When your heart skips, races, or flutters out of rhythm, it’s not just annoying-it can be dangerous. Arrhythmias like atrial fibrillation (AF) affect over 33 million people worldwide, and for many, pills alone don’t cut it. That’s where catheter ablation and device therapy come in. These aren’t just last-resort options anymore. For the right patients, they can mean the difference between living with constant anxiety about your next heartbeat-or getting back to normal life.
What Is Catheter Ablation, Really?
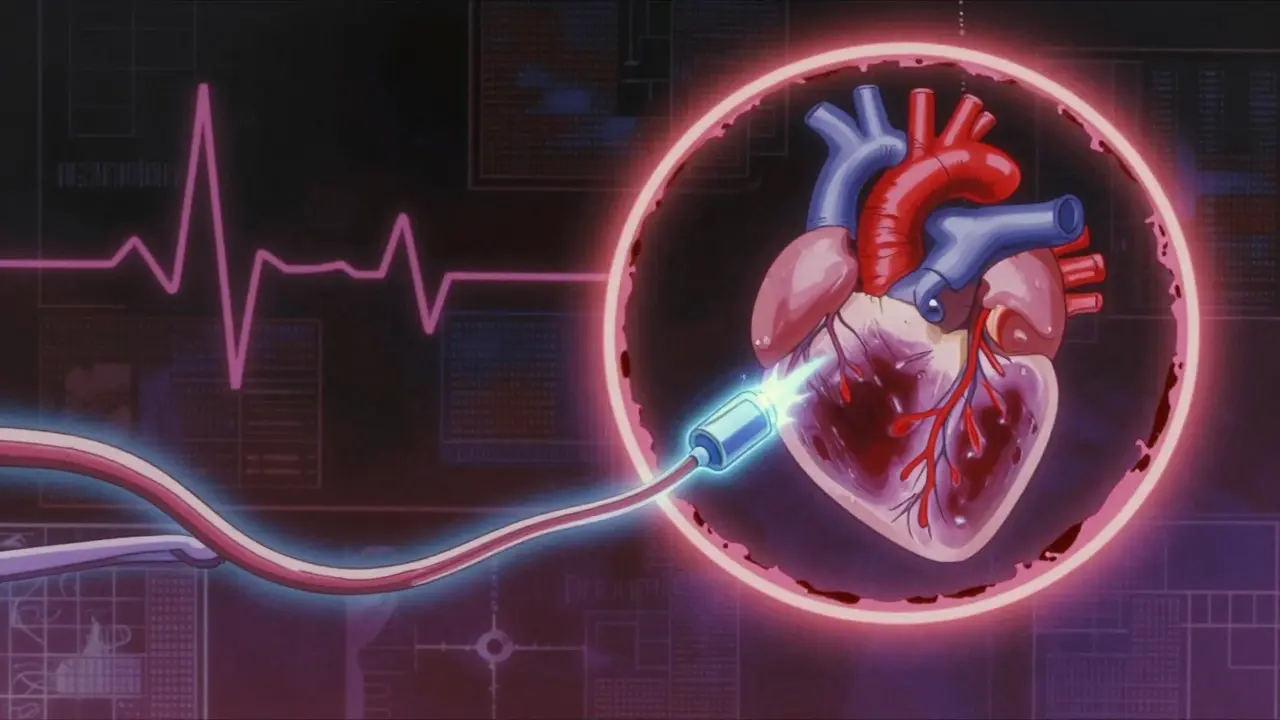
Catheter ablation is a minimally invasive procedure where thin, flexible tubes (catheters) are threaded through a vein in your groin or neck and guided into your heart. Once in place, the tip of the catheter delivers energy-either heat (radiofrequency) or cold (cryoablation)-to destroy tiny areas of heart tissue that are causing the abnormal rhythm. It’s not surgery. No big cuts. No open chest. Most people go home the same day or the next. But don’t let that fool you. This is precision medicine. The goal? To create small, controlled scars in the heart that block the faulty electrical signals. Think of it like rerouting a short-circuit in your home’s wiring-except you’re doing it inside a beating heart. The most common target? The pulmonary veins. In atrial fibrillation, erratic signals often start there. So doctors use a technique called pulmonary vein isolation (PVI). They circle each vein with a ring of scar tissue, effectively isolating it from the rest of the heart. This stops the chaos before it spreads.Radiofrequency vs. Cryoablation: Which One’s Better?
