Drug Interaction Checker
Check Your Medication Safety
Acid-reducing medications like omeprazole or famotidine can reduce the effectiveness of certain drugs by up to 95%. Enter your medication to check for potential interactions.
Most people think of acid-reducing medications like omeprazole or famotidine as harmless fixes for heartburn. But what if taking one of these pills could make your blood pressure medicine, HIV treatment, or cancer drug stop working? That’s not a hypothetical. It’s happening right now - and many doctors and patients don’t even know it.
Proton pump inhibitors (PPIs) and H2 receptor antagonists (H2RAs) work by turning down stomach acid. That’s great if you have GERD or an ulcer. But your stomach isn’t just a digestion machine - it’s the first stop for most oral drugs. And when you change the pH there, you change how those drugs get into your bloodstream. The science is clear: acid-reducing medications can cut the absorption of certain drugs by up to 95%.
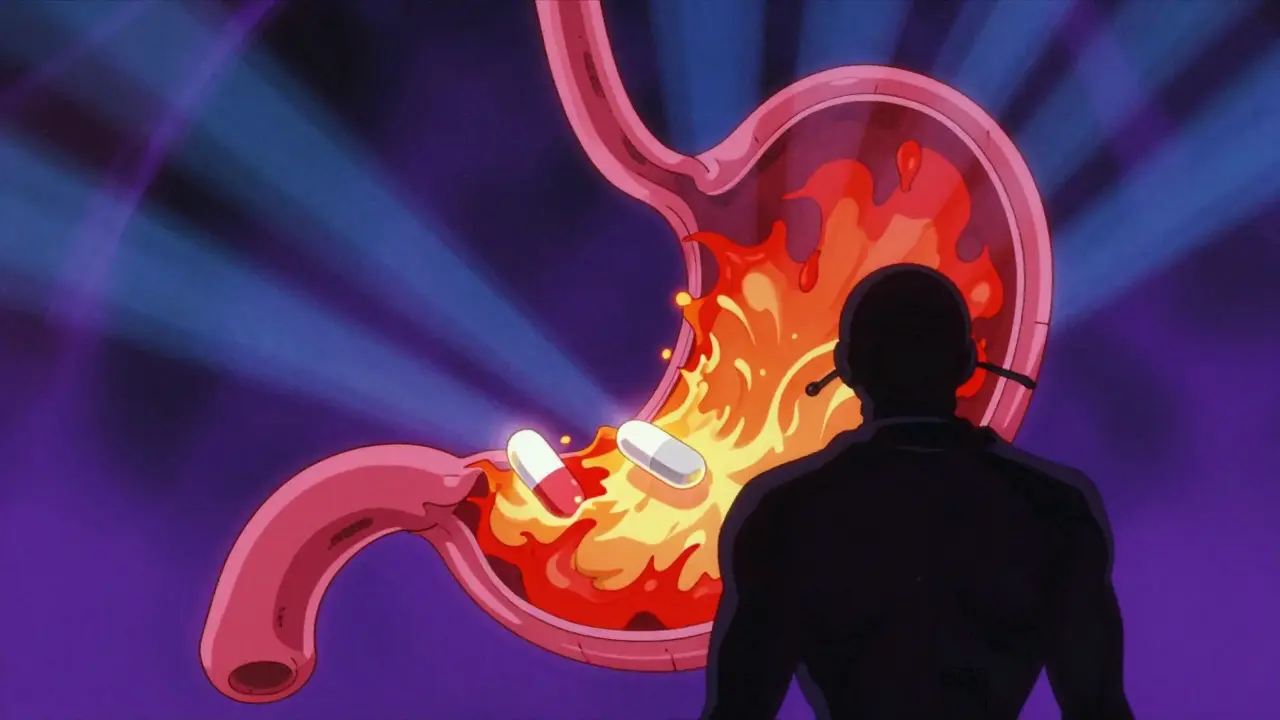
How Stomach Acid Affects Drug Absorption
Drugs aren’t all absorbed the same way. Most pills need to dissolve before they can be absorbed, and how well they dissolve depends on pH. The stomach normally has a pH between 1 and 3.5 - super acidic. That’s perfect for some drugs, terrible for others.
