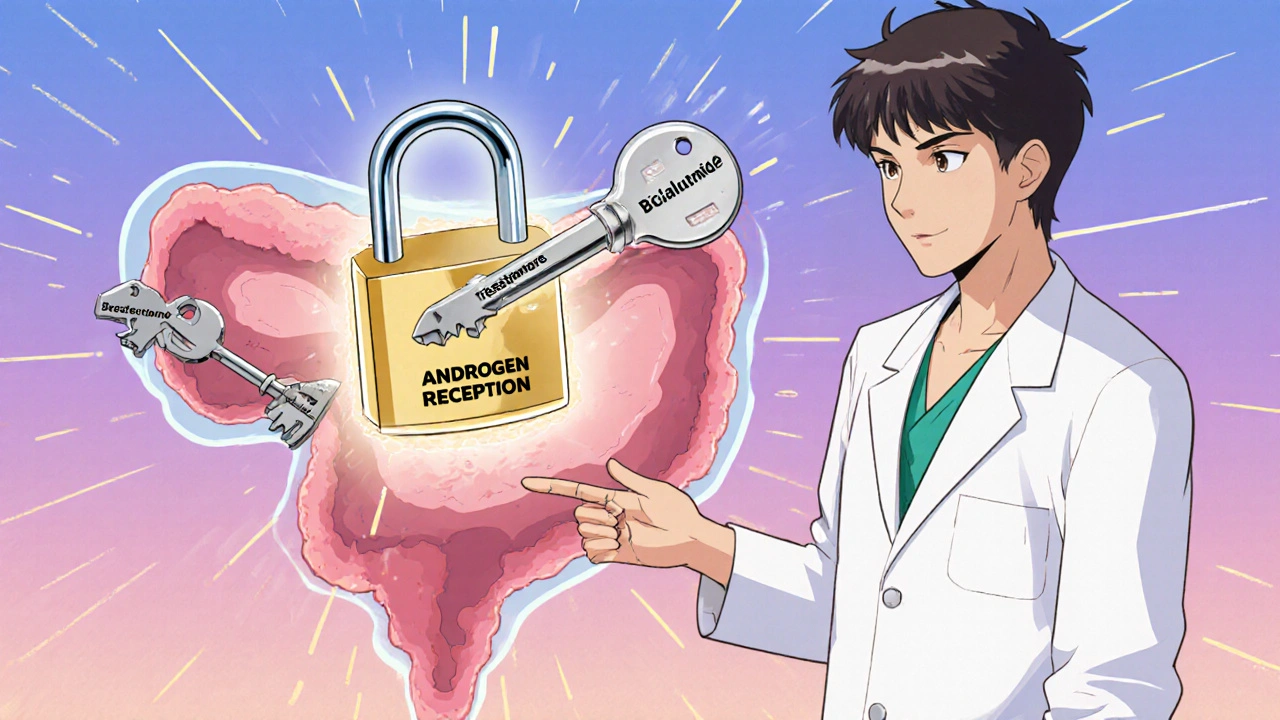
When you’re prescribed bicalutamide, a non-steroidal anti-androgen used primarily to treat prostate cancer by blocking testosterone’s effects on cancer cells. It’s not a cure, but it slows progression—especially when paired with other therapies like LH-RH agonists. Unlike chemo, it doesn’t kill cells outright; it starves them of the signals they need to grow. That’s why it’s often chosen for men who need long-term control without the brutal toll of stronger treatments.
But safety isn’t just about whether it works—it’s about what it does to your body over time. The biggest red flag? liver damage, a rare but serious risk that can develop without symptoms until it’s advanced. About 1 in 100 people on bicalutamide show abnormal liver enzymes, and a fraction develop hepatitis. That’s why your doctor should check your liver function every 3 months, especially in the first year. If you notice yellow skin, dark urine, or unexplained fatigue, stop taking it and get tested—don’t wait. Other common issues include hot flashes, breast tenderness, and loss of libido. These aren’t life-threatening, but they’re real and can mess with your quality of life. Some men even develop gynecomastia—enlarged breasts—which can be emotionally tough. Compression shirts or, in rare cases, surgery help, but prevention starts with early talk to your doctor.
Drug interactions, especially with medications that affect liver enzymes like warfarin or certain antidepressants, can change how bicalutamide behaves in your system. If you’re on blood thinners, your INR levels might spike. If you take SSRIs, you could feel more fatigued or dizzy. Always tell every provider you see—dentists, ER staff, even pharmacists—that you’re on bicalutamide. It’s not just about pills; alcohol and certain herbal supplements like St. John’s Wort can also interfere. And if you have a history of liver disease, heart problems, or seizures, your doctor might avoid it altogether or start you on a lower dose.
What you won’t hear from the pamphlet? Many men stay on bicalutamide for years. It’s not a short-term fix. That’s why tracking matters: keep a journal of side effects, mood changes, or new aches. Bring it to every appointment. Some clinics use digital apps now to log symptoms automatically—ask if yours does. The goal isn’t just to survive treatment, but to live well during it. You’re not just a patient with prostate cancer—you’re someone who still wants to work, travel, play with grandkids, or just sleep through the night without hot flashes.
What follows are real-world comparisons, patient experiences, and clinical insights from posts that dig into how bicalutamide stacks up against other hormone blockers, what to do when side effects get bad, and how to spot early warning signs before they become emergencies. No theory. No fluff. Just what people actually deal with—and what works.
A clear, up‑to‑date guide on Bicalutamide covering its uses, dosage, side effects, monitoring, and drug interactions for prostate cancer patients.