When it comes to your health, healthcare communication, the clear exchange of information between patients, doctors, and pharmacists. Also known as patient-provider dialogue, it’s not just about talking—it’s about being understood and understanding others. Too many people leave the doctor’s office confused, unsure if they took their pill right, or afraid to ask what that weird abbreviation on the label really means. That’s where things go wrong—medication errors, missed doses, dangerous interactions. This isn’t theory. It’s why people end up in the ER because they mixed warfarin with an OTC cold medicine, or why someone on azithromycin didn’t know their heart was at risk.
Prescription labels, the small print that tells you when and how to take your medicine. Also known as medication instructions, they’re written in shorthand like BID, TID, and PRN—not for doctors, but for you. If you don’t know what those mean, you’re guessing. And guessing with pills is dangerous. Then there’s drug interactions, when one medicine changes how another works in your body. Also known as medication conflicts, they’re silent killers—like alcohol making warfarin spike your INR, or aspirin messing with seizure meds. And it’s not just about pills. It’s about who you talk to: your pharmacist, your support group, your nurse. Patient support groups, communities where people share real experiences with generics, side effects, and how to stick with treatment. Also known as medication communities, they’re often the missing link when the system fails.
You don’t need a medical degree to protect yourself. You just need to know what to ask. What’s this pill for? What happens if I skip it? What should I avoid mixing it with? Can I take this with my coffee? These aren’t silly questions—they’re survival questions. The posts below show you exactly how to read your labels, spot hidden dangers in OTC meds, understand why your doctor chose one drug over another, and how others have navigated the same confusion. You’ll find real stories from people managing lupus with deflazacort, college students avoiding stimulant misuse, and seniors learning how to cut back on opioids safely. No jargon. No fluff. Just what works.
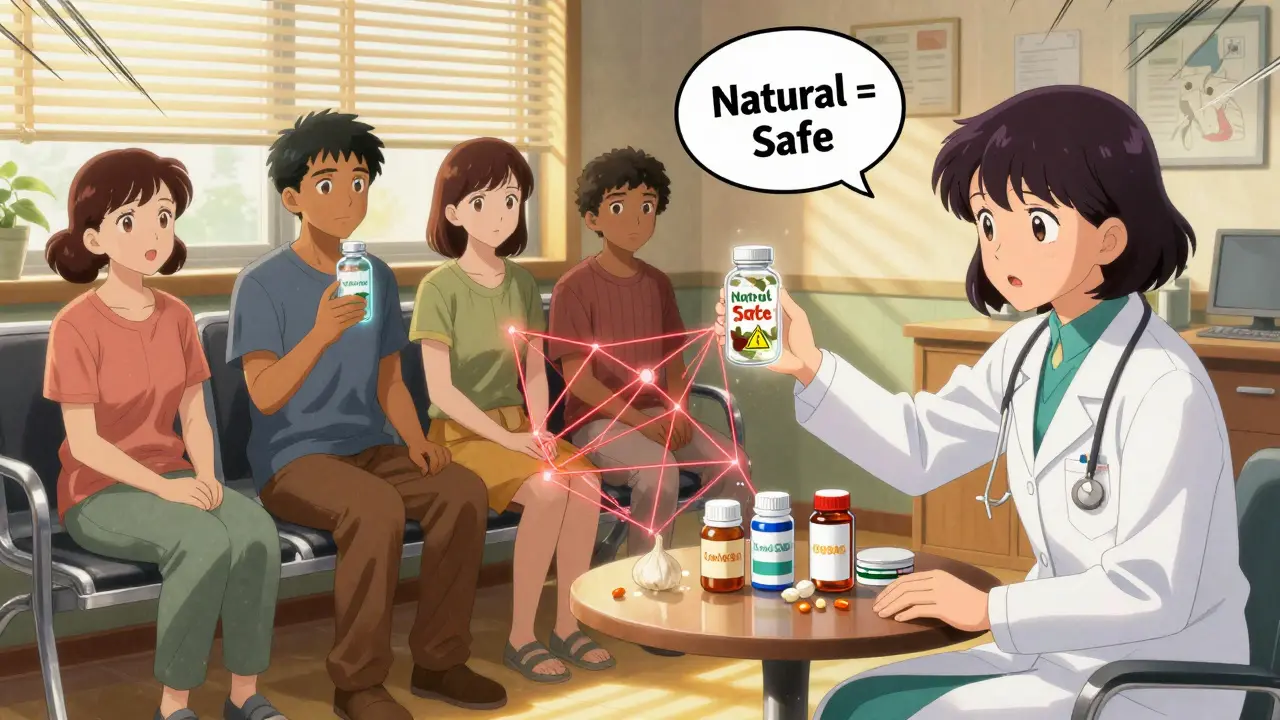
Many people take dietary supplements without telling their doctors-but this silence can lead to dangerous drug interactions. Learn why full disclosure is essential for your safety and how to talk to your care team effectively.

Institutional healthcare communication programs train providers to improve patient understanding, reduce errors, and lower burnout. Learn how evidence-based training works, which programs deliver results, and what still needs to change.