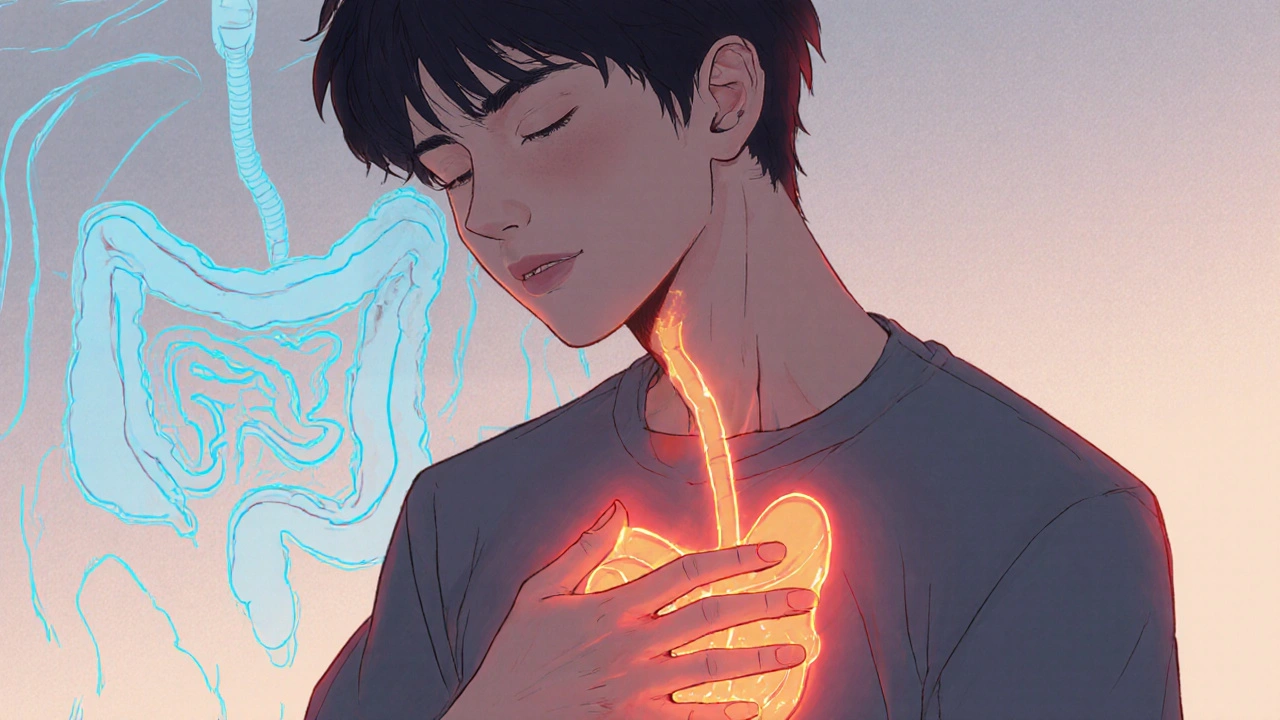
When dealing with GERD, gastroesophageal reflux disease is a chronic condition where stomach acid frequently backs up into the esophagus, causing heartburn, regurgitation, and irritation. Also known as acid reflux, it can affect anyone but is especially common among people with certain lifestyle factors. Understanding how it works helps you pick the right treatment and make smart daily choices.
Proton Pump Inhibitors (PPIs), medications that lower stomach acid production by blocking the enzyme responsible for acid secretion are often the first line of therapy. They relieve symptoms, allow damaged tissue to heal, and are the key ingredient in many over‑the‑counter options like omeprazole. However, long‑term use can have downsides, so clinicians weigh benefits against risks such as nutrient malabsorption. Our guide on buying cheap generic Prilosec online walks you through safe purchasing, price comparison, and how to avoid counterfeit pills.
Obesity, excess body fat that puts pressure on the abdomen and weakens the lower esophageal sphincter is a major driver of GERD. Studies show that even a modest weight reduction can cut reflux episodes by half. That’s why diet and exercise often appear alongside drug therapy in comprehensive care plans. We also cover how obesity links to urine leakage and pelvic‑floor strain, because the same pressure dynamics affect multiple organs.
Dehydration, insufficient fluid intake that thickens stomach contents and slows digestion can worsen reflux by increasing gastric acidity and delaying emptying. Staying well‑hydrated dilutes acid and promotes smoother gut motility, making it a simple but effective habit for many patients. Our article on dehydration‑induced bladder spasms shows the broader impact of fluid balance on urinary and gastrointestinal health.
Pelvic floor exercises, targeted muscle training that strengthens the diaphragm and lower esophageal sphincter support have gained attention for their role in reducing nighttime reflux. Regular Kegel‑style routines can improve intra‑abdominal pressure control, complementing medication and weight‑loss efforts. The same techniques are detailed in our guide on easing urinary tract spasms, so you get a full picture of how core strength benefits both gut and bladder.
Beyond the big three—meds, weight, and hydration—daily habits matter a lot. Eating large meals or lying down right after dinner lets acid splash upward more easily. Aim for smaller portions, chew slowly, and wait at least two to three hours before bedtime. Elevating the head of the bed by six to eight inches helps gravity keep acid down while you sleep.
Smoking and alcohol are another pair of culprits. Nicotine relaxes the lower esophageal sphincter, while alcohol increases acid production. Cutting back or quitting can shrink symptom frequency dramatically. If you enjoy a nighttime glass of wine, try a lower‑acid alternative or limit intake to the early evening.
Spicy foods, citrus, chocolate, and mint are common triggers, but individual tolerance varies. Keep a simple food diary for a week: note what you eat, when symptoms appear, and any relief measures you try. Over time you’ll spot patterns and can fine‑tune your diet without sacrificing enjoyment.
Our site’s broader collection often explores medication comparisons—like Betadine versus other antiseptics or Olanzapine versus its rivals—to show how we break down complex drug info into easy choices. The same rigorous approach applies to GERD meds: we compare PPIs, H2 blockers, antacids, and newer alginate formulas so you can see which option fits your budget and health profile.
Stress isn’t just a mental issue; it can raise stomach acid and slow digestion. Mind‑body practices such as deep breathing, gentle yoga, or short walks after meals can calm the gut‑brain axis. When you pair these techniques with solid sleep hygiene—regular bedtime, a cool dark room—you give your esophagus a fighting chance to heal.
Finally, keep an eye on vitamin and mineral intake. Long‑term PPI use may lower absorption of B12, magnesium, and calcium. A daily multivitamin or periodic blood tests can catch deficiencies early, preventing fatigue or bone loss down the line.
All these pieces—medication insight, weight management, proper hydration, core strengthening, and smart daily habits—come together in a practical plan that many of our readers have found life‑changing. Below you’ll see a curated list of articles that dive deeper into each topic, from buying affordable generic drugs to mastering pelvic floor routines, so you can build a complete toolbox for managing GERD.
Learn how epigastric pain signals GERD, get clear diagnosis steps, and discover effective lifestyle, medication, and surgical treatments for lasting relief.