There are two main types of energy used in ablation, and each has pros and cons. Radiofrequency ablation uses heat. It’s been around since the late 1980s and is the most common method. Modern catheters like the THERMOCOOL SMARTTOOTH a contact-sensing radiofrequency catheter developed by Biosense Webster don’t just zap tissue-they measure how firmly they’re touching the heart wall. This is huge. If the catheter isn’t pressing hard enough, the scar won’t stick. And if the scar doesn’t stick, the arrhythmia comes back. Studies show these smart catheters improve success rates by 12-15% and cut procedure time by about 25 minutes. They also reduce complications like heart perforation by 30-40%. The secret? A metric called the Ablation Index (AI). It combines pressure, power, and time into one number. If the AI hits the target, the scar is likely permanent. Cryoablation uses extreme cold. The Arctic Front Advance a cryoballoon system by Medtronic freezes the tissue in one go. Instead of moving a catheter around point by point, the balloon inflates and freezes the entire area around the pulmonary vein. It’s faster-usually 90 to 120 minutes-and has a shorter learning curve for doctors. But it carries a small risk of injuring the phrenic nerve, which controls the diaphragm. That’s why doctors monitor it with pacing during the procedure.Device Therapy: Pacemakers and ICDs for When Ablation Isn’t Enough
Not all arrhythmias are fixed by ablation. Some patients have slow heart rates (bradycardia) or dangerous fast rhythms that could cause sudden death. That’s where devices come in. Pacemakers are small implants that send electrical pulses to keep your heart beating regularly. They’re often used after ablation if the heart’s natural rhythm becomes too slow. Modern pacemakers can adjust your heart rate based on activity-so you don’t feel winded walking up stairs. Implantable cardioverter defibrillators (ICDs) are for higher-risk patients. These devices don’t just pace-they shock. If your heart goes into a life-threatening rhythm like ventricular tachycardia, the ICD delivers a jolt to reset it. They’re lifesavers for people with heart failure or a history of cardiac arrest. For some, ablation and device therapy go hand in hand. A patient might get an ablation to stop AF, then get an ICD to protect against sudden arrhythmias caused by underlying heart damage. It’s not one or the other-it’s layered care.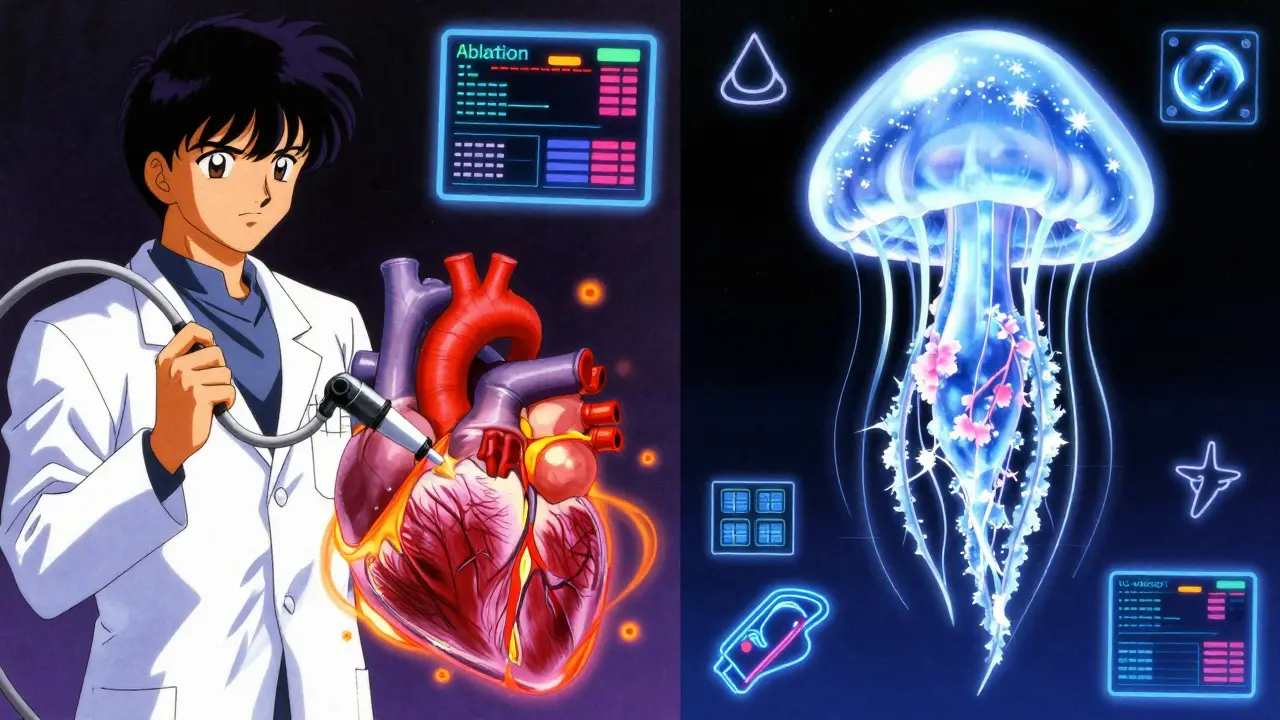
Why This Works Better Than Just Taking Pills