Weakly basic drugs - those with a pKa above 7 - need acid to dissolve. In a low-pH environment, they become charged and soluble. But when you take a PPI or H2RA, your stomach pH jumps to 4 or higher. Suddenly, these drugs stay neutral and don’t dissolve well. They just sit there, pass through, and get excreted. No absorption. No effect.
It’s not just about the stomach. About 90% of drug absorption happens in the small intestine, where pH is neutral to slightly alkaline. But here’s the catch: if a drug doesn’t dissolve in the stomach, it doesn’t get a chance to start moving into the intestine properly. Think of it like a pill that never breaks open - it just travels through your gut intact.
The Top Drugs That Get Knocked Out by Acid Reducers
Not all drugs are affected equally. The FDA and clinical studies have identified a shortlist of high-risk medications that lose effectiveness when taken with acid reducers. These aren’t rare or obscure - they’re commonly prescribed.
- Atazanavir (HIV treatment): AUC drops by 74-95% with PPIs. The prescribing label says do not use together. Yet, many patients take both because their doctor didn’t know.
- Dasatinib (leukemia drug): Absorption drops by 60%. Studies show patients on PPIs have 37% higher treatment failure rates.
- Ketoconazole (antifungal): Absorption falls by 75%. It’s so bad that this drug is often useless when paired with a PPI.
- Dasiglucagon (for low blood sugar): The opposite effect - absorption increases slightly. But even here, the change is small enough that dosing rarely needs adjustment.
These aren’t edge cases. Between 2020 and 2023, the FDA received over 1,200 reports of therapeutic failure linked to acid-reducing meds. Atazanavir alone accounted for over 300 of them. One Reddit user wrote: “My viral load went from undetectable to 12,000 after starting Prilosec.” That’s not anecdotal - it’s a textbook interaction.
PPIs vs. H2RAs: Not All Acid Reducers Are Equal
Many assume that all acid reducers work the same. They don’t. PPIs like omeprazole, esomeprazole, and pantoprazole are far more disruptive than H2RAs like famotidine or ranitidine.
PPIs shut down acid production for 14-18 hours a day. They’re designed to be long-lasting. That’s why they’re so effective for chronic GERD. But it also means they keep the stomach pH high for hours - long enough to wreck the absorption of drugs taken during that window.
H2RAs? They only last 8-12 hours. Their effect is weaker and shorter. Studies show they reduce absorption of weak-base drugs by 20-40%, compared to 40-80% for PPIs. So if you absolutely need an acid reducer and are on a high-risk drug, famotidine might be a safer choice - if timed right.
And it’s not just about strength. Immediate-release tablets are more vulnerable than extended-release versions. Enteric-coated pills? They’re supposed to dissolve in the intestine. But if the stomach is too alkaline, they can dissolve too early - and get destroyed by acid before they even reach their target.
Real-World Consequences: What Happens When Drugs Don’t Work
Imagine you’re on dasatinib for chronic myeloid leukemia. You take it daily. Your numbers are stable. Then you start omeprazole for acid reflux. Two weeks later, your white blood cell count spikes. Your oncologist says, “Something’s off.” You didn’t miss a dose. You didn’t change your diet. But your drug didn’t get absorbed.
That’s not rare. A 2023 study of over 12,000 patients found that those on PPIs with dasatinib had significantly higher rates of treatment failure. The same pattern shows up with HIV drugs. Patients who didn’t know about the interaction experienced viral rebound - meaning the virus came back, and they risked developing resistance.
And it’s not just life-threatening drugs. One Drugs.com user wrote: “My doctor didn’t tell me Nexium would interfere with my blood pressure meds - my readings were consistently 20 points higher until we figured out the interaction.”
These aren’t isolated stories. The American College of Gastroenterology estimates that 15,000-20,000 therapeutic failures each year in the U.S. are directly tied to inappropriate PPI use. That’s preventable harm.
What Can You Do? Practical Steps to Stay Safe
Don’t stop your acid reducer without talking to your doctor. But do ask these questions:
- Is my medication a weak base? (Ask your pharmacist - they can check the pKa.)
- Is there a safer alternative to my acid reducer? (Famotidine may be better than omeprazole.)
- Can I space them out? (Take the drug 2 hours before the acid reducer.)
- Is there a non-PPI option for my heartburn? (Antacids like Tums can be used 2-4 hours apart, but they don’t last long.)
- Am I even supposed to be on this PPI long-term? (About half of long-term users have no clear medical need.)
