When you hear leptomeningeal metastases, a condition where cancer cells infiltrate the thin membranes covering the brain and spinal cord, also called meningeal carcinomatosis, you probably wonder how it happens and why it matters. In simple terms, tumor cells travel from a primary site—most often lung, breast, or melanoma—and hitch a ride in the cerebrospinal fluid (CSF) to coat the meninges. This spread triggers a mix of headaches, vision changes, and motor weakness because the nerves and brain tissue get squeezed or irritated. Understanding these basics sets the stage for spotting the disease early and choosing the right therapy.
Leptomeningeal metastases is tightly linked to several other entities. First, primary cancers, especially non‑small‑cell lung carcinoma, HER2‑positive breast cancer, and melanoma, act as the source. Second, diagnostic tools, like contrast‑enhanced MRI and lumbar puncture, provide the evidence you need. A classic semantic triple here is: Leptomeningeal metastases requires CSF analysis. Another is: Advanced MRI reveals meningeal enhancement indicative of tumor spread. And because treatment hinges on drug delivery, we see: Intrathecal chemotherapy enables direct targeting of cancer cells in the CSF. Together, these entities form a loop—primary tumor → CSF seeding → neurological signs → imaging and CSF sampling → targeted therapy.
When it comes to symptoms, people often report a blend of cranial nerve palsies, balance problems, and diffuse pain. These signs point to the meninges being irritated across the central nervous system. Recognizing this pattern early can prompt a quick MRI, which looks for the tell‑tale thin, linear enhancements along the sulci. If imaging is suggestive, a lumbar puncture follows to collect CSF for cytology—the gold‑standard test that spots malignant cells. The combination of imaging and CSF cytology boosts diagnostic accuracy to over 80% in specialized centers.
Therapeutically, the landscape includes intrathecal chemotherapy (methotrexate, cytarabine, or liposomal cytarabine), focal radiation to symptomatic sites, and systemic targeted agents that cross the blood‑brain barrier. Recent trials show that patients with HER2‑positive breast cancer benefit from intrathecal trastuzumab, while those with EGFR‑mutated lung cancer see improved outcomes with osimertinib, which penetrates the CSF. Prognosis remains guarded, with median survival ranging from 3 to 6 months without treatment, but aggressive multimodal approaches can extend life and improve quality of living.
This collection below pulls together practical guides, drug comparisons, and the latest research on leptomeningeal metastases. Whether you’re looking for a step‑by‑step diagnostic checklist, a rundown of intrathecal chemotherapy options, or tips on managing neurological symptoms, you’ll find focused, up‑to‑date information to help you navigate this challenging condition.
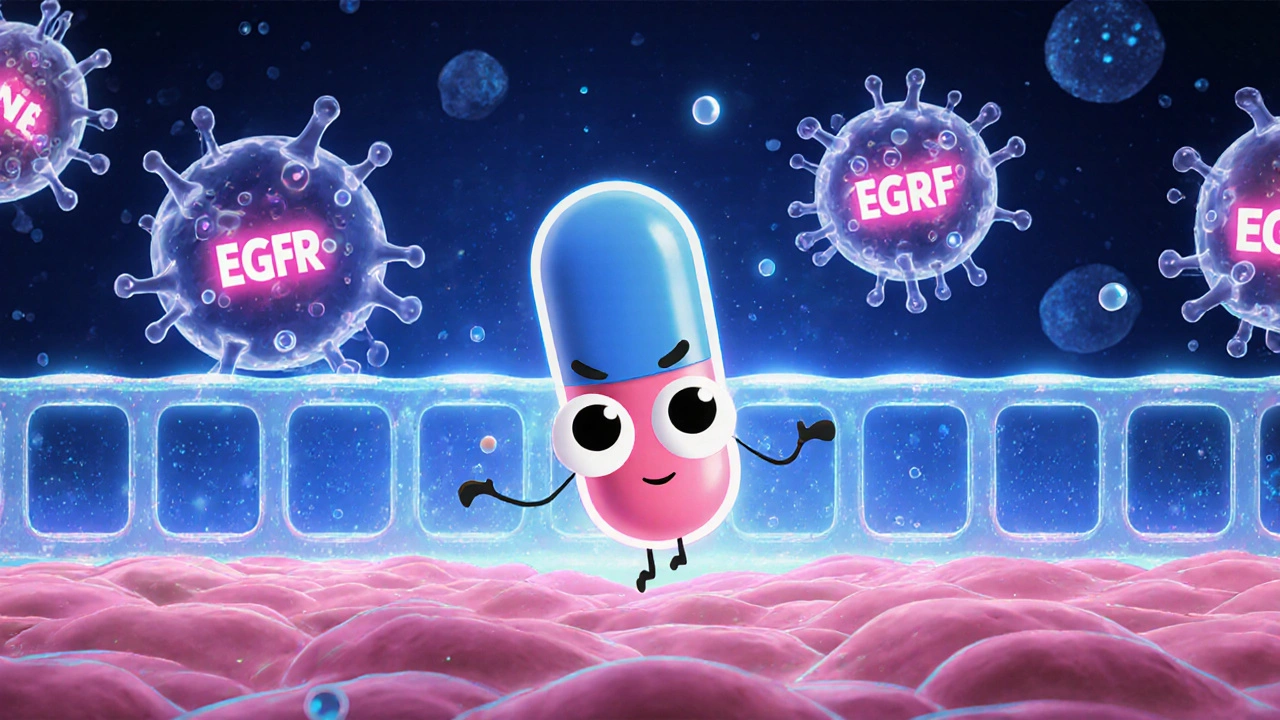
A detailed case study shows how high‑dose Erlotinib can control leptomeningeal metastases in EGFR‑mutated lung cancer, covering pharmacology, outcomes, safety, and comparisons with other TKIs.