When your body overreacts to injury or disease, corticosteroids, a class of powerful anti-inflammatory drugs that mimic hormones naturally made by your adrenal glands. Also known as steroids, they’re not the same as the muscle-building kind you hear about in sports. These are prescription medicines used to calm down runaway immune responses—like in asthma, rheumatoid arthritis, or severe skin conditions. They work by turning down the volume on your body’s alarm system, reducing swelling, redness, and pain. But they’re not harmless. Even short-term use can cause mood swings or trouble sleeping; long-term use brings bigger risks like bone thinning or high blood sugar.
Doctors reach for corticosteroids when other treatments don’t cut it. You might get them as a pill, an injection, a cream, or an inhaler—depending on what’s wrong. For example, if you have eczema, a topical steroid cream can clear up a flare-up faster than any moisturizer. If you’re having an asthma attack, an inhaler with corticosteroids helps keep your airways open over time. But here’s the catch: they don’t fix the root cause. They just silence the symptoms. That’s why they’re often paired with other treatments, like allergy meds or physical therapy. And because your body can get used to them, stopping suddenly can backfire. That’s why tapering off under a doctor’s watch is non-negotiable.
Related to corticosteroids are other immune system modulators, drugs that adjust how your immune system behaves without fully suppressing it. These include biologics and DMARDs, often used in autoimmune diseases like lupus or Crohn’s. Then there’s inflammation, the body’s natural response to harm, which corticosteroids aim to control. Too much inflammation leads to chronic pain and tissue damage. That’s why these drugs are so widely used—but also why they’re not a first-line fix for every ache or itch. And let’s not forget side effects, the trade-off for getting quick relief. Weight gain, thinning skin, cataracts, and increased infection risk are real concerns. That’s why knowing when to use them—and when to avoid them—is just as important as knowing how to take them.
The posts below cover real cases where corticosteroids come into play, whether as the main treatment or part of a bigger plan. You’ll find comparisons with alternatives, tips on managing side effects, and insights into how they interact with other meds. No fluff. Just what you need to make smarter choices about your health.
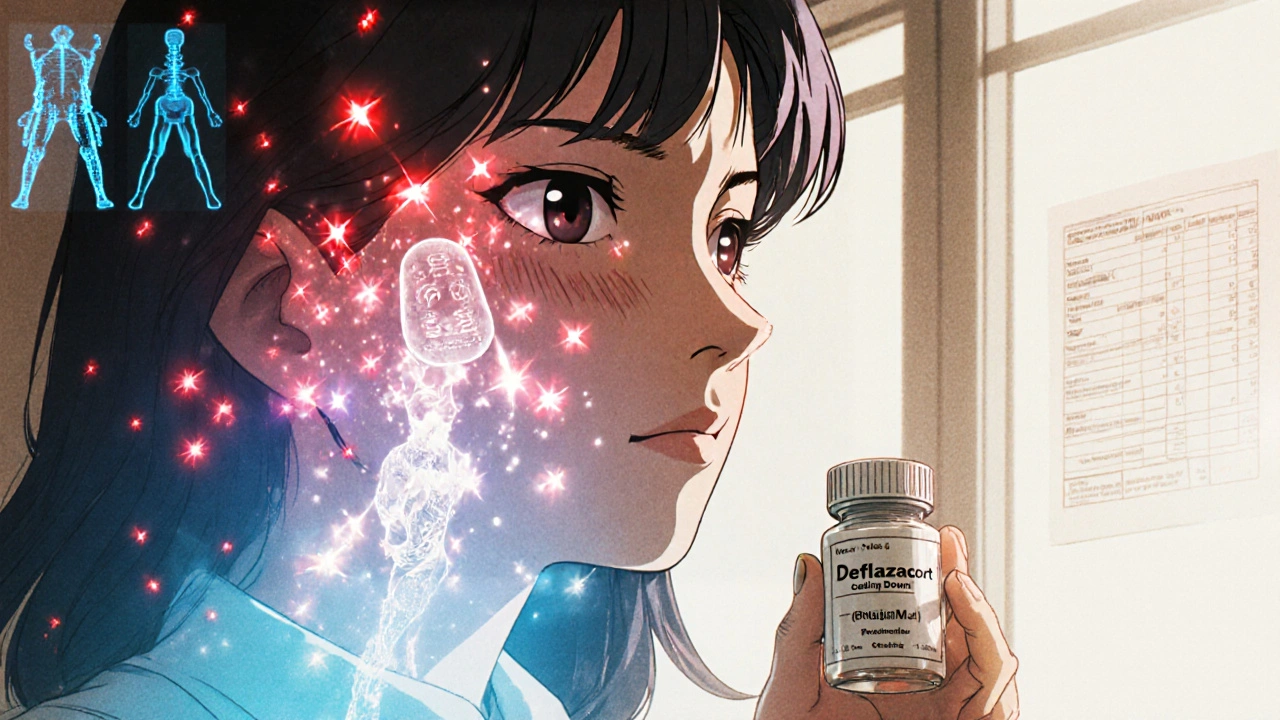
Deflazacort offers a potentially safer alternative to prednisone for lupus patients, with fewer metabolic side effects like weight gain and blood sugar spikes. Learn how it works, who benefits most, and how to talk to your doctor about switching.