Staggering doses helps - but only a little. Tan et al. (2024) found that spacing a weak-base drug 2 hours before a PPI reduces the interaction by only 30-40%. It’s not a fix - just a partial workaround.
Pharmacists are your best allies. A 2023 study showed that when pharmacists reviewed prescriptions, they cut inappropriate ARA co-prescribing by 62% in Medicare patients. If your pharmacist flags a possible interaction, listen.
Electronic health records now warn doctors about these combinations. Epic Systems reports 78% of clinicians follow those alerts. But if your doctor didn’t get the alert - maybe because your meds were prescribed by someone else - you’re still at risk.
The Bigger Picture: Why This Keeps Happening
The global market for acid-reducing meds hit $18.7 billion in 2023. PPIs make up two-thirds of those prescriptions. But the CDC says 15% of adults in developed countries take them long-term - often without a diagnosis. Many take them for “just a little heartburn,” not realizing they’re risking their other meds.
The FDA has responded. Between 2020 and 2023, they required 28 drug labels to add warnings about acid-reducing interactions - up from just 12 in the prior five years. New drugs in development are being designed to avoid pH-dependent absorption. Some are using coatings that only dissolve at specific pH levels, or delivery systems that bypass the stomach entirely.
But until those innovations become standard, the risk remains. The American Gastroenterological Association predicts that by 2027, better clinical decision tools and provider education could reduce inappropriate PPI use by 25%. That could prevent 5,000-7,000 cases of therapeutic failure each year.
The bottom line? Acid-reducing meds aren’t harmless. They’re powerful tools - and like any powerful tool, they can break things if used carelessly. If you’re on one of these drugs and taking another medication, don’t assume it’s fine. Ask. Check. Double-check. Your life might depend on it.
Can I take antacids like Tums with my PPI?
Yes, but timing matters. Antacids work fast and fade fast - usually within 1-2 hours. If you need to take both, space them at least 2-4 hours apart. This avoids the pH spike that can interfere with absorption of other drugs. But antacids aren’t a long-term replacement for PPIs. They’re meant for occasional use.
Does famotidine (Zantac) have fewer interactions than omeprazole?
Yes. Famotidine raises stomach pH less and for a shorter time than PPIs. Studies show it reduces drug absorption by 20-40%, while PPIs cut it by 40-80%. If you must use an acid reducer while taking a high-risk drug like dasatinib or atazanavir, famotidine is the safer choice - but still not risk-free. Always check with your pharmacist.
I’m on atazanavir. Can I ever take a PPI?
No. The prescribing information for atazanavir explicitly says to avoid PPIs entirely. Even a single dose can drop drug levels by over 70%, risking HIV resistance. If you need acid control, talk to your infectious disease specialist. Alternatives like H2RAs or lifestyle changes (eating smaller meals, avoiding late-night food) may help. Never switch on your own.
Why don’t doctors always catch these interactions?
Many doctors don’t realize how common and dangerous these interactions are. A 2023 study found that over 60% of primary care providers couldn’t correctly identify high-risk drug pairs. Plus, patients often start taking PPIs on their own - buying them over the counter. If your doctor doesn’t know you’re taking one, they won’t check. Always tell every provider about every medication, even OTC ones.
Are there any new drugs being developed to avoid this problem?
Yes. Pharmaceutical companies are now designing drugs that don’t rely on stomach pH for absorption. About 37% of new molecular entities in clinical trials use special coatings, pellets, or delivery systems that bypass the stomach entirely. Some are even using AI to predict absorption patterns. These innovations will help, but they’re years away from being mainstream. Until then, the risk remains.

Sarah B
February 7, 2026 AT 20:01Tola Adedipe
February 9, 2026 AT 07:44Eric Knobelspiesse
February 9, 2026 AT 15:37Marcus Jackson
February 11, 2026 AT 14:13Natasha Bhala
February 12, 2026 AT 01:35Jesse Lord
February 13, 2026 AT 23:46Catherine Wybourne
February 15, 2026 AT 14:13Amit Jain
February 17, 2026 AT 14:04Niel Amstrong Stein
February 19, 2026 AT 08:02Joey Gianvincenzi
February 21, 2026 AT 00:27Ritu Singh
February 22, 2026 AT 11:06Mark Harris
February 23, 2026 AT 11:17Paula Sa
February 24, 2026 AT 04:22