When you're living with systemic lupus erythematosus, a chronic autoimmune disease where the immune system attacks healthy tissue, often affecting skin, joints, kidneys, and organs. Also known as SLE, it doesn't have a cure—but it can be managed. Many people mistake lupus for just joint pain or a rash, but it’s deeper than that. It flares up unpredictably, and what works for one person might do nothing—or even make things worse—for another.
The backbone of most lupus treatment, a personalized plan to control symptoms, prevent flares, and protect organs from long-term damage. Also known as SLE management, it starts with drugs you’ve probably heard of: hydroxychloroquine, an antimalarial drug that reduces inflammation and flare frequency in over 70% of lupus patients. Also known as Plaquenil, it is often the first and longest-used medication. It’s not a quick fix, but studies show it lowers the risk of organ damage over time. Then come corticosteroids, powerful anti-inflammatories like prednisone used during flares, but avoided long-term due to side effects like weight gain, bone loss, and diabetes. Also known as steroids, they are like fire extinguishers—effective in emergencies, but dangerous if you keep using them. For more severe cases, doctors turn to immunosuppressants, drugs like azathioprine or mycophenolate that quiet the overactive immune system without the broad damage of steroids. Also known as immune modulators, they take weeks to kick in but can keep lupus under control for years.
What you won’t find in most treatment guides? The real trade-offs. Hydroxychloroquine needs regular eye checks. Steroids can wreck your mood and sleep. Immunosuppressants make you more vulnerable to infections. And no one talks enough about how lifestyle—sun protection, stress control, quitting smoking—can be as important as the pills. The goal isn’t to eliminate lupus. It’s to live with it without letting it take over your life.
Below, you’ll find real, no-nonsense comparisons of medications, what they actually do to your body, and how people manage side effects in daily life. No marketing. No guesswork. Just what’s been tried, what failed, and what actually helped.
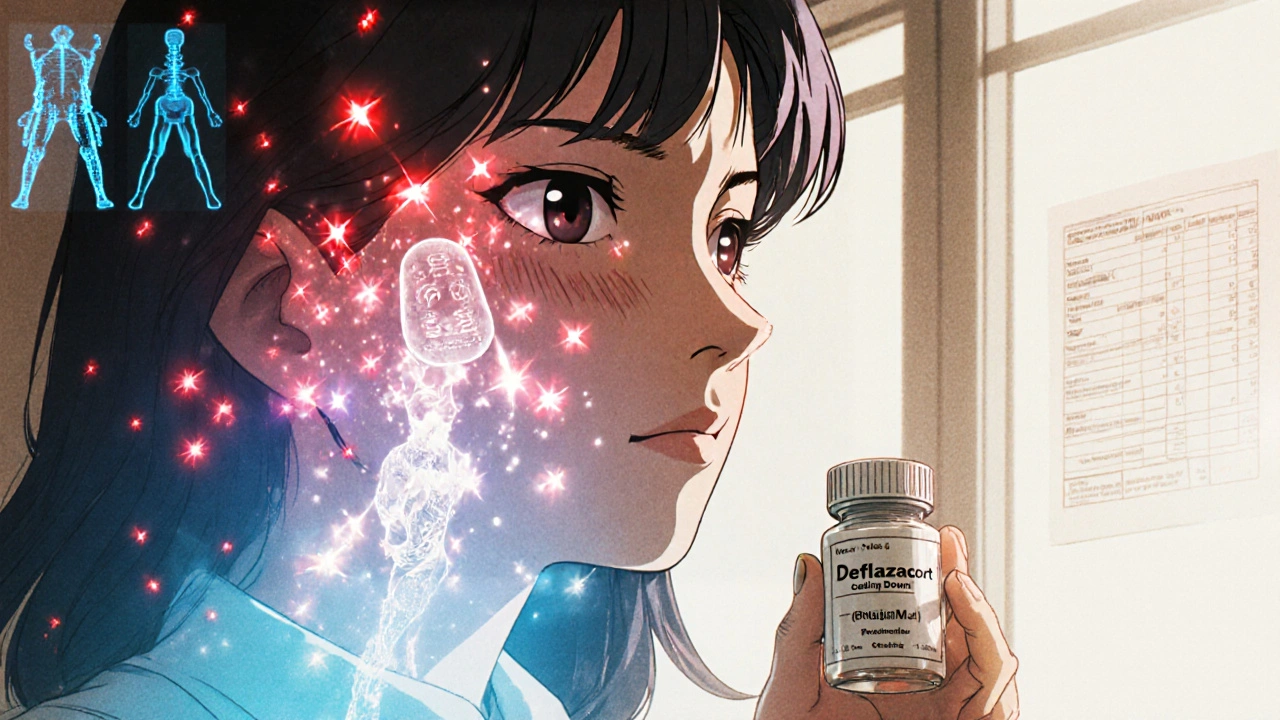
Deflazacort offers a potentially safer alternative to prednisone for lupus patients, with fewer metabolic side effects like weight gain and blood sugar spikes. Learn how it works, who benefits most, and how to talk to your doctor about switching.