When you mix alcohol interaction, the way alcohol affects how your body handles medications. Also known as drug-alcohol interactions, it’s not just about getting drunk—it’s about whether your medicine still works, or if it turns risky. This isn’t theoretical. People on blood thinners like warfarin have ended up in the ER after just one drink because alcohol changes how their body processes the drug. The same goes for antibiotics, antidepressants, painkillers, and even sleep aids. Your liver treats alcohol and most medications the same way: as something to break down. When both are in there at once, things get backed up—or worse, they clash.
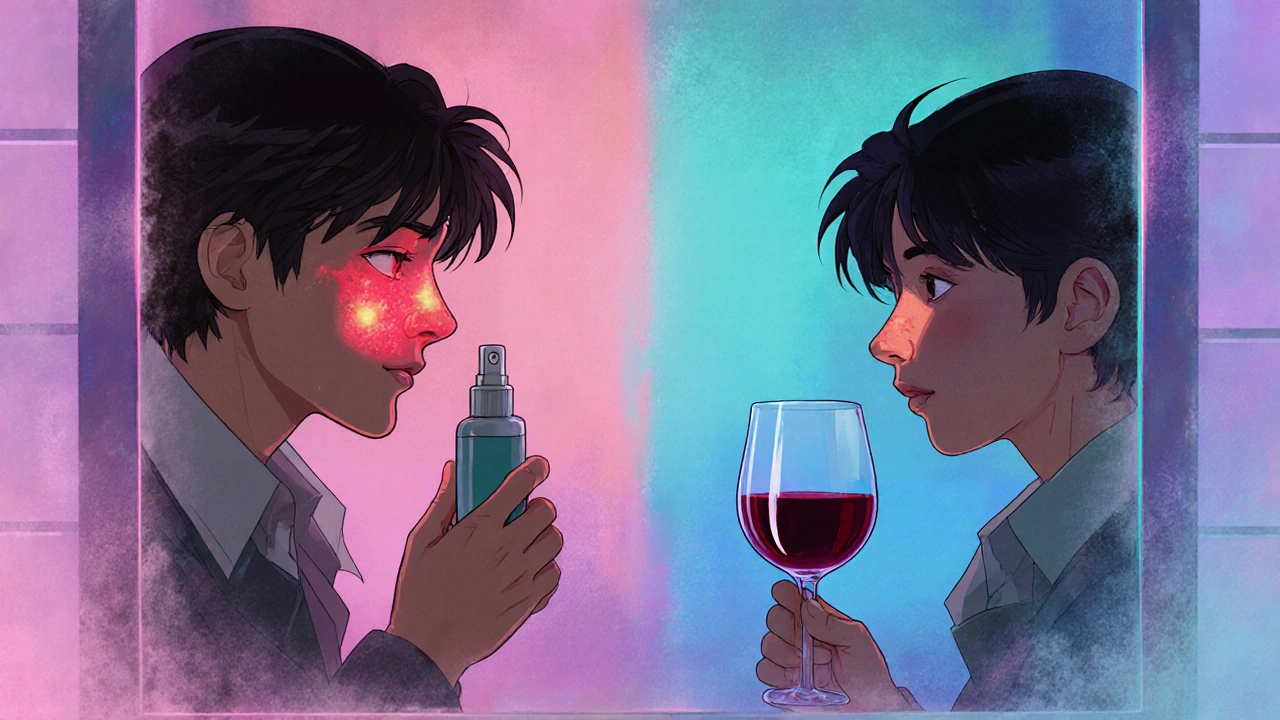
alcohol and warfarin, a dangerous combo that can spike your INR levels and cause internal bleeding. One study tracked patients on warfarin who drank even one alcoholic drink a day. Their INR levels jumped unpredictably, making them far more likely to bleed out from a minor cut or bruise. It’s not just warfarin, either. NSAIDs like ibuprofen? Add alcohol, and you’re asking for stomach ulcers. Antidepressants? Alcohol can make you feel sadder, sleepier, or even dizzy enough to fall. And if you’re on antibiotics like metronidazole or tinidazole, drinking can trigger vomiting, racing heart, and flushing—like your body’s screaming at you to stop.
INR levels, a measure of how long your blood takes to clot, and alcohol can throw them off balance. Doctors monitor INR closely for people on blood thinners because it’s the only real way to know if the dose is right. Alcohol doesn’t just change the number—it makes it unstable. One night of drinking might send your INR sky-high. Two days later, it could crash. That’s why some doctors tell patients to avoid alcohol entirely. Others say one drink occasionally might be okay—if you’re consistent, your INR is stable, and you check in with your provider. But there’s no universal green light.
It’s not just about the big stuff. Even over-the-counter meds like cold pills or sleep aids can turn risky with alcohol. Tylenol? Safe in small doses—but with alcohol, it can damage your liver. Benadryl? Makes you sleepy. Add alcohol? You might not wake up. And if you’re on anything for anxiety, seizures, or chronic pain, alcohol doesn’t just make side effects worse—it can cancel out the medicine’s whole purpose.
You don’t need to be a heavy drinker for this to matter. A glass of wine with dinner. A beer after work. A shot at a party. All of it counts. And if you’re over 65, your body clears alcohol slower, so the risk goes up even more. That’s why so many of the posts here focus on elderly patients, blood thinners, and hidden dangers in everyday meds. This isn’t about fear. It’s about awareness. You’re not being paranoid if you check before you drink. You’re being smart.
Below, you’ll find real stories and clear guides from people who’ve been there—whether it’s understanding why alcohol messes with your INR, how to read labels on OTC meds, or what to do if you accidentally mixed alcohol with your prescription. No fluff. No jargon. Just what you need to know to stay safe, whether you’re managing a chronic condition or just taking meds for a short time.
Fluticasone and alcohol don't interact directly, but alcohol can worsen allergy and asthma symptoms by triggering inflammation and drying out nasal passages. Learn how drinking affects your treatment and what to do instead.