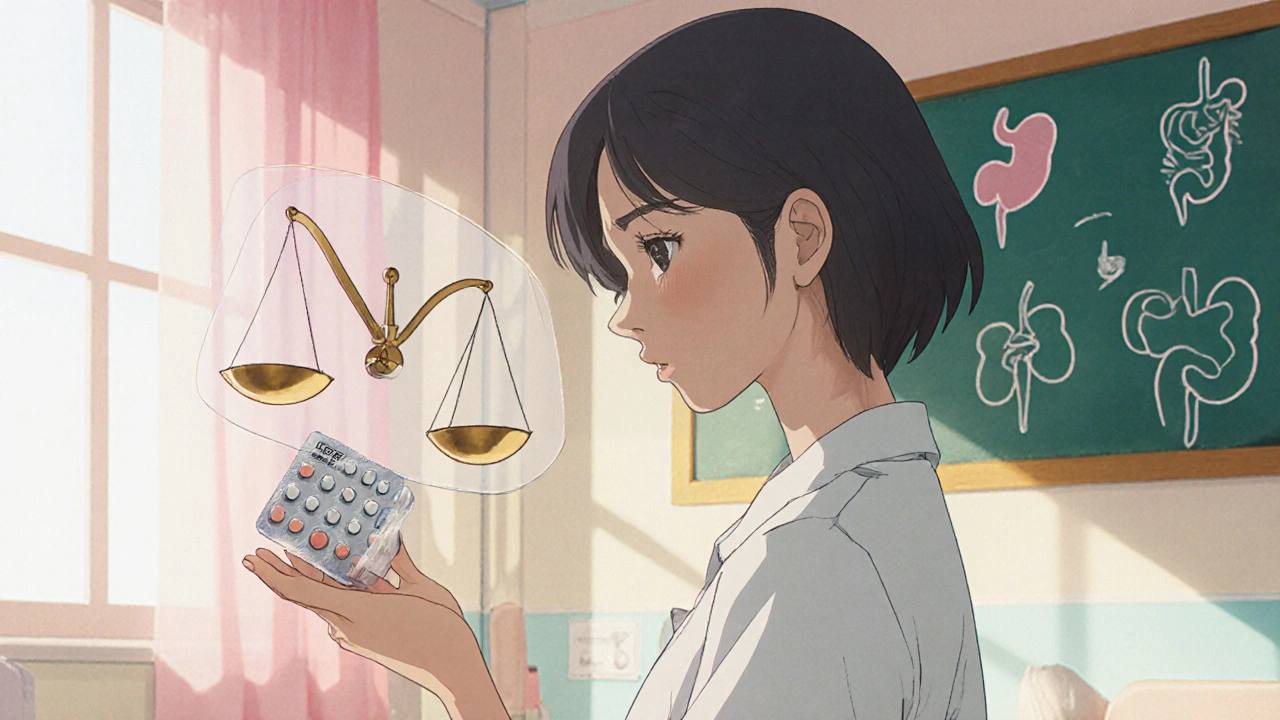
When working with NSAID dosing, determining the right amount of non‑steroidal anti‑inflammatory drugs for each patient. Also known as NSAID dose calculation, it aims to balance effective pain relief with minimized side effects. NSAID dosing can feel like a puzzle because each drug has its own strength, half‑life, and organ impact. Getting the math right means fewer stomach aches, lower kidney risk, and better pain control. Below we break down the core pieces you need to consider before you write a prescription or grab an over‑the‑counter bottle.
Most clinicians start with the most common agents: Ibuprofen, a short‑acting NSAID often used for headaches, muscle pain, and fever. The standard adult dose is 200‑400 mg every 4‑6 hours, not exceeding 1,200 mg without doctor supervision. For chronic conditions like osteoarthritis, the ceiling can rise to 2,400 mg, but only under close monitoring.
Another workhorse is Naproxen, a longer‑acting NSAID that stays in the system for up to 12 hours. Typical dosing starts at 250‑500 mg twice daily, with a maximum of 1,500 mg per day for most adults. Because naproxen hangs around longer, it’s a go‑to for inflammatory arthritis when patients want fewer pills.
Both ibuprofen and naproxen share the same dosing principle: calculate based on body weight for children, adjust for renal function in older adults, and watch for drug‑drug interactions. That’s why NSAID dosing always includes a quick check of kidney health, liver enzymes, and any anticoagulants the patient may be taking.
Beyond the two giants, other NSAIDs like diclofenac, celecoxib, and ketorolac have their own limits. Diclofenac caps at 150 mg per day, celecoxib (a COX‑2‑selective option) usually stays under 200 mg, and ketorolac—reserved for short‑term hospital use—should never exceed 5 days because of its high bleeding risk. Knowing these caps helps you avoid accidental overdose.
When you combine NSAIDs with other meds, the math changes. For instance, adding a proton‑pump inhibitor (PPI) can protect the stomach, allowing a slightly higher dose for patients with a history of ulcers. Conversely, pairing an NSAID with an ACE inhibitor or diuretic raises the chance of kidney injury, so you might need to lower the dose or switch drugs.
Age matters, too. Elderly patients often have reduced clearance, so a 25 % dose reduction is a common rule of thumb. If a senior is on multiple blood thinners, you may choose a COX‑2‑selective NSAID like celecoxib to cut bleeding risk while still tackling inflammation.
For kids, weight‑based dosing is non‑negotiable. Ibuprofen is usually prescribed at 5‑10 mg/kg every 6‑8 hours, never past 40 mg/kg per day. Naproxen for children is less common, but when used, the dose sits around 5 mg/kg twice daily. Always round to the nearest appropriate suspension concentration to keep dosing simple.
Finally, remember the timing of doses. Taking an NSAID with food or milk can blunt stomach irritation, but it may also slow absorption slightly—usually not a problem for pain control but worth noting for acute fever spikes.
All these pieces—drug choice, maximum daily limit, patient age, organ function, and concurrent meds—form the backbone of safe NSAID dosing. By checking each factor, you can tailor a regimen that relieves pain without inviting side effects.
Ready to see how these guidelines play out in real‑world scenarios? Below you’ll find detailed comparisons, dosing charts, and practical tips that walk you through choosing the right NSAID for common conditions, handling special populations, and avoiding the most common pitfalls.
Learn how to determine the correct diclofenac sodium dosage, covering forms, safe limits, risk factors, interactions, and practical tips for safe use.