For years, doctors treated atrial fibrillation with antiarrhythmic drugs. But those meds come with side effects: dizziness, lung damage, even worsening arrhythmias. And they often fail. A 2020 meta-analysis of nearly 1,800 patients showed catheter ablation reduced AF recurrence by 58% compared to drugs. It also cut hospital visits for heart problems by 44%. But the biggest win? Survival. For patients with heart failure and reduced pumping ability (HFrEF), ablation slashed mortality by 48%. One study found these patients improved their heart’s pumping strength by over 5%-a massive jump for someone whose heart is already struggling. They walked farther, felt less tired, and lived longer. And it’s not just physical. A 2023 JAMA study found patients who had ablation reported less anxiety, fewer panic attacks, and better sleep. Why? Because they stopped living in fear of the next flutter. One Reddit user put it simply: “After my second ablation, I went from daily palpitations to zero episodes in nine months. The mental relief? Priceless.”What About the Risks?
No procedure is risk-free. About 8% of patients experience a major complication. The most serious? Cardiac tamponade-when blood leaks into the sac around the heart. It happens in about 1.2% of cases and needs immediate drainage. Other risks include damage to blood vessels, stroke (rare, less than 0.5%), and esophageal injury (especially with radiofrequency near the back of the heart). Cryoablation can affect the phrenic nerve, leading to temporary hiccups or breathing trouble. But here’s the thing: complications have dropped sharply since contact-sensing catheters became standard. And centers with high procedure volumes-those doing over 100 ablations a year-have complication rates nearly half those of low-volume centers.Who Gets This Treatment?
Guidelines from the European Society of Cardiology say catheter ablation should be offered as a first-line option for people with symptomatic paroxysmal AF who’ve tried at least one drug and still have symptoms. For persistent AF, it’s still a strong option if drugs aren’t working. It’s not for everyone. If your heart is severely damaged or you have other serious illnesses, the risks may outweigh the benefits. But if you’re otherwise healthy and tired of feeling like your heart is betraying you, ablation could be the reset button you need.
Cost, Access, and the Future
In the U.S., an ablation costs between $16,000 and $21,000 upfront. That sounds steep. But over time, it pays for itself. Patients need fewer hospital visits, less medication, and miss less work. Studies show ablation becomes cost-effective after just 3 to 8 years. The global market for these devices is booming-projected to hit $6.2 billion by 2028. Companies like Biosense Webster, Medtronic, and Abbott are racing to improve tech. The newest frontier? Pulsed Field Ablation (PFA) a non-thermal technique using electric pulses to destroy tissue. Approved by the FDA in 2023, PFA works faster-under 80 minutes-and doesn’t damage nearby structures like the esophagus. Early results show 86% freedom from AF at one year. AI is coming too. Soon, software will analyze the heart’s electrical map in real time and suggest where to ablate. This could make procedures even more precise-and maybe even available in smaller hospitals.What Happens After the Procedure?
