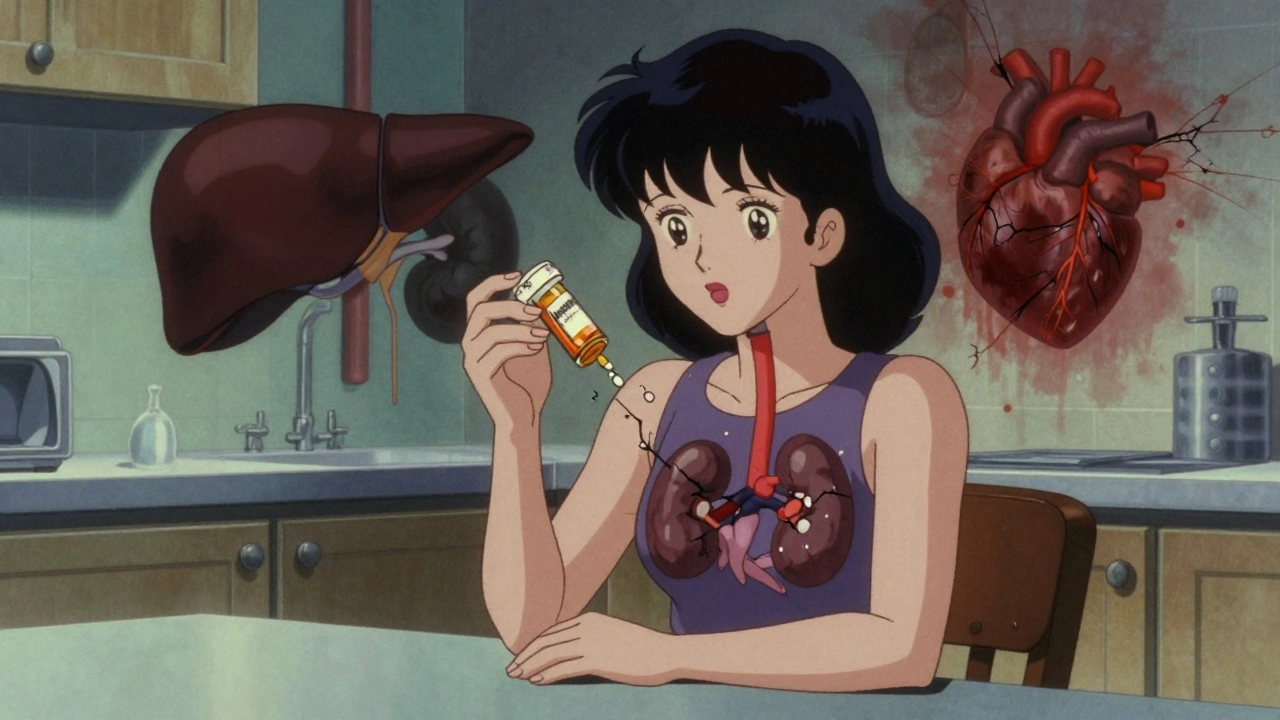
When you take a medication, it doesn’t always behave the same way in your body as it does in a lab. That’s where therapeutic drug monitoring, the process of measuring the amount of a drug in your blood to make sure it’s in the right range. Also known as TDM, it’s not just for hospitals — it’s a key tool for managing chronic conditions safely. Think of it like checking your car’s oil level: too little and the engine fails; too much and you risk damage. With drugs, the difference between helping and harming can be just a few nanograms per milliliter.
Some medications have a narrow window where they work best. NTI drugs, narrow therapeutic index medications like warfarin or digoxin are especially tricky. A small change in dose or absorption can lead to treatment failure or serious side effects. That’s why doctors check blood levels — not just to confirm you’re taking the pill, but to make sure your body is processing it correctly. Factors like age, liver function, kidney health, or even what you ate that day can shift how a drug behaves. drug interactions, like quercetin slowing down liver enzymes or calcium blocking thyroid medication absorption, can throw off those levels without you even noticing.
Therapeutic drug monitoring isn’t just about avoiding toxicity. It’s also about making sure you’re getting enough. If your seizure meds aren’t reaching the right level, you could have a breakthrough seizure. If your antidepressant is too low, you might feel like nothing’s working — even if you’re taking it daily. And with generics, especially for combination NTI drugs, multi-component medications where even tiny bioequivalence gaps can cause harm, monitoring becomes even more critical. A pill might look the same, but if your body absorbs it differently, your levels could drop — and no one would know unless they tested.
It’s not just for people on complex regimens. Even common drugs like gabapentin or lithium need tracking in some cases. Older adults, people with multiple conditions, or those on five or more meds are at higher risk for hidden imbalances. That’s why medication safety, the practice of preventing harm from drugs through careful dosing and monitoring isn’t just about avoiding side effects — it’s about making sure every pill you take actually does what it’s supposed to.
You won’t always hear about it, but therapeutic drug monitoring is happening behind the scenes for millions. It’s why your doctor asks for blood tests after starting a new drug. It’s why some pharmacies track your INR levels if you’re on warfarin. And it’s why switching to a generic isn’t always as simple as it seems. Below, you’ll find real-world examples of how drug levels affect treatment — from alcohol messing with blood thinners to supplements quietly changing how your meds work. These aren’t theoretical risks. They’re daily realities for people managing serious conditions. Let’s look at how others have navigated them.
Cumulative drug toxicity occurs when medications build up in your body over time, causing side effects that appear only after months or years. Learn which drugs are most risky and how to protect yourself.