When working with pain relief dosage, the exact amount of medication required to ease pain while minimizing risk. Also known as analgesic dosing, it serves as the backbone of any pain‑management plan. Understanding the numbers helps you avoid under‑treating pain and prevents dangerous side effects.
pain relief dosage isn’t a one‑size‑fits‑all figure; it changes with age, weight, kidney function, and the type of drug you’re using. For example, acetaminophen dosage, the daily limit of this common over‑the‑counter pain reliever is capped at 4 g for most adults, but drops to 3 g for those with liver concerns. Exceeding that limit can lead to serious liver injury, a risk that many people overlook.
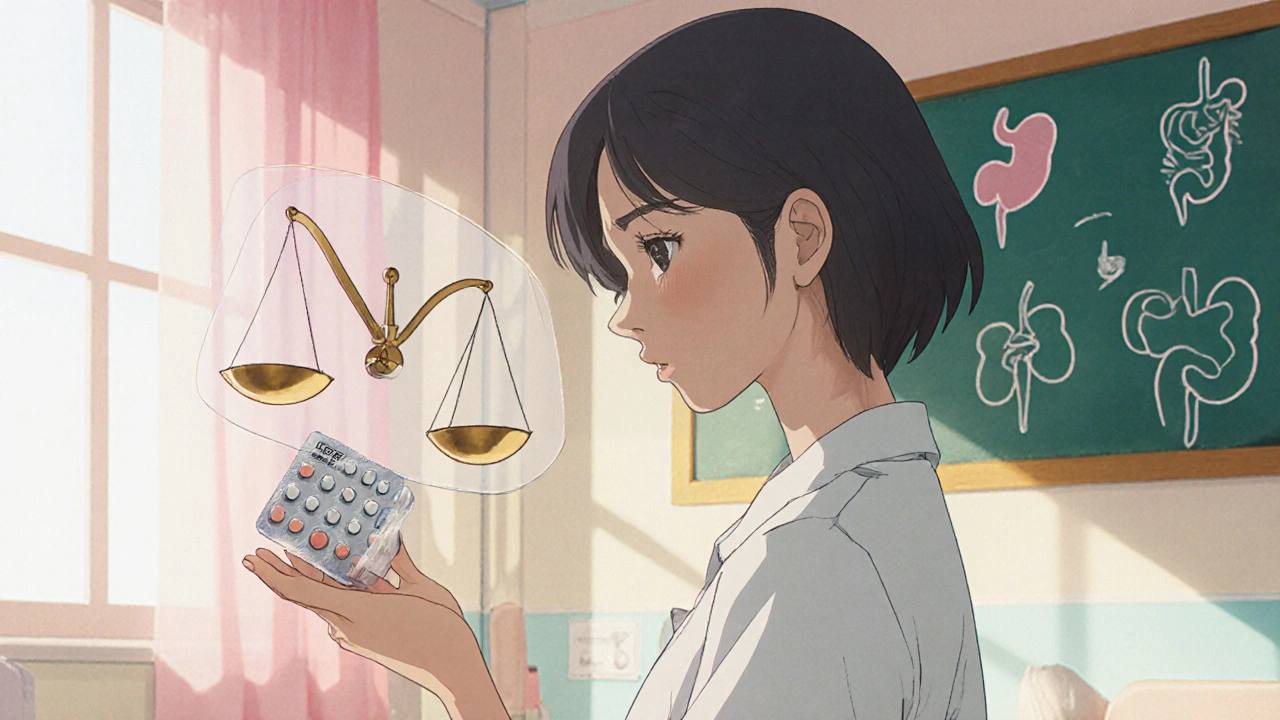
First, the drug class matters. NSAID dosage, the amount of non‑steroidal anti‑inflammatory drugs like ibuprofen or naproxen must consider stomach lining health because higher doses increase the chance of ulcers. Second, patient characteristics such as age and kidney function shape the safe range. Third, the pain’s origin—whether it’s a headache, joint inflammation, or post‑surgical pain—guides the choice of medication and its dosing schedule.
When the pain is moderate to severe, many clinicians turn to opioids. opioid dosage, the calibrated amount of opioid medication prescribed for pain control follows strict guidelines because of addiction potential and respiratory depression risks. Starting low and going slow is the standard rule: a low initial dose, reassessing after 24‑48 hours, and adjusting only if pain remains uncontrolled.
Even within the same class, individual drugs have distinct dosing limits. ibuprofen dosage, the recommended maximum amount of ibuprofen per day for adults is 1,200 mg over‑the‑counter, but a doctor may prescribe up to 3,200 mg for short‑term use in severe inflammation. Knowing the ceiling helps you avoid kidney strain and high blood pressure spikes.
Another crucial variable is timing. Some analgesics work best when taken with food, while others need an empty stomach for optimal absorption. For instance, taking NSAIDs with a meal reduces gastric irritation, whereas acetaminophen’s effectiveness isn’t heavily food‑dependent. Aligning dose timing with daily routines improves adherence and keeps pain under control.
Drug interactions also reshape dosage decisions. Combining acetaminophen with alcohol, or mixing NSAIDs with certain blood thinners, can magnify side effects. Always check a medication’s interaction profile before stacking pain relievers, especially if you’re on chronic prescriptions.
Special populations need extra caution. Children receive weight‑based dosing; a toddler’s ibuprofen dose is calculated in mg per kilogram, not a flat adult tablet. Elderly patients often have reduced renal clearance, so a lower NSAID dose is safer. Pregnant people must avoid certain NSAIDs in the third trimester and adjust opioid use under close medical supervision.
Finally, monitoring is part of the dosage cycle. Track pain scores, side effects, and any signs of over‑medication, such as drowsiness from opioids or unusual bruising from NSAIDs. Regular check‑ins allow your healthcare provider to fine‑tune the regimen before problems arise.
Below you’ll find a curated list of articles that dive deeper into each of these topics—acetaminophen limits, ibuprofen best practices, opioid safety, and more. Browse the collection to get the specifics you need for safe, effective pain relief.
Learn how to determine the correct diclofenac sodium dosage, covering forms, safe limits, risk factors, interactions, and practical tips for safe use.