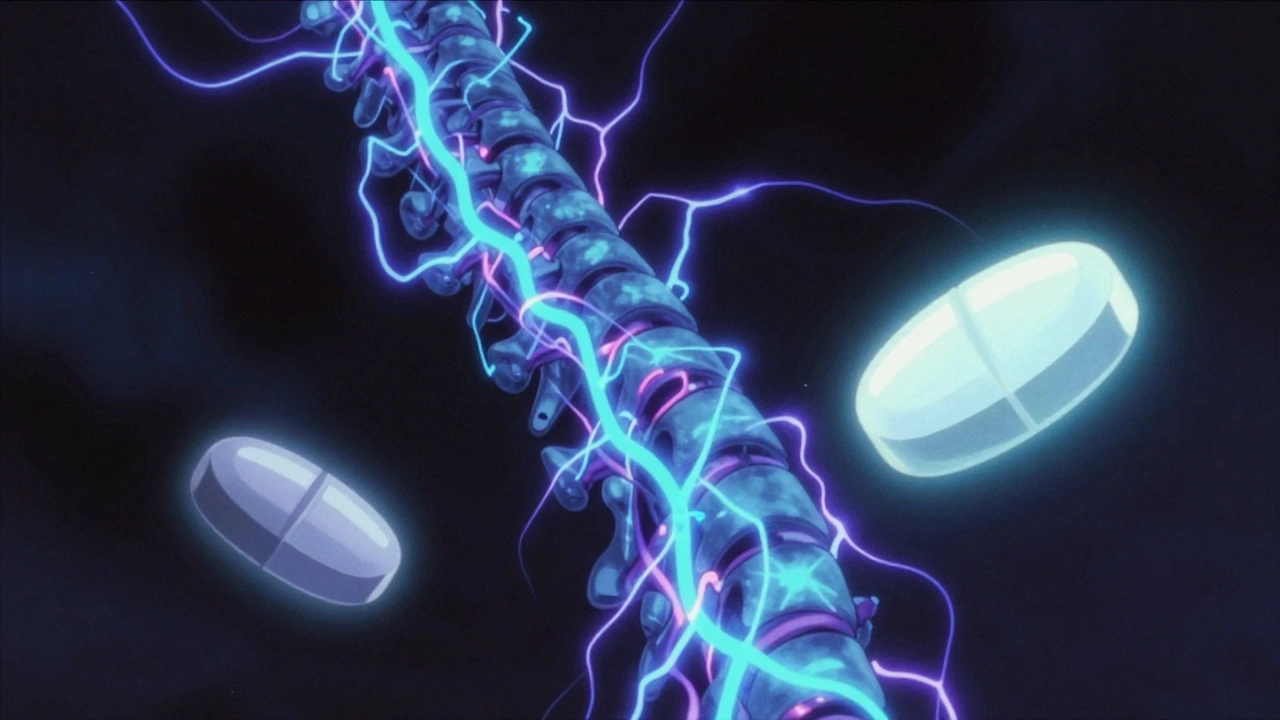
When your nerves are firing wrong, you don’t just feel pain—you feel electric shocks, burning, or pins and needles that won’t quit. This isn’t your typical ache. It’s nerve pain treatment, a category of therapies designed to calm overactive or damaged nerves, often caused by diabetes, injury, or long-term conditions. Also known as neuropathic pain, it doesn’t respond to regular painkillers like ibuprofen or acetaminophen, which is why so many people end up frustrated and confused. If you’ve been told "it’s just nerves" and left with no real plan, you’re not alone. The truth is, treating nerve pain isn’t about popping a pill and hoping for the best. It’s about matching the right drug to the type of nerve damage you have—and knowing what to avoid.
Two of the most common drugs used for gabapentin, an anticonvulsant repurposed to calm nerve signals, often prescribed for diabetic neuropathy and post-shingles pain and pregabalin, a similar but stronger version of gabapentin, approved for faster relief and fewer dose adjustments show up in over 60% of nerve pain cases. But they don’t work for everyone. Some people get dizziness or brain fog. Others feel nothing at all. That’s because nerve pain isn’t one condition—it’s a symptom with many roots. Diabetes, shingles, spinal injuries, even chemotherapy can trigger it. And each root needs a slightly different approach. That’s why you’ll find posts here about drug interactions, like how quercetin, a popular supplement that can interfere with liver enzymes and alter how nerve pain meds are processed, might make your treatment less effective—or more dangerous.
There’s also the issue of long-term use. Many people take these meds for months or years. That’s where cumulative drug toxicity, the slow buildup of side effects from daily medication use, often unnoticed until it’s too late becomes a real concern. You might not feel worse right away, but over time, your kidneys, liver, or even your balance can be affected. That’s why knowing how to monitor your meds matters as much as taking them. And if you’re older, or taking other drugs for heart issues or sleep, the risks stack up fast. You’ll find posts here that break down exactly how these interactions play out—like why mixing alcohol with certain nerve meds can make dizziness worse, or why calcium supplements might interfere with absorption if you’re on the wrong schedule.
This collection doesn’t just list drugs. It shows you how they fit into real life. You’ll see what patients actually experience with generics versus brand names, how timing affects results, and why some people stop taking meds not because they don’t work—but because they feel worse. There’s no magic bullet for nerve pain. But there are smarter ways to manage it. What follows are real, tested insights from people who’ve been through it, and the science behind why some treatments stick—and others don’t.
Gabapentin and pregabalin are first-line treatments for neuropathic pain, but they differ in effectiveness, dosing, cost, and side effects. Learn which one may be better for your condition.