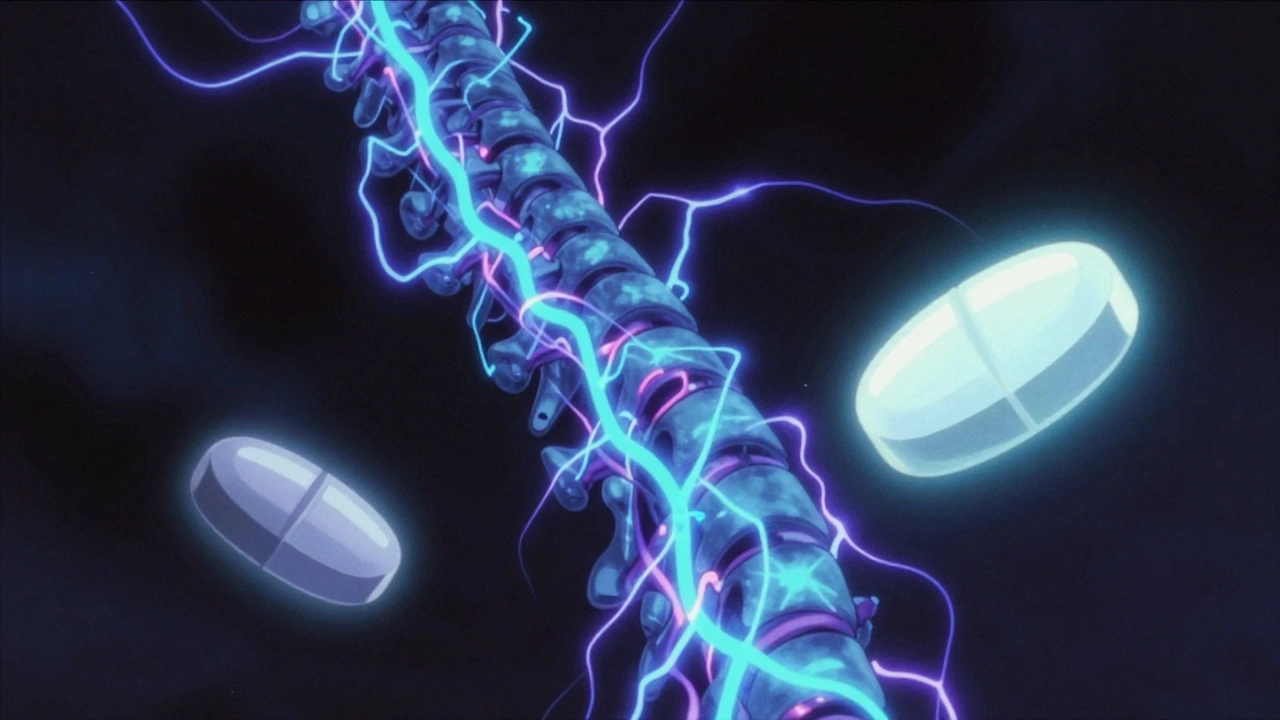
When your nerves get damaged, they don’t just send pain signals—they scream. This is neuropathic pain, a type of chronic pain caused by nerve damage or dysfunction, often described as burning, shooting, or electric shocks. Also known as nerve pain, it doesn’t respond to regular painkillers like ibuprofen or even high-dose acetaminophen. Instead, it needs targeted drugs that calm overactive nerves, not just reduce inflammation. Unlike muscle soreness or a sprained ankle, neuropathic pain lingers long after the injury heals—or shows up with no clear cause at all.
This kind of pain is linked to conditions like diabetes, shingles, spinal injuries, and even some chemotherapy treatments. It’s also why people on long-term meds like antidepressants, used off-label to stabilize nerve signals in chronic pain or anticonvulsants, originally for seizures but now common for nerve pain need careful monitoring. These drugs don’t just help with pain—they can interact with other meds you’re taking. For example, mixing certain antidepressants with supplements like L-tryptophan can trigger serotonin syndrome. Or, if you’re on blood thinners, even common OTC cold meds can raise bleeding risks. The body doesn’t treat pain in isolation; every drug you take changes how another works.
And here’s the catch: many people with neuropathic pain end up on multiple medications over time. That’s when cumulative drug toxicity, the slow buildup of side effects from long-term medication use becomes a real threat. A drug that seemed fine at first might start causing confusion, dizziness, or liver stress after months or years. Elderly patients are especially vulnerable, as aging slows how the body clears these drugs. Even something as simple as calcium supplements can mess with thyroid meds, and quercetin—often taken for allergies—can dangerously raise levels of other drugs by blocking liver enzymes. Managing neuropathic pain isn’t just about finding the right pill. It’s about understanding how every pill you take talks to the others.
What you’ll find below isn’t a list of quick fixes. It’s a collection of real, practical insights from people who’ve lived with this pain and the experts who treat it. You’ll see how generic drugs can be just as effective—but also riskier if not monitored. You’ll learn why alcohol might make nerve pain worse, how certain antibiotics can trigger dangerous heart rhythms in sensitive patients, and why timing your supplements matters more than you think. There’s no magic cure, but there’s a lot you can do to take control—without adding more risk to your daily routine.
Gabapentin and pregabalin are first-line treatments for neuropathic pain, but they differ in effectiveness, dosing, cost, and side effects. Learn which one may be better for your condition.