You’ll need to rest for a few days. Avoid heavy lifting for a week. Some people feel chest discomfort or irregular beats for a few weeks-that’s normal. The heart is healing. Most patients stop antiarrhythmic drugs after 3 months if the rhythm stays stable. Follow-up is key: you’ll have ECGs, Holter monitors, and possibly a repeat ablation if the arrhythmia returns. Success rates after one procedure are about 70-80%. After a second ablation, they jump to over 90%. The goal isn’t just to stop the arrhythmia. It’s to give you back your life. To sleep through the night. To climb stairs without stopping. To stop checking your pulse every five minutes.Final Thoughts
Catheter ablation and device therapy aren’t just medical procedures-they’re turning points. For thousands, they’ve replaced fear with freedom. The tech is better than ever. The evidence is clear. And the people who’ve been through it? They’re living proof. If you’ve been told you need to live with your arrhythmia, ask if ablation is right for you. It might be the most important decision you make this year.Is catheter ablation considered surgery?
No, catheter ablation is not open-heart surgery. It’s a minimally invasive procedure where thin tubes (catheters) are inserted through a vein in the groin or neck and guided to the heart. No incisions are made in the chest. Patients usually go home within 24 hours.
How successful is catheter ablation for atrial fibrillation?
Success rates vary by type of AF. For paroxysmal AF (episodes that come and go), one ablation has about a 70-80% success rate at one year. For persistent AF (longer-lasting episodes), the rate is around 60-70%. A second procedure can boost success to over 90%. Contact-sensing catheters and the Ablation Index improve outcomes by 12-15% compared to older methods.
Can I stop taking blood thinners after ablation?
Not automatically. Even if your rhythm is normal, you may still need blood thinners for several months-or longer-because AF can leave behind electrical "remnants" that increase stroke risk. Your doctor will assess your stroke risk using tools like CHA₂DS₂-VASc and decide when it’s safe to stop.
What’s the difference between a pacemaker and an ICD?
A pacemaker helps if your heart beats too slowly by sending small electrical pulses to keep it going. An ICD does that too, but it can also deliver a strong shock if your heart goes into a dangerous fast rhythm like ventricular tachycardia or fibrillation. ICDs are for people at risk of sudden cardiac arrest.
How long does recovery take after catheter ablation?
Most people return to light activities within 2-3 days. Avoid heavy lifting or strenuous exercise for about a week. Some feel tired or have mild chest discomfort for up to two weeks. Irregular heartbeats in the first few weeks are normal as the heart heals. Full recovery and rhythm stabilization can take up to three months.
Are there alternatives to catheter ablation for arrhythmias?
Yes. Medications like beta-blockers or antiarrhythmic drugs are the first line. For some, cardioversion-an electric shock to reset the rhythm-is used temporarily. But if drugs fail or cause side effects, ablation is the next best option. For slow rhythms, a pacemaker may be needed. Device therapy and ablation are often used together, not as alternatives.
Is pulsed field ablation available now?
Yes. The Farapulse PFA system received FDA approval in September 2023 and is now being used in major U.S. and European centers. It uses short bursts of electric pulses instead of heat or cold, making it faster and safer for nearby tissues. Early results show 86% freedom from AF at one year with no reported esophageal injuries.

Jason Silva
December 23, 2025 AT 06:51mukesh matav
December 23, 2025 AT 23:03Peggy Adams
December 24, 2025 AT 13:39Christina Weber
December 25, 2025 AT 20:47Cara C
December 26, 2025 AT 11:23Dan Adkins
December 27, 2025 AT 23:01Meina Taiwo
December 28, 2025 AT 16:56Adrian Thompson
December 29, 2025 AT 14:13Southern NH Pagan Pride
December 30, 2025 AT 04:04Orlando Marquez Jr
December 31, 2025 AT 08:52