When you take warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, artificial heart valves, or a history of deep vein thrombosis. Also known as Coumadin, it works by blocking vitamin K, which your body needs to form clots. But mixing it with alcohol, a substance that affects liver function and how your body processes medications can turn a safe treatment into a serious health risk.
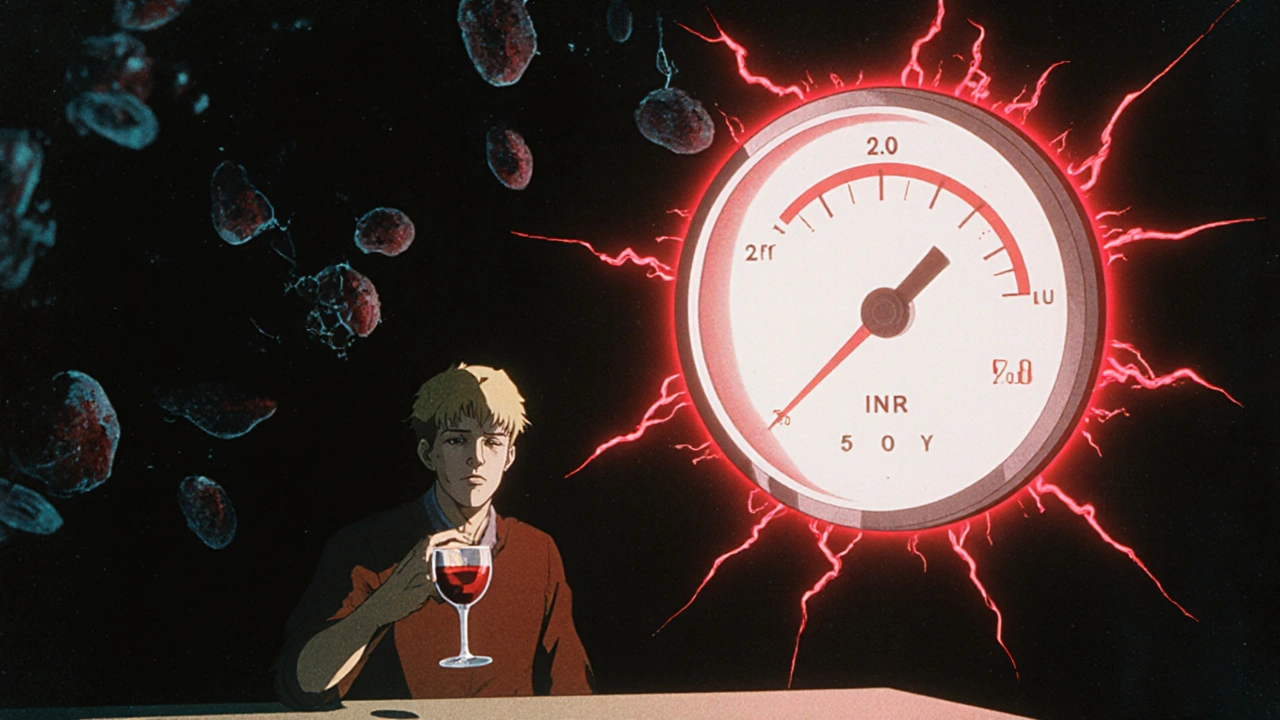
The alcohol and warfarin combo doesn’t just raise your INR — it can cause unpredictable spikes that lead to internal bleeding, bruising, or even stroke. Your liver is responsible for breaking down both alcohol and warfarin. When you drink, especially heavily or regularly, your liver gets overwhelmed. This slows down how fast warfarin leaves your body, making it build up to dangerous levels. Even a single drink can throw off your dosing if you’re not consistent. Studies show people who drink more than three alcoholic drinks a week have a 30% higher chance of serious bleeding compared to non-drinkers on warfarin.
It’s not just about how much you drink — it’s about consistency. If you usually have one beer with dinner and suddenly have three, your INR could jump overnight. If you quit drinking cold turkey after drinking regularly for months, your warfarin levels could drop too low, raising your risk of clots. The same goes for switching between beer, wine, and spirits — your body doesn’t care what kind of alcohol it is. What matters is the total amount and how often you take it.
Some people think a glass of wine is fine because it’s "healthy." But for someone on warfarin, there’s no safe level that’s guaranteed to be harmless. The real issue isn’t wine or vodka — it’s the liver metabolism, the process that determines how fast your body clears drugs from your system. Alcohol changes this process, and since warfarin has such a narrow safety window, even small changes can be dangerous. That’s why doctors often tell patients to avoid alcohol entirely — not because it’s always deadly, but because the risk isn’t worth it.
You’re not alone if you’re struggling with this. Many people on warfarin want to keep enjoying social drinks, but don’t know how to do it safely. The key is honesty with your care team. Tell them exactly how much you drink — even if it’s just on weekends. They can adjust your dose, monitor your INR more closely, or suggest alternatives if needed. Never stop or change your warfarin dose on your own, and never assume a drink won’t affect you just because it worked fine last time.
Below, you’ll find real patient experiences, expert advice, and clear comparisons on how alcohol interacts with blood thinners like warfarin — and what to do if you’ve already had a drink. These aren’t theoretical warnings. They’re lessons from people who’ve been there, and the doctors who help them get back on track.
Alcohol can cause dangerous INR fluctuations in people taking warfarin, increasing bleeding risk. Learn how drinking affects your blood thinning levels, what's safe, and what warning signs to watch for.