally are the same product.
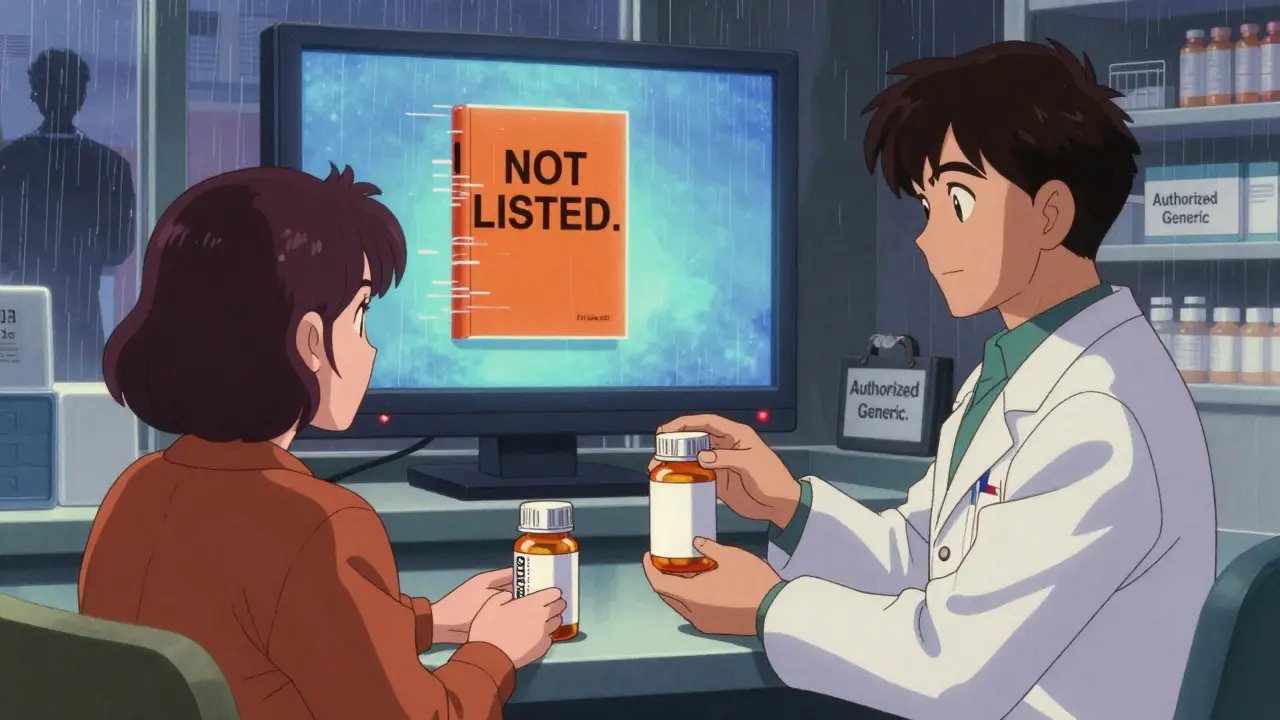
And here’s the twist: they’re not listed in the FDA’s Orange Book, the official directory of approved drug products. That’s because they’re not new applications-they’re just rebranded versions of the original. So if you’re a pharmacist checking for substitution rules, you won’t find them there. You have to know they exist.
Why Do Brand Companies Launch Them?
It’s not altruism. It’s business.
When a patent expires, the first generic manufacturer gets 180 days of exclusive market access under the Hatch-Waxman Act. That’s a huge window to capture market share before everyone else jumps in. But if the brand company sits back and waits, they lose everything. So instead, they launch their own generic version-right then, right there.
Studies show that between 2010 and 2019, there were 854 authorized generic launches in the U.S. Most of them hit the market before or during that 180-day exclusivity window. Why? To undercut the first generic and keep their revenue flowing. When a brand company launches its own generic, it forces the first generic to lower prices to compete. That drives down costs for consumers and insurers.
According to the Federal Trade Commission’s 2011 report, markets with authorized generics saw prices 15-20% lower during the exclusivity period than those without. That’s not a coincidence. It’s strategy. The brand company doesn’t just protect its profits-it reshapes the entire pricing landscape.
Authorized Generics vs. Traditional Generics: The Real Difference
People assume all generics are the same. They’re not.
Traditional generics only need to match the active ingredient. They can-and often do-use different fillers, dyes, or coatings. For most drugs, that’s fine. But for medications with a narrow therapeutic index-like blood thinners, seizure drugs, or thyroid hormone-those tiny differences matter. A patient stabilized on the brand might have a bad reaction to a generic with different inactive ingredients. That’s where authorized generics step in.
Because they’re chemically identical, they’re the closest thing to the original drug you can get. That’s why they’re especially common in CNS drugs like ADHD medications (Concerta’s authorized generic is methylphenidate ER) or antidepressants. Pharmacists report patients who failed on traditional generics but did perfectly fine on the authorized version.
But here’s the catch: patients don’t always know they’re getting the same thing. A 2023 review on Drugs.com showed people confused why their “generic” Singulair looked identical to the brand. Others thought they were being tricked. Pharmacy staff say 68% of their patients ask about the difference between authorized and traditional generics. The labeling doesn’t help-just the absence of the brand name. No “generic” label. No clear warning. Just a different box.
Who Benefits? And Who Gets Left Out?
On paper, everyone wins: consumers pay less, insurers save money, and patients get consistent medication. But the story gets complicated.
Brand companies benefit by keeping a foot in the door. Instead of losing 100% of sales when the patent expires, they keep 20-40% through their authorized generic. Some estimates suggest 42% of top-selling drugs facing patent expiry between 2015 and 2020 had authorized generics launched within six months.
But critics argue this delays true competition. If the first generic can’t capture the market because the brand is undercutting them with its own version, the broader wave of generic manufacturers may never enter. The Generic Pharmaceutical Association has warned this tactic fragments the market and reduces long-term price drops.
Meanwhile, the FDA and FTC agree: consumers win in the short term. Lower prices during the critical 180-day window mean real savings. But long-term? It’s unclear. The FTC is now studying whether recent trends have changed the 2011 findings. Preliminary data expected in early 2026 may show if this strategy is becoming more aggressive-or if regulators are stepping in.
How Pharmacies Handle Authorized Generics
Pharmacists are on the front lines of confusion.
Because authorized generics aren’t in the Orange Book, pharmacy systems don’t automatically flag them as interchangeable. Many still get coded as brand-name drugs in billing systems, causing insurance denials. A 2021 survey found 41% of independent pharmacies had billing errors tied to authorized generics.
Training is patchy. AmerisourceBergen’s 2022 data showed 73% of pharmacy technicians needed 2-3 weeks of extra training to identify and explain them correctly. Some manufacturers, like Greenstone Pharmaceuticals (Pfizer’s authorized generic arm), provide clear documentation. Others? Not so much. One 2022 review gave some smaller manufacturers a 2.8 out of 5 for clarity.
Pharmacy software is catching up. Epic Systems added a specific flag for authorized generics in its 2021 update, cutting identification errors by 67%. But not every pharmacy uses Epic. Many still rely on manual checks or outdated databases.
And then there’s the patient education problem. You can’t just say, “This is a generic.” You have to explain: “This is the exact same pill your doctor prescribed, just sold under a different name.” That takes time. And time is money in a busy pharmacy.

The Future: More Authorized Generics, or a Regulatory Crackdown?
The numbers tell a clear story: authorized generics are growing. The FDA’s updated list as of October 2025 includes 1,247 products-up from under 500 in 2015. Evaluate Pharma predicts 45% of major branded drugs will have authorized generics by 2027, up from 32% in 2022.
But pushback is coming. In 2023, Congress introduced the Promoting Competition in Pharmaceutical Markets Act, which would ban brand companies from launching authorized generics during the first generic’s 180-day exclusivity period. If passed, it would force them to choose: either let the market open fully, or keep the brand name and lose the generic revenue.
Some analysts think this is the beginning of the end. Bernstein Research predicts market saturation by 2027 as more generic manufacturers enter and brand companies lose the edge. Others, like Jefferies, see continued growth through 2030, especially in complex drug categories where consistency matters most.
One thing’s certain: as more drugs lose patent protection-especially high-revenue ones like biologics and specialty medications-authorized generics will keep being used. They’re not a loophole. They’re a tool. And for now, the companies that make them are using it well.
What Patients Should Know
If you’re on a brand-name drug and your prescription suddenly changes to a different-looking pill, don’t panic. Ask your pharmacist: “Is this an authorized generic?”
If yes, you’re getting the same medicine. No risk. No compromise. Just lower cost.
And if your insurance switches you to a traditional generic and you feel off-fatigued, dizzy, or your condition isn’t controlled-ask about the authorized version. For some drugs, it’s the only generic that won’t throw you off balance.
Don’t assume all generics are equal. Know what you’re getting. And if your pharmacist doesn’t know the difference, ask them to check. It’s your health.
Are authorized generics the same as the brand-name drug?
Yes. Authorized generics contain the exact same active and inactive ingredients as the brand-name drug. They’re made on the same production line, often by the same company, and are therapeutically identical. The only difference is the label-no brand name, no marketing.
Why aren’t authorized generics listed in the FDA’s Orange Book?
Because they’re not new drug applications. Authorized generics are marketed under the original brand’s New Drug Application (NDA), so they don’t need separate FDA approval. The Orange Book only lists drugs approved through ANDA or NDA submissions as distinct products. Since authorized generics are just re-labeled versions of the brand, they’re excluded.
Do authorized generics cost less than traditional generics?
Usually, yes-but not always. Authorized generics often cost less than the brand name and sometimes less than traditional generics, especially during the first 180 days after patent expiry. However, prices vary by insurer, pharmacy, and region. In some cases, traditional generics may be cheaper if multiple manufacturers are competing.
Can I ask my pharmacist for an authorized generic?
Absolutely. You have the right to request it. If your insurance covers it and the pharmacy stocks it, they can fill your prescription with the authorized version. Just say: “Is there an authorized generic for this drug?” and ask them to check the label or database.
Why do some patients do worse on traditional generics but fine on authorized generics?
Because traditional generics can have different inactive ingredients-fillers, dyes, binders-that affect how the drug is absorbed. For drugs with a narrow therapeutic index, even small changes can impact effectiveness or cause side effects. Authorized generics eliminate this risk because they’re chemically identical to the brand.
Is it legal for brand companies to launch their own generic?
Yes. It’s fully legal under U.S. drug laws. The Hatch-Waxman Act allows brand manufacturers to market authorized generics, and the FDA permits it under the original NDA. While controversial, it’s a recognized part of the market structure-not a loophole or violation.