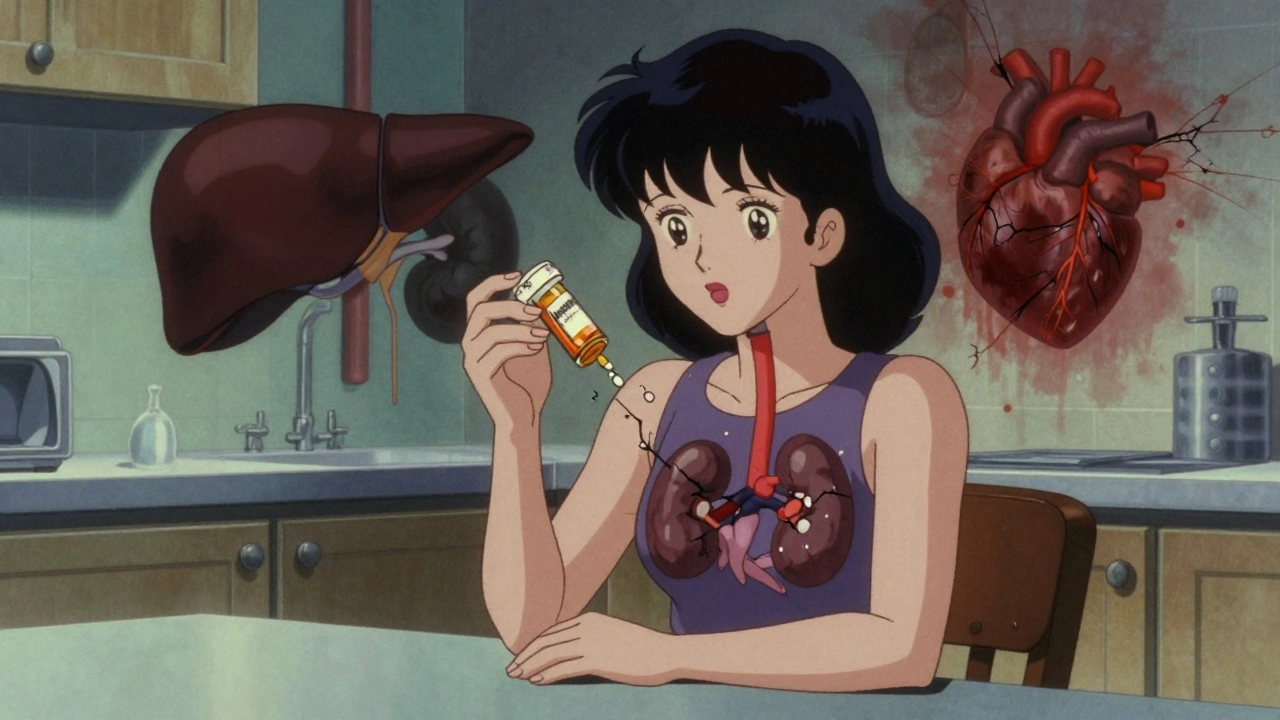
When you take a medication over days or weeks, your body doesn’t always clear it all before the next dose. That leftover amount adds up—that’s the cumulative dose, the total amount of a drug that has built up in your system over time from repeated doses. Also known as drug accumulation, it’s not just a number on a chart—it’s what makes some pills safe to take daily and others dangerously risky if you miss a dose or take too much. This isn’t just for opioids or sedatives. Even common drugs like gabapentin, acetaminophen, or SSRIs can build up in your system, especially if your liver or kidneys aren’t working at full speed.
Why does this matter? Because the therapeutic window, the range between a drug’s effective dose and its toxic dose is often narrow. Take too little, and it doesn’t work. Take too much—because you didn’t realize the dose was stacking up—and you could end up in the ER. That’s why doctors track cumulative dose for drugs like lithium or digoxin. But it’s also critical for over-the-counter painkillers. If you’ve been taking 1,000 mg of acetaminophen four times a day for two weeks, you’ve hit over 14,000 mg—way past the safe daily limit. Your liver doesn’t tell you it’s overwhelmed until it’s too late.
Age, other meds, and even what you eat can change how fast your body clears a drug. Elderly patients are especially at risk because kidney and liver function slow down naturally. And if you’re on multiple medications—like a blood thinner, an antidepressant, and a painkiller—some of them can block the enzymes that break down others. Quercetin, for example, can slow how fast your body processes certain drugs, making the cumulative dose climb faster than expected. Even alcohol can interfere, especially with drugs like warfarin or gabapentin, where small changes in blood levels lead to big changes in how you feel or how safe you are.
You don’t need to be a scientist to track this. Just know: if you’ve been on a med for more than a few days, the total amount you’ve taken matters. Check your pill bottles. Write down how many pills you’ve taken each day. Ask your pharmacist: "Does this build up?" If you’re switching from brand to generic, or if your doctor changes your dose, ask if the new dose could push your cumulative dose into risky territory. That’s why patient stories in support groups often mention confusion over why they felt worse after a "small" change—it wasn’t the dose alone, it was the total they’d already taken.
What you’ll find below are real-world examples of how cumulative dose plays out in everyday medicine. From gabapentin and pregabalin to warfarin and thyroid meds, these posts show you how drug buildup affects safety, effectiveness, and side effects. You’ll see how timing, interactions, and individual differences make one person’s safe dose another’s danger zone. No theory. No fluff. Just what you need to know to take your meds without surprises.
Cumulative drug toxicity occurs when medications build up in your body over time, causing side effects that appear only after months or years. Learn which drugs are most risky and how to protect yourself.