When doctors prescribe gabapentinoids, a class of medications originally developed for epilepsy but now widely used for nerve pain and anxiety. Also known as gabapentin-like drugs, they include gabapentin and pregabalin, two of the most commonly prescribed drugs in this group. These aren’t traditional painkillers like ibuprofen or opioids. Instead, they calm overactive nerves—making them useful for conditions like diabetic neuropathy, post-shingles pain, and even certain types of anxiety. But they’re not harmless. Many people take them long-term without knowing how they work or what side effects to expect.
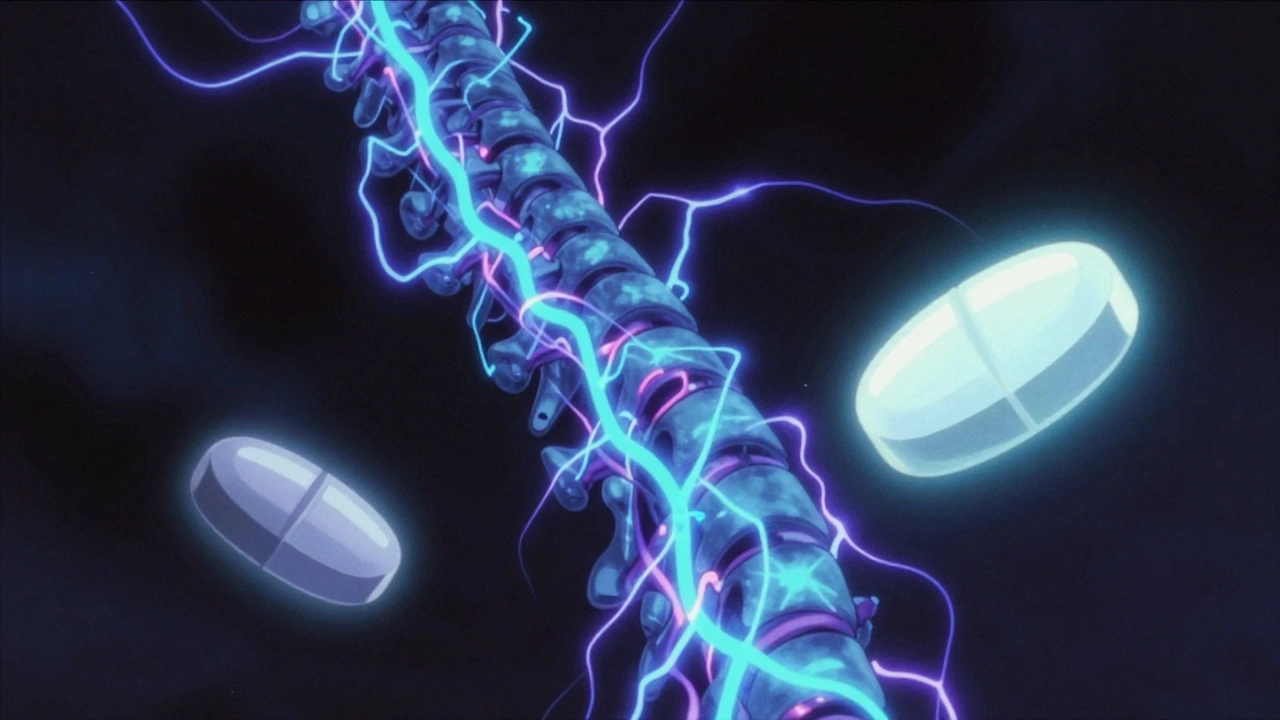
Gabapentinoids work by binding to calcium channels in the brain and spinal cord, reducing the release of neurotransmitters that signal pain or seizures. That’s why they help with nerve pain but won’t touch a headache or muscle strain. The difference between gabapentin and pregabalin isn’t just price—pregabalin works faster, is more predictable in how it’s absorbed, and is often prescribed at lower doses. But both can cause dizziness, drowsiness, weight gain, and brain fog. Some people feel like they’re walking through syrup. And while these drugs are rarely fatal on their own, mixing them with alcohol, opioids, or benzodiazepines can be deadly. The CDC has flagged gabapentinoids as part of the rising opioid-related death trend—not because they’re opioids, but because they’re often used together with them.
What’s more, these medications are prescribed far more often than the science supports. Studies show they’re effective for certain nerve pain conditions, but not for lower back pain, migraines, or insomnia—yet they’re still handed out for all of those. And because they’re not tightly controlled in many places, people sometimes get them without a proper diagnosis. If you’ve been on gabapentin for years and aren’t sure why, it’s worth asking your doctor if it’s still helping—or if it’s just becoming another daily pill you don’t need.
There’s also growing concern about withdrawal. Stopping gabapentinoids suddenly can trigger anxiety, insomnia, nausea, and even seizures in rare cases. That’s why tapering slowly matters. And if you’re switching from one to another—say, from gabapentin to pregabalin—you can’t just swap doses. The body handles them differently. A 300mg dose of gabapentin isn’t the same as 75mg of pregabalin. Getting that wrong can mean either no relief or too many side effects.
What you’ll find below are real, practical guides on how gabapentinoids interact with other drugs, what side effects people actually report, how they affect sleep and cognition, and why some patients do better than others. You’ll see how they connect to broader issues like polypharmacy in older adults, drug accumulation over time, and the risks of combining supplements with prescriptions. These aren’t theoretical discussions. They’re based on what people experience—and what doctors are starting to rethink.
Gabapentin and pregabalin are first-line treatments for neuropathic pain, but they differ in effectiveness, dosing, cost, and side effects. Learn which one may be better for